Abstract
INTRODUCTION
Trauma is the fifth principal cause of death in Singapore, with traumatic brain injury (TBI) being the leading specific subordinate cause.
METHODS
This study was an eight-year retrospective review of the demographic profiles of patients with severe TBI who were admitted to the neurointensive care unit (NICU) of the National Neuroscience Institute at Tan Tock Seng Hospital, Singapore, between 2004 and 2011.
RESULTS
A total of 780 TBI patients were admitted during the study period; 365 (46.8%) patients sustained severe TBI (i.e. Glasgow Coma Scale score ≤ 8), with the majority (75.3%) being male. The ages of patients with severe TBI ranged from 14–93 years, with a bimodal preponderance in young adults (i.e. 21–40 years) and elderly persons (i.e. > 60 years). Motor vehicle accidents (48.8%) and falls (42.5%) were the main mechanisms of injury. Invasive line monitoring was frequently employed; invasive arterial blood pressure monitoring and central venous pressure monitoring were used in 81.6% and 60.0% of the patients, respectively, while intracranial pressure (ICP) measurement was required in 47.4% of the patients. The use of tiered therapy to control ICP (e.g. sedation, osmotherapy, cerebrospinal fluid drainage, moderate hyperventilation and barbiturate-induced coma) converged with international practices.
CONCLUSION
The high-risk groups for severe TBI were young adults and elderly persons involved in motor vehicle accidents and falls, respectively. In the NICU, the care of patients with severe TBI requires heavy utilisation of resources. The healthcare burden of these patients extends beyond the acute critical care phase.
INTRODUCTION
Severe traumatic brain injury (TBI) is a major health and socioeconomic problem globally.(1,2) TBI can be defined as a trauma-induced physiologic disruption or insult to the brain from an external mechanical force. Outcomes of TBI are diverse and can include physical, cognitive and social problems, with the majority of patients facing significant mortality and morbidity.
Country-based estimates of TBI incidence range from 108–332 new hospitalised cases per 100,000 population/year; differences in reported incidences may be due to variations in the definition of TBI.(3) In the United States, TBI accounts for approximately 40% of all deaths from acute injuries and approximately 200,000 victims of TBI require hospitalised care annually.(4) In Singapore, ‘external causes of morbidity and mortality’ (ICD10: V01-Y89) is the fifth principal cause of death,(5) with TBI being the leading specific subordinate cause. It is difficult to ascertain the full socioeconomic cost of TBI, but any financial estimate should include the cost of life-saving neurosurgical treatment and/or neurocritical care in the acute phase, other ongoing medical expenses (e.g. ambulatory and rehabilitation care), and the loss of potential income for the patient and caregiver.(4,6) In other words, TBI is a major public health concern. The objective of this study was to delineate the demographic profile of patients with severe TBI in the Singapore context, since this information has major implications in the management of TBI patients as well as the allocation and utilisation of scarce local healthcare resources. Such information would also be useful for devising prevention programmes in the local community. Importantly, the present study also highlights the impact of falls on the elderly.
METHODS
This retrospective study was approved by the Institutional Review Board of the National Healthcare Group, Singapore. The data of patients who were admitted to the neurointensive care unit (NICU) at the National Neuroscience Institute, Tan Tock Seng Hospital, Singapore, between 2004 and 2011 was obtained from a prospectively maintained TBI database. The data of patients with severe TBI was subsequently extracted for analysis. Patients who had a Glasgow Coma Scale (GCS) score of ≤ 8 following nonsurgical resuscitation (i.e. airway management, haemodynamic and volume support, electrolyte correction, and osmotic therapy) were considered to have severe TBI.
