INTRODUCTION
With the COVID-19 pandemic at its peak, governments, communities, businesses and hospitals all over the world have had to develop rapidly changing workflows and processes. The emphasis has been on extensive testing, contact tracing, early isolation and appropriate medical care.(1) The Singapore government responded to the crisis by putting in place several measures to curb the spread of the virus.
For years, Singapore has relied on migrant workers for its needs in the construction, marine shipyard, manufacturing and service industries. The Ministry of Manpower has estimated that there are over two hundred thousand workers in the construction industry alone.(2) A vast majority of these workers are from Bangladesh, India and China. Dormitories housing these workers not only provide rooms, but some (known as purpose-built dormitories or PBDs) also provide food courts, minimarts, money changers and even cinemas.
When the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus was first identified to have infected the migrant workers, there was already rapid transmission within the dormitories. The government converted these dormitories into community quarantine facilities to ensure containment of the disease. Sengkang General Hospital (SKH) responded by sending medical teams to assess, triage and treat the workers who were housed in these facilities. As this was a novel situation, various challenges were encountered during this endeavour. The medical teams were pushed to come up with targeted solutions to these problems. This article delves into the issues faced and the solutions employed by the teams managing the dormitory operations for a period of one month, roughly three months into the onset of the pandemic. We hope that this will shed some light on our experiences and provide guidance to other medical teams who may be faced with similar challenges.
OPERATIONAL DIFFICULTIES
At the beginning of April 2020, a team from SKH was tasked to perform swabs on migrant workers residing at a dormitory in Punggol who were suspected of having COVID-19. This dormitory housed approximately 15,000 migrant workers. Patients who tested positive were moved into an isolation block within the dormitory, while all other residents were quarantined within a separate part of the dormitory.
A team of emergency medicine specialists and nurses was then tasked to set up a medical post to look after the medical needs of the COVID-19-positive patients who were housed in the quarantine block. Every morning, all newly diagnosed COVID-19 patients were screened by the SKH medical team, who would assess their symptoms, vital signs and physical findings. These patients were prescribed symptomatic medications, then sent to the quarantine block. Patients who were already in the quarantine block could self-report to the medical post for review later in the morning and at a second review session in the evening. Similarly, symptomatic medications were dispensed, after which the patients would be sent back to their rooms. Patients deemed to require further investigation or management in an acute hospital were transported by an SKH ambulance for stable patients and by Emergency Medical Services for emergency cases.
All other residents in the dormitory who were not diagnosed as COVID-19 positive were seen by a separate medical team at a medical post run by the Singapore Armed Forces (SAF) Medical Corps. Again, this group of residents would self-report to the SAF medical post either during a morning or an afternoon session to have their medical needs attended to.
The SAF and SKH teams were run entirely independent of each other. This led to issues of different workflows, medication availability and lack of continuity of care should an initially COVID-19-negative patient managed by the SAF team become COVID-19 positive, after which their care would be transferred to the SKH team. Other differences between the teams included: how patients were brought to the clinic by the dormitory security and staff; the type of medications used to treat symptoms of upper respiratory tract infections, gastritis and musculoskeletal pain; and how patients were transferred to the hospital Accident and Emergency (A&E) departments. This caused confusion for both the dormitory operators and patients alike. Duplication of resources used in terms of manpower and medical equipment also naturally led to inefficient utilisation. Equipment such as blood pressure machines, stethoscopes and blood oxygen saturation probes, and storage spaces for medications could have been made universally available to both teams, with decontamination of the equipment being done after each clinic session. Clinics looking after the COVID-19-positive and COVID-19-negative patients could have been staggered so that a single team could be deployed onsite, with the equipment used being decontaminated between clinics. This would reduce the manpower requirement of running two teams. Since decontamination of equipment was already being done after each clinic session, there would be no additional logistical and manpower requirements for running the clinics with a single team.
These issues were resolved when SingHealth took over the management of all medical activities at the dormitory in the beginning of May 2020. A standardised workflow was established in consultation with the SKH A&E department, which was designated to receive potentially unwell patients. Medications received by all patients within the dormitory were also standardised and dispensed by a central SingHealth pharmacy. Resources were also more efficiently utilised with a single team of doctors and nurses, along with a central set of medical equipment and personal protective equipment (PPE) being used at the medical post. Clinics looking after COVID-19-positive patients and COVID-19-negative patients were also staggered, eliminating the need for two separate teams.
MEDICAL DIFFICULTIES
Identifying COVID-19-positive patients at the dormitory who were deteriorating or at risk of deteriorating proved to be challenging. COVID-19 patients with respiratory complications, acute coronary syndromes or prothrombotic events such as pulmonary emboli need to be identified early to ensure that they can be managed appropriately in an acute hospital. Unfortunately, these conditions tend to be asymptomatic early in their presentation. Thus, a thorough history, physical examination and vital sign assessment might not be sufficient to safely discharge the patients back to their rooms. This difficulty was exacerbated by the fact that over 75% of the dormitory residents comprised Muslims who were fasting for Ramadan during that period, resulting in many presenting with symptoms of gastritis and dehydration. The resultant tachycardia, and chest and epigastric pain made it difficult to discern a benign diagnosis from a life-threatening one.
