Abstract
INTRODUCTION
General anaesthesia is associated with higher maternal morbidity and mortality when compared with regional anaesthesia, related mainly to failure of intubation, hypoxia and aspiration. The aim of this retrospective review was to define the incidence of failed and difficult intubation in parturients undergoing general anaesthesia for Caesarean delivery at a high-volume obstetric hospital in Singapore.
METHODS
All parturients who underwent Caesarean delivery under general anaesthesia from 2013 to 2016 were identified and their medical records were reviewed to extract pertinent data. Difficult intubation was defined as ‘requiring more than one attempt at intubation or documented as such, based on the opinion of the anaesthetist’. A failed intubation was defined as ‘inability to intubate the trachea, with subsequent abandonment of intubation as a means of airway management’.
RESULTS
Records of 660 Caesarean sections under general anaesthesia were extracted. The mean age of the parturients was 32.1 ± 5.5 years and the median body mass index was 27.5 (interquartile range 24.6–31.1) kg/m2. Rapid sequence induction with cricoid pressure was employed for all patients, with thiopentone and succinylcholine being administered for 91.2% and 98.1% of patients, respectively. There were 33 difficult intubations among 660 patients, yielding an incidence of 5.0%. Junior trainees performed about 90% of all intubations and 28 (84.8%) out of 33 difficult intubations. Repeat intubations were performed by senior residents/fellows (57.1%) and consultants (14.3%). No instance of failed intubation was reported.
CONCLUSION
The local incidence of difficult obstetric intubation was one in 20. No failure of intubation was observed.
INTRODUCTION
Studies on obstetric mortality suggest that regional anaesthesia is 2–16 times safer than general anaesthesia for obstetric patients.(1) This may have contributed to the observed decline in general anaesthesia for Caesarean deliveries in the last decades.(2,3) General anaesthesia is now employed mainly as a rescue technique for a failed regional block(4) or, in emergencies, when prompt delivery is mandated.(5,6) Serious maternal complications associated with general anaesthesia are related to failure of intubation, with ensuing maternal hypoxia, aspiration or even death.(1,7) Physiological and anatomical changes in pregnancy contribute to difficult laryngoscopy and visualisation of the larynx. Increased oxygen consumption and a concomitant decrease in functional residual capacity compound the problem by causing rapid desaturation and a reduced tolerance for apnoea during induction.
The incidence of failed intubation in the obstetric population has been estimated to be eight times higher than that in the general surgical population,(8) and this has not changed significantly through the decades.(9,10) In a review of failed obstetric intubations reported since the 1970s, the incidence of failed intubation was noted to be stable at 2.3 cases per 1,000 anaesthetics for Caesarean delivery, or 1:443.(9) The probability of maternal death associated with a failed intubation was high at 1:100.(9) There is no recent local data on the incidence of failed obstetric intubation. A previous local study conducted more than 20 years ago had estimated the incidence of difficult intubation to be 6:277.(11) The purpose of this retrospective review was to define the incidence of failed and difficult intubation in parturients receiving general anaesthesia for Caesarean delivery at our high-volume obstetric hospital in Singapore. Results from this review could provide insights into the adequacy of existing faculty supervision and trainee performance when administering general anaesthesia for Caesarean delivery.(12)
METHODS
This study was conducted at KK Women’s and Children’s Hospital, Singapore’s largest tertiary referral centre for obstetrics, gynaecology, paediatrics and neonatology. The 830-bed hospital provides care for about 11,000 deliveries a year, with a stable Caesarean section rate of 28%. The institution is also accredited by the Accreditation Council for Graduate Medical Education International for specialist training in obstetrics and gynaecology, paediatrics, and anaesthesiology. In the five-year anaesthesiology training programme, clinical experience is gained systematically through a block rotation system, with graduated increase in responsibility at each level. Junior residents embark on the basic obstetric anaesthesia module in their second and third years of training, completing the advanced obstetric anaesthesia module during their senior residency training. Departmental guidelines and standards are available to guide clinical care and the supervision of trainees or residents. Anaesthesia care for labour epidurals and Caesarean deliveries is provided round the clock by a team comprising residents and resident physicians or fellows, led by a consultant anaesthetist during office hours or a specialist of at least staff registrar grade after hours. As a rule, all Caesarean deliveries under general anaesthesia are covered directly by a consultant anaesthetist during office hours and a specialist of at least staff registrar grade after office hours.