Data on patient demographics, the mechanism of injury leading to severe TBI, and the types of monitoring and treatment administered to reduce increased intracranial pressure (ICP) was collected and analysed. The data on the mechanism of injury was obtained from patient records from the emergency department, ambulance pre-hospital care records and/or the patient’s history as reported by family members or witnesses. Death/mortality was evaluated based on the assessment of the patients’ condition (i.e. dead or alive) at the end of their hospital stay. High-risk activities were defined as activities that resulted in high-impact falls (i.e. from a height ≥ 2 m), motor vehicle accidents (MVAs), activities involving assaults and sports-related activities. Elderly patients were defined as patients aged > 60 years.
Statistical analysis was performed using IBM SPSS Statistics version 20.0 for Windows (IBM Corp, Armonk, NY, USA). Chi-square test was used to evaluate the association between age group/gender and the outcome of patients with severe TBI. Logistic regression analysis predicting falls from a height < 2 m and high-risk activities was used to estimate the odds ratios, 95% confidence intervals (CIs) and p-values of the predictor variables, after controlling for age group, gender and nationality. All statistical tests were two-sided and a p-value < 0.05 was considered to be statistically significant.
RESULTS
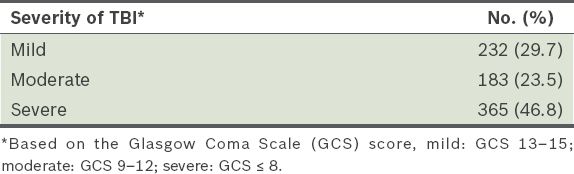
Over the eight-year period from January 2004 to December 2011, 780 patients were admitted to the NICU with TBI of various levels of severity (
Table I
Traumatic brain injury (TBI) patients, classified by severity (n = 780).
The demographic data of the 365 patients with severe TBI is summarised in
Table II
Demographic data of severe traumatic brain injury patients (n = 365).
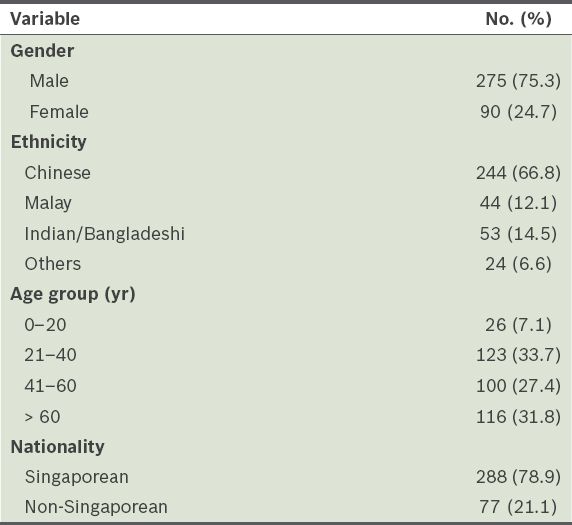
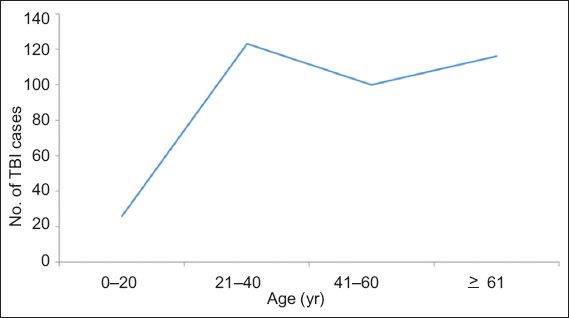
Fig. 1
Line graph shows the bimodal age distribution of the patients with severe traumatic brain injury (TBI; n = 365).
Details of the injuries, such as the mechanism of injury, are presented in
Table III
Details of the injury sustained by patients with severe traumatic brain injury (n = 365).