To mitigate this risk, it was decided that there would be a low threshold for transfer of patients with chest pain, dyspnoea or disproportionate tachycardia to the SKH A&E. This inevitably led to an increased burden on the A&E. Suggestions to further improve risk assessment at the medical post include providing the medical teams based at these facilities with electrocardiography (ECG) machines, portable/handheld ultrasonographic devices(3,4) and point-of-care blood test devices. This would enable the teams to better risk-stratify patients using risk assessment criteria, such as the HEART score,(5) thus identifying dynamic changes on serial ECG, picking up acute coronary events with elevated cardiac enzymes on five-minute point-of-care troponin tests and detecting ultrasonographic changes suggestive of a pulmonary embolus. This would provide the medical teams with objective criteria to safely discharge patients back to their rooms or decide that escalation of care to an acute hospital was necessary. While these additional measures may lead to increased running costs for such medical posts, they will improve patient safety through more accurate diagnosis, as well as reduce the load on acute hospitals.
PSYCHOLOGICAL DIFFICULTIES
Through interactions with the dormitory residents, we identified that some of them were experiencing stress and anxiety over movement restrictions in the dormitory, as well as over uncertainties regarding their future. Feedback on food, living conditions, salary and employment issues was elicited, but we were unable to explore these problems further owing to limitations in communication and lack of subject matter expertise. Partnering with non-governmental organisations (NGOs) helped to address some of these matters.
An automated helpline was established and publicised in the dormitory for residents who were experiencing stress or required case-work or social assistance. Residents experiencing high levels of stress, anxiety or depression were also referred to trained counsellors or psychiatrists, as required. Website and pamphlets were created and made available in the languages spoken by the residents to include daily updates on COVID-19 numbers, resources for help and educational materials. In addition, focus group discussions facilitated by the NGOs helped to identify issues regarding food and living conditions, which were then relayed to the dormitory management so that the necessary improvements could be made.
COMMUNICATION DIFFICULTIES
The heterogeneous composition of the residents made effective communication during consultation and dispensing difficult. Most of the dormitory residents were able to converse with the medical team in basic English. Clarifications often required an interpreter, which increased the throughput time.
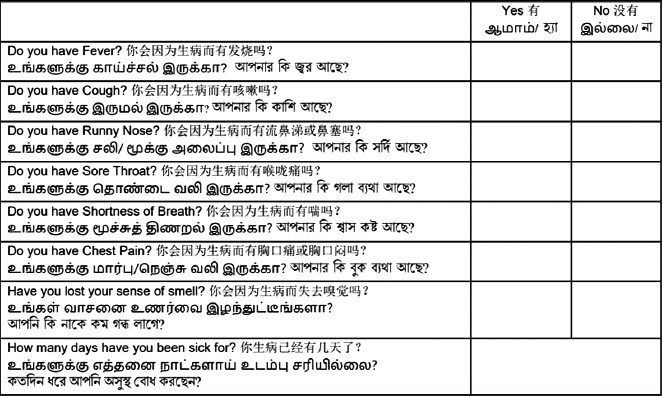
A pre-screening questionnaire was created with common presentations translated from English to Tamil, Bengali and Mandarin. During the consultation, the doctor had to clarify and confirm the symptoms that the patients self-reported in the questionnaire before proceeding with the examination. Although having an interpreter on site would have been ideal, such resources were unavailable during that period. Written translations such as the questionnaire helped mitigate this problem by bridging the communication gap.
Fig. 1
Image shows sample of the questionnaire in four languages: English, Tamil, Bengali and Mandarin.
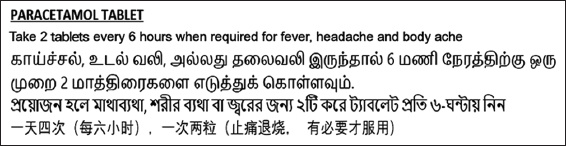
At the start of the operation, medications were prepared and labelled in English by the hospital pharmacy. These medication labels were poorly understood by the dormitory residents. Therefore, there was a significant risk of medication error and noncompliance owing to misinterpretation of the medications’ function, dosage and frequency. To address this issue, we worked with hospital pharmacists and volunteers from the local community who spoke the native languages of the dormitory residents to translate the English medication labels to Tamil, Bengali and Mandarin (
Fig. 2
Image shows sample of a medication label in four languages: English, Tamil, Bengali and Mandarin.
ENVIRONMENTAL DIFFICULTIES
The clinics in the dormitory were held at the sheltered canteen areas. Although ceiling fans were available, working in full PPE during the day when it was often hot and humid proved to be physically challenging for the medical team. Heat exhaustion and heat strokes were serious considerations. Prolonged use of N95 masks also led to facial pressure sores and skin erosions. These problems were controlled by ensuring that staff were well-hydrated prior to the start of the clinic and took regular breaks every two hours, where they were able to remove their PPE in clean zones and hydrate with the provided beverages. Staff who were feeling unwell during the clinic were also encouraged to alert their colleagues early and to remove their PPE in clean zones for the purpose of hydration and rest. Thankfully, none of the healthcare staff deployed experienced such heat-related injuries.
CONCLUSION
To ensure an effective medical post at quarantine facilities, a holistic approach to planning should be taken. A starting point would be communication and agreement with the designated acute hospitals on workflows and resources. Ideally, the medical post should be run by a single organisation that is supplied with adequate manpower and necessary portable equipment to effectively manage most cases in these facilities. Effective communication in multiple languages for medical consultation and medication use must also be accounted for. It would be prudent to consider partnering with NGOs that already have experience, expertise and motivation in looking after the logistical and psychological needs of this group of patients.