For the study, all parturients who underwent Caesarean delivery under general anaesthesia during the study period – 1 January 2013 to 31 December 2016 – were identified from the anaesthesia department database and their medical records were reviewed to extract the relevant data. The hospital delivery database was also accessed to retrieve the total number of Caesarean deliveries for the study period. Ethics approval was sought from the institutional review board (CIRB 2015/2746) and waiver of informed consent was granted.
Demographic and obstetric data collected included patient age, gravidity and parity, gestational age at delivery, body mass index, the American Society of Anesthesiologists (ASA) physical status, indication for general anaesthesia and priority classification of Caesarean sections. For the latter, our institution has adopted Lucas’ classification for urgency of a Caesarean section.(13)
Anaesthetic data included preoperative airway assessment, induction technique and drugs, level of experience of providers of intubation (where possible), number of intubation attempts and success at intubation, Cormack-Lehane view at each attempt, use of airway adjuncts and associated airway complications. A potential difficult airway was considered ‘to be anticipated’ if the relevant tick box for predicted difficult airway on the anaesthetic chart was checked during pre-anaesthesia assessment. For the purpose of the study, difficult intubation was defined as ‘requiring more than one attempt at intubation or documented as such, based on the opinion of the anaesthetist’. A failed intubation was defined as ‘inability to intubate the trachea, with subsequent abandonment of intubation as a means of airway management’. Data on difficult and failed intubations was cross-checked against the database for critical incidents and adverse events to ensure completeness and accuracy of data.
Statistical analysis was performed using IBM SPSS Statistics for Windows version 19.0 (IBM Corp, Armonk, NY, USA). Data was presented as mean ± standard deviation, median (interquartile range [IQR]) or count (%), as appropriate. Categorical data and proportions were compared using Pearson’s chi-square test or Fisher’s exact test, where appropriate. A p-value < 0.05 was considered to be statistically significant. Patients with missing or incomplete data were excluded from the subgroup analysis.
RESULTS
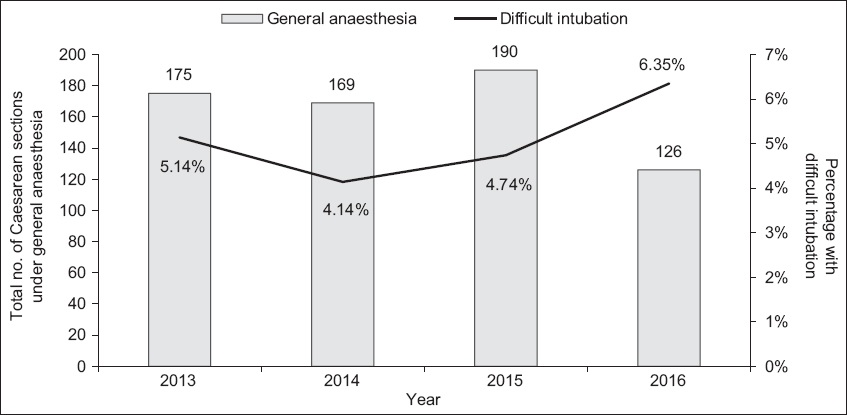
A total of 14,545 Caesarean sections were recorded over the four-year study period, of which 9,000 (61.9%) were elective. Overall, 660 (4.5%) Caesarean sections were performed under general anaesthesia, with 518 (78.5%) procedures being conducted as emergencies. The yearly distribution of difficult intubations among Caesarean sections performed under general anaesthesia is shown in
Fig. 1
Chart shows the incidence of difficult intubations among Caesarean sections performed under general anaesthesia.
The indications for general anaesthesia are shown in
Table I
Indications for general anaesthesia among obstetric patients undergoing Caesarean sections (n = 660).