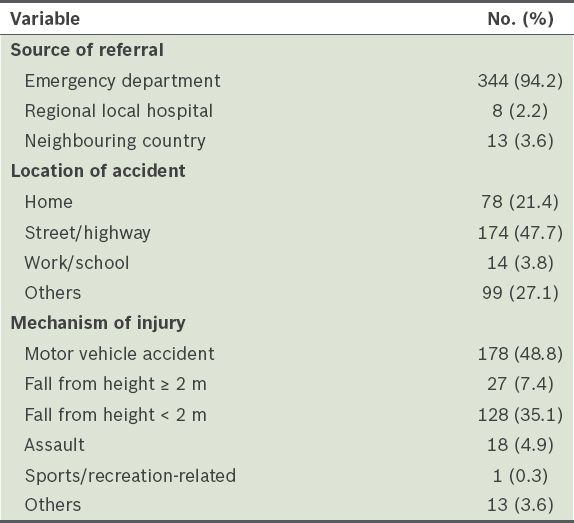
Table IV
Mechanism of injury among the patients with severe traumatic brain injury, according to age group (n = 365).
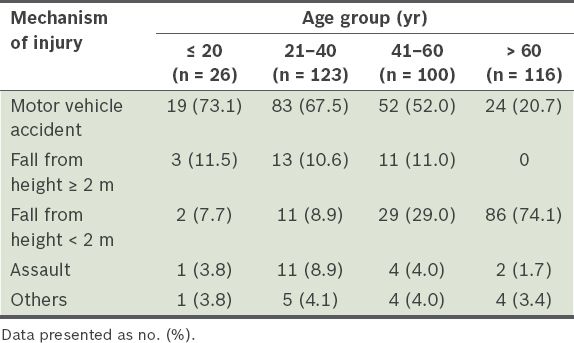
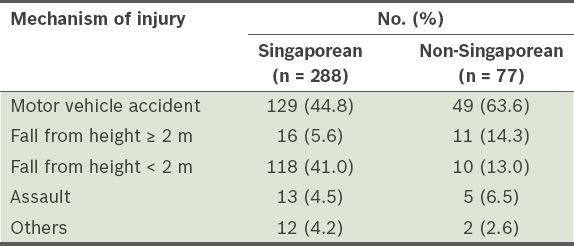
Table V
Mechanism of injury among the patients with severe traumatic brain injury, according to nationality (n = 365).
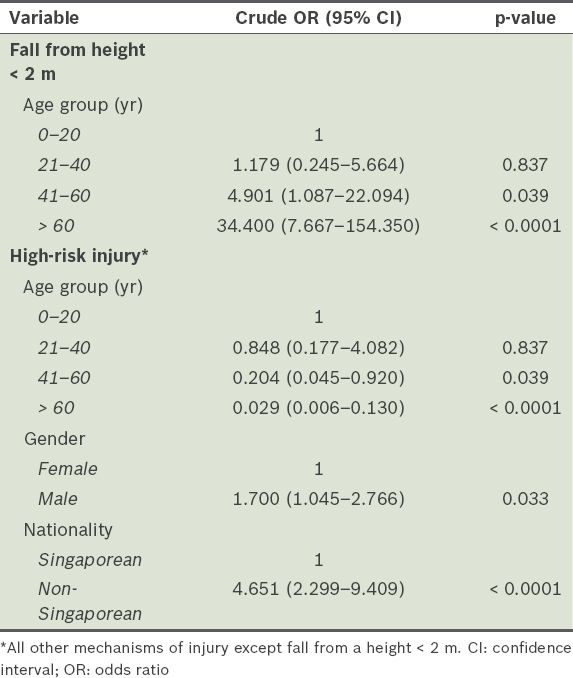
Age was found to be an independent predictor of severe TBI after a fall from a height < 2 m. Elderly patients (i.e. aged > 60 years) were approximately 34 times more likely to sustain severe TBI after a fall from a height < 2 m, as compared to patients in the younger age groups (95% CI 7.667–154.350, p < 0.0001) (
Table VI
Results of logistic regression predicting the mechanism of injury among patients with severe traumatic brain injury.
A comparison of the outcomes of severe TBI between the age groups revealed that the elderly were more likely to experience a poorer outcome as compared to patients aged ≤ 60 years (
Table VII
Comparison of the outcomes of severe traumatic brain injury, according to age group and gender.
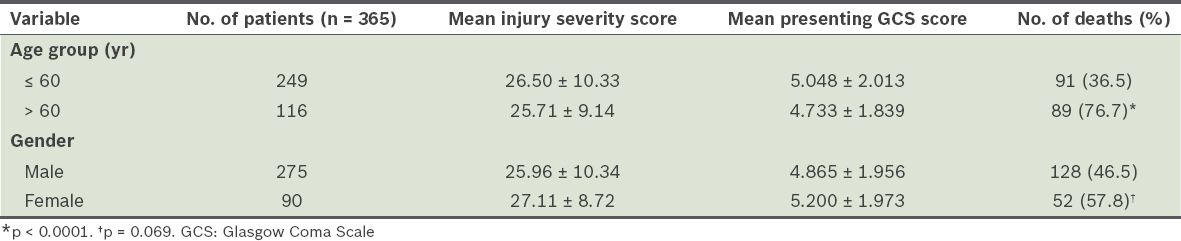
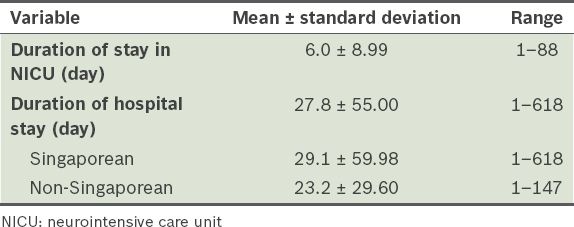
Table VIII
Length of stay of patients with severe traumatic brain injury.
The monitoring modalities that were applied to the 365 patients with severe TBI are summarised in
Table IX
Monitoring modalities applied to patients with severe traumatic brain injury (n = 365).
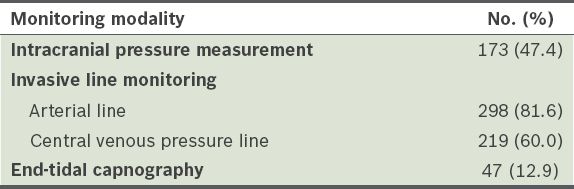
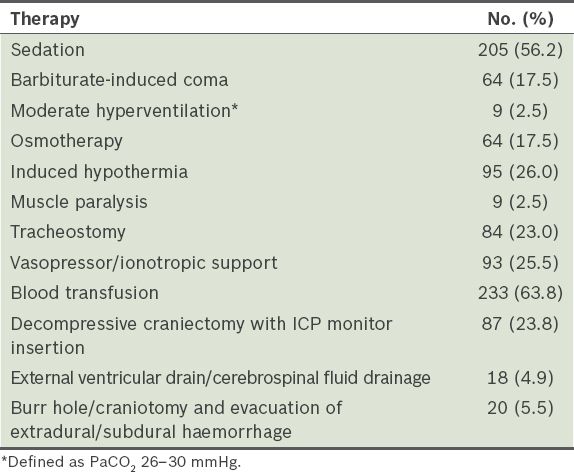
Table X
Incidence of tiered therapy used for raised intracranial pressure (ICP) (n = 365).
DISCUSSION
In the present study, 415 (53.2%) of the 780 patients with TBI who were admitted to the NICU had mild-to-moderate TBI. This indicates that a substantive proportion of the NICU workload was dedicated to patients who were not suffering from severe TBI. Patients with non-severe TBI still require management in the NICU, especially those who are at risk of acute deterioration, such as elderly patients.(7,8) Greater attention to this group of patients is warranted and the close neurological monitoring offered by the NICU plays an important role in the management of TBI in such cases.