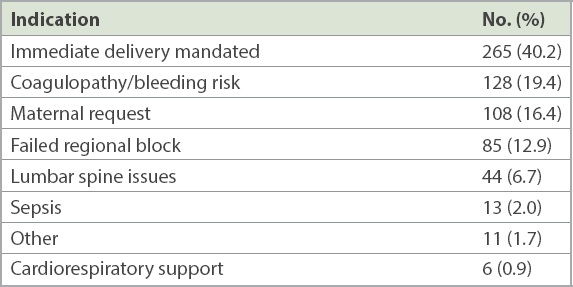
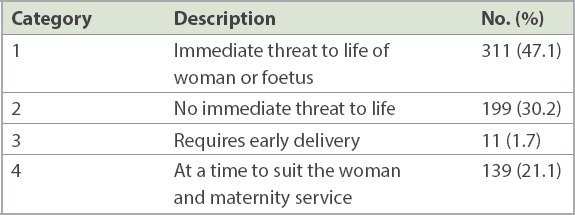
Table II
Priority classification of Caesarean sections performed under general anaesthesia (n = 660).
Thiopentone was used for induction of general anaesthesia in 91.2% of patients, with a mean dose of 5.1 ± 1.2 mg/kg. Some (8.3%) patients were induced with propofol (mean dose 2.0 ± 0.8 mg/kg). The remaining 0.5% of patients were induced with ketamine. Succinylcholine was the muscle relaxant of choice for 98.1% of patients (mean dose 1.5 ± 0.3 mg/kg). Rocuronium was used for the remaining patients (mean dose 0.8 ± 0.5 mg/kg). Except for four patients with missing induction data, all patients had rapid sequence induction and consistent use of cricoid pressure to facilitate tracheal intubation. Cricoid pressure was released transiently in 29 patients to facilitate laryngoscopy. All intubations were first attempted by a junior resident for 90.1% of patients, by a senior resident or fellow for 8.5% of patients and by a consultant for only 1.4% of patients. Almost half of the intubations were aided by direct laryngoscopy using a Macintosh blade (Armstrong Medical Industries Inc, Lincolnshire, IL, USA), while the rest were aided by a C-MAC® video laryngoscope (Karl-Storz, Tuttlingen, Germany). External laryngeal pressure was exerted in 8.6% of intubations. The gum-elastic bougie was used to facilitate tube placement for 29.2% of patients, while a preloaded stylet was used even less frequently – in only 6.0% of patients.
Overall, 33 (1:20 or 5.0%) of 660 patients fulfilled the study criteria for difficult intubation. None of the patients had a failed intubation. There was no record of the need for insertion of a laryngeal mask airway, bronchoscopic-assisted intubation or front-of-neck access.
Table III
Cormack and Lehane grades based on laryngoscopy.
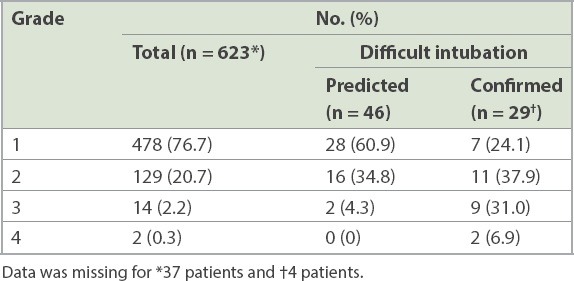
Table IV
Difficult intubations against Cormack-Lehane grades based on laryngoscopy.