The incidence of severe TBI had a bimodal age distribution in this study; the first peak was observed in the young adult age group (i.e. 21–40 years), while the second peak was observed in the elderly age group (i.e. > 60 years). Overall, male patients were found to be approximately 3–4 times more likely to sustain severe TBI than female patients (75.3% vs. 24.7%). The difference in the incidence of severe TBI among the different age groups and genders may demonstrate differing predisposing factors.(9,10) This is evidenced partly by the fact that young males are substantially overrepresented in the severe TBI cases resulting from high-risk activities such as MVAs and assaults. Conversely, the elderly formed the bulk of severe TBI cases that resulted from low-height/impact falls (i.e. falls from a height < 2 m).
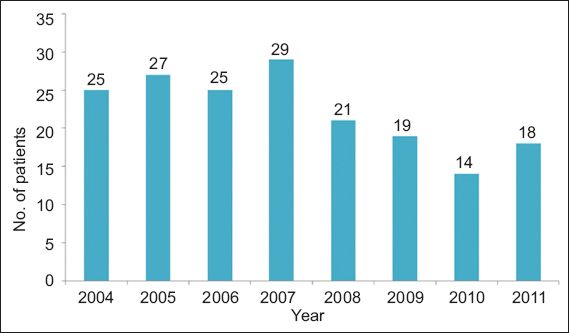
A previous local study reported a decrease in MVA-related severe TBI cases admitted to the NICU of the National Neuroscience Institute at Tan Tock Seng Hospital, Singapore, in the years leading up to 2004.(11) The present study appears to show that the downward trend at the same NICU continued during the years of 2005–2011 (
Fig. 2
Bar graph shows the annual number of patients admitted to the neurointensive care unit of the National Neuroscience Institute at Tan Tock Seng Hospital, Singapore, with traumatic brain injury caused by motor vehicular accidents (2004–2011).
Severe TBI being common among young adults is a major public health concern, as this would result in a reduced number of productive life years due to death or disability, inflicting high costs on society. The observation that a large majority of such injuries and fatalities occur among males in their economic prime is also reflected in many other studies.(13,14)
Depending on the underlying mechanism of trauma, 70% of patients with TBI may have associated polytrauma, fractures, cardiopulmonary or visceral injuries, spinal cord injuries, peripheral nerve injuries and limb amputations.(15) These conditions may aggravate neurodisability due to craniocerebral trauma. Survivors of severe TBI have a marked reduction in life expectancy, dying two times faster than the general population. Furthermore, survivors of severe TBI face the need for prolonged care and rehabilitation, and have consequent long-term physical, cognitive and psychological disorders that affect their independence, relationships and employment.(16,17)
Similar to most developed countries, Singapore has an ageing population that has given rise to a new cohort of elderly persons who sustain significant TBI from fairly low-height falls (i.e. falls from a height < 2 m). The bimodal age distribution observed in the present study, with peaks occurring at the young adult (aged 21–40 years) and elderly age groups, has also been reported in other studies.(3,6,18) In many high-income countries, comprehensive traffic safety legislation, preventive measures and educational campaigns have limited the rise in the incidence of transport-related TBI.(11) However, the incidence of TBI caused by low-height falls is increasing as the population ages, resulting in a rise in the median age of the TBI population. In this study, the elderly formed a large part of the severe TBI cohort, with most (74.1%) of the severe TBI cases caused by falls from a height < 2 m. Compared to their younger counterparts, elderly persons have a greater fall propensity due to multifactorial causes. These causes include: (a) intrinsic patient factors, such as cognitive/mental or musculoskeletal disabilities, cardiac arrhythmias and postural hypotension, and visual, proprioceptive or balance impairments; (b) extrinsic environmental factors, such as poor lighting or glare, furniture hazards and uneven flooring; and (c) social/behavioural factors, such as living alone and poor safety awareness.(19) Consequently, there may be a pattern shift in the types of TBI seen, with focal intraparenchymal or subdural haematomas (resulting from low-height falls among older patients) gaining prominence over diffuse injuries (resulting from high-velocity accidents among younger patients).