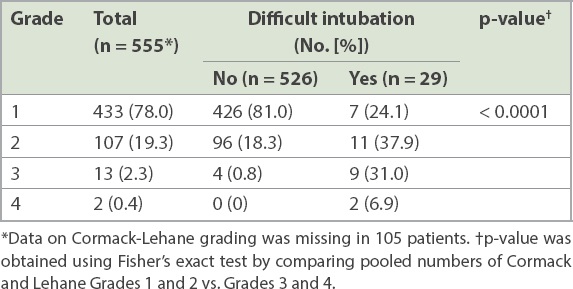
In our study, 28 (84.8%) of 33 difficult intubations were first attempted by a junior resident while the remaining intubations were performed by a senior resident or fellow. Only 12 patients required two or more attempts at tracheal intubation. Repeat intubations were performed by senior residents/fellows for 57.1% of these patients, by the same resident for 28.6% and a consultant for 14.3% of patients. For repeat intubations, C-MAC video laryngoscopy was preferred over direct laryngoscopy for ten out of 12 patients, with the D-blade (Karl-Storz) being employed in three patients. There was no report of aspiration as a complication in any of the patients. For the 46 patients anticipated to have a difficult airway, a video laryngoscope was used twice as often as direct laryngoscopy (67.4% vs. 32.6%). In addition, for patients with predicted difficult airway, a stylet or bougie was used 43.5% of the time as compared to 33.9% of the time when a difficult airway was not anticipated.
DISCUSSION
The frequency of general anaesthesia for Caesarean delivery at our institution has declined from 20.4% in the early 2000s(14) to 4.5% in the present study, in line with global trends.(15) Similar to the indications elsewhere, general anaesthesia was administered mainly in emergency settings to facilitate expeditious delivery or when regional anaesthesia was contraindicated. The incidence of difficult intubation was 33 (1:20 or 5.0%) in 660 patients during our study. This appeared to be higher than previously reported,(11) although the definition of difficult intubation was not clearly stated in the earlier study. There was no case of failed intubation in our cohort.
The lowered frequency of employing general anaesthesia for Caesarean deliveries is a matter of concern, as it could compromise obstetric airway training.(16-18) In the United Kingdom (UK), a mandatory decrease in work hours and concomitant reduction in workload for obstetric general anaesthesia resulted in anaesthesia trainees encountering only one Caesarean general anaesthetic procedure per year at a university hospital.(18) With fewer training opportunities, trainees may not achieve the required expertise by the time they graduate and this could impact the quality of obstetric care rendered. An apparent association between the decline in Caesarean general anaesthesia exposure and an increase in failed intubations has previously been highlighted.(19,20) When the prevalence of obstetric general anaesthesia decreased from 83% in 1981 to 23% in 1994, the incidence of failed intubation was noted to increase from 1:300 to 1:250 during the same period.(19) Conversely, centres that have adopted a more liberal approach to general anaesthesia reported a lower incidence of difficult or failed intubations.(21,22) At a hospital where 4% of elective and 24% of emergency Caesarean deliveries were performed under general anaesthesia, no failed intubation was reported and only 23 difficult intubations were observed among 3,430 patients (95% confidence interval [CI] 1:238–1:100).(21) While such observations are, at best, associations, they do highlight the importance of providing trainees every learning opportunity to manage the obstetric airway.(18,23) The faculty at our institution probably subscribed to this philosophy, as 90.1% of all tracheal intubations and 28 of 33 difficult intubations were performed by residents.
Statistics on failed or difficult intubation provide ‘a valuable barometer of trainee performance‘ and could identify gaps in supervision.(12) The relatively high incidence of difficult intubation observed in our setting could be attributable to the fact that 90.1% of intubations had been performed by junior residents. The true incidence of difficult intubation is likely lower. In one study, in which senior trainees and consultants performed most of the obstetric intubations, the incidence of difficult intubation was reported to be lower than ours: 36 in 1,095 patients (3.3% or 1:30).(6) Notably, the definition of difficult intubation used in this previous study was similar to that of ours. The association between level of expertise and success at tracheal intubation is well established.(24) However, the fact that no case of failed intubation or adverse complications was encountered in our study suggests that all patients with difficult intubations were managed safely and the supervision of trainees had been adequate. Departmental guidelines on trainee supervision mandate the presence of a trained specialist of at least staff registrar grade during induction and reversal of obstetric general anaesthesia in all patients.
Simulation has been proposed as a solution to address the declining opportunities at managing obstetric general anaesthesia.(25-27) In one study, 24 trainees who attended two repeated high-fidelity simulation sessions on conducting general anaesthesia for emergent Caesarean delivery were able to reach the requisite competency level at the end of eight weeks, with retention of competence for up to eight months.(27) Simulation-based training has also been shown to improve trainees’ compliance with airway management guidelines.(25,28) Recognising these benefits, simulation-based airway training has become an integral component of the local training programme.
This study has also revealed interesting aspects of local anaesthetic practice. Preoperative prediction of difficult intubation was highly inaccurate, as three-quarters of difficult intubations were not predicted by the preoperative airway assessment. The low reliability of current tests of airway assessment has been highlighted previously.(29,30) In a retrospective cohort study of a Danish population, 93% of all difficult intubations were unanticipated, and among patients who were predicted to have difficult intubation during preoperative assessment, only 25% eventually did.(30) As no single test is reliable, a combination of tests should be used to increase the predictive value.(31) We speculate that the emergent nature of Caesarean deliveries, with time pressure to deliver, could have resulted in inadequate or incomplete airway assessment in these instances. Following this audit, we have implemented difficult airway simulation drills for rotating batches of residents during orientation and made the C-MAC video laryngoscope readily available in the obstetric theatre.
To facilitate intubation, succinylcholine remained the preferred choice, even though sugammadex has been available at our institution since 2015 and the combination of rocuronium and sugammadex could confer benefits in anticipated difficult intubations. Early comparative studies in non-obstetric populations showed that rocuronium 0.9–1.2 mg/kg produced similar intubating conditions as succinylcholine 1.0 mg/kg.(32,33) However, a recent Cochrane review of 50 studies comparing rocuronium and succinylcholine for rapid sequence induction found succinylcholine to be superior to rocuronium in achieving excellent intubating conditions (risk ratio [RR] 0.86, 95% CI 0.81–0.92) and clinically acceptable intubating conditions (RR 0.97, 95% CI 0.95–0.99).(34) Despite its less optimal intubating conditions, the availability of sugammadex for rapid reversal of rocuronium-induced neuromuscular blockade should prompt a reappraisal of rocuronium in the context of difficult airway management. The UK Obstetric Anaesthetists’ Association, in conjunction with the Difficult Airway Society, has recommended the use of rocuronium when difficult intubation is anticipated, with sugammadex as a backup.(35) We speculate that the high cost of sugammadex could have been a prohibitive factor at our government restructured hospital.
The C-MAC video laryngoscope was preferred over the Macintosh laryngoscope when a difficult airway was anticipated or encountered. This was reflective of current practice, as international airway societies now recommend the immediate availability of video laryngoscopes in difficult airway management guidelines.(35,36) Compared with direct laryngoscopy, intubations performed with a video laryngoscope are associated with a higher success rate. A study reported no case of failed intubation after video laryngoscopes were added to the difficult airway cart.(10) In a systematic review and meta-analysis comparing video laryngoscopy with direct laryngoscopy for emergency intubations outside the operating room, a greater success rate of first-pass intubations with video laryngoscopy was observed among novice/trainee clinicians but not expert practitioners.(37) Compared with direct laryngoscopy, the overall success rate for first-pass intubation improved with C-MAC (RR 1.32, 95% CI 1.08–1.62; p = 0.007). To date, no study has demonstrated the superiority of any particular video laryngoscope over others.(38) In choosing a video laryngoscope, familiarity is the key consideration.
There were a few limitations to this study. As this was a retrospective review, incomplete documentation and missing data could have introduced bias in the analysis. As the number of patients with difficult intubation was small, we did not seek to evaluate the risk factors for difficult intubation.
In conclusion, the incidence of difficult intubation among local obstetric patients delivering by Caesarean section under general anaesthesia was 33 in 660 (1:20 or 5.0%) patients during the study period. There was no case of failed intubation. The true incidence of difficult intubation was likely to be lower, as 90.1% of intubations were performed by junior residents. As the frequency of obstetric general anaesthesia is declining, there is a need to provide residents with every opportunity possible to manage the obstetric airway under appropriate supervision.