Although many of the severe TBI cases among elderly patients in this study were caused by low-height falls with less severe ISS, these patients presented with a much lower GCS score and higher mortality outcome as compared to patients from the younger age group (
We also found that the home was the second most common (21.4%) location of accidents that resulted in severe TBI (
As of December 2012, the foreign workforce in Singapore, who are mainly from Southeast Asian countries, the Indian subcontinent and China, amounts to 1.27 million.(21) Many of these workers are involved in industrial, building construction and shipbuilding/repair activities, which are inherently high-risk. In the present study, 21.1% of the patients with severe TBI were non-Singaporean (i.e. foreign workers). Foreign workers were more likely to suffer from severe TBI that was associated with high-risk activities, with MVAs and falls from a height ≥ 2 m forming the top two causes (
The vast majority of the patients with severe TBI had invasive arterial line monitoring in the NICU. The use of arterial line monitoring is essential, as tight regulation of the patient’s mean arterial blood pressure (MAP) is necessary in the setting of severe TBI. In addition, arterial line monitoring allows the derivation of cerebral perfusion pressure (i.e. MAP – ICP) and provides access for arterial blood samples to be taken. Central venous access and pressure monitoring was also widely employed among the patients with severe TBI. Thus, invasive line monitoring can be regarded as part of the standard monitoring of salvageable patients with severe TBI;(24) it is possible that the utility of end-tidal carbon dioxide monitoring needs greater recognition and application in our unit.
The incidence of the use of tiered therapy (e.g. sedation, osmotherapy with mannitol, cerebrospinal fluid drainage, moderate hyperventilation and barbiturate-induced coma) in the present study to control ICP converged with international practices.(25) The majority (56.2%) of the patients with severe TBI required hypnotic pharmacotherapy (i.e. the use of midazolam, propofol and/or fentanyl) for sedation in our NICU. Sedation is employed mainly for control of ICP, facilitation of mechanical ventilation or endotracheal tube tolerance, or blood pressure control. Patients with severe TBI who have a low post-resuscitation GCS score may not require further sedation. Hyperventilation should only be used as an acute temporising measure in the context of life-threatening and refractory intracranial hypertension, due to the potential for exacerbating cerebral ischaemia;(24) the judicious use of moderate hyperventilation, defined as PaCO2 26–30 mmHg, was reserved for only a small proportion (< 3%) of the patients in the present study.
The benefit of decompressive craniectomy was recently brought into question.(26) The use of early craniectomy in diffuse traumatic brain injury (DECRA) effectively decreases ICP and the length of stay in the ICU, but increases the proportion of patients with an unfavourable functional outcome (i.e. worse scores on the Extended Glasgow Outcome Scale) as compared to patients who receive standard care. In response to the perceived limitations of the DECRA trial,(27) the Randomised Evaluation of Surgery with Craniectomy for Uncontrollable Elevation of Intra-Cranial Pressure study is currently in progress.
To conclude, TBI has often been described as a silent epidemic. The results of the present study are consistent with other reports that document the greater frequency of MVA-related TBI among younger individuals and fall-related TBI among the elderly. The second peak in the incidence of severe TBI was from patients aged > 60 years; this group of patients, which accounted for 31.8% of all patients with severe TBI in the present study, were also found to have poorer functional outcome even though they had seemingly less severe ISS at presentation. Locally, fall-related TBI among the elderly may be expected to further increase in view of Singapore’s ageing population.
TBI is a prime contributor to the global burden of disease and disability. It continues to be an exigent domain of healthcare, particularly in developed, high-income countries. The management of TBI precedes and goes beyond the NICU, hence should be viewed as a continuum from pre-hospital emergency systems to community-based rehabilitation care. Prevention requires a multipronged, tailored, preventive strategy that involves educating at-risk populations in society (e.g. the young, elderly and persons from high-risk occupational groups) as well as relevant legislation, engagement and enforcement.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to Karen Go and Crystal Raphael, Trauma Coordinators from the Department of General Surgery, Tan Tock Seng Hospital, Singapore.


