Abstract
INTRODUCTION
Patients with chronic diseases face difficulties when navigating the healthcare system. Using the Healthcare System Hassles Questionnaire (HSHQ) developed by Parchman et al, this study aimed to explore the degree of hassles faced by patients in primary care in Singapore and identify the characteristics associated with greater hassles.
METHODS
A cross-sectional study was conducted on patients with chronic diseases at Hougang Polyclinic, Singapore, using the interviewer-administered HSHQ. The mean HSHQ score was compared with that reported by Parchman et al. The associations between the number of chronic diseases, demographic variables and healthcare hassles were assessed using multivariate linear logistic regression analysis.
RESULTS
In total, 217 outpatients aged 21 years and above were enrolled. Their overall mean HSHQ score (4.77 ± 6.18) was significantly lower than that of patients in the study by Parchman et al (15.94 ± 14.23, p < 0.001). Patients with five or more chronic diseases scored 3.38 (95% confidence interval [CI] 0.11–6.65, p = 0.043) points higher than those with one chronic disease did. With each increasing year of age, the mean HSHQ score decreased by 0.17 (95% CI −0.26 to −0.08, p = 0.001) points. Patients with polytechnic/diploma/university education and higher scored 2.65 (95% CI 0.19–5.11, p = 0.035) points higher than those with primary education and lower did.
CONCLUSION
Patients in our population reported less hassles than those in the study by Parchman et al did. Increasing age and lower education level were associated with less hassles. Further analysis of the types of chronic diseases may yield new information about the association of healthcare hassles with the number and types of chronic diseases.
INTRODUCTION
A chronic disease is a disease that lasts three months or more, as defined by the United States (US) National Center for Health Statistics, and it is increasingly common to encounter patients with chronic diseases in the primary care setting.(1) Patients with chronic diseases may face difficulties such as poor continuity of care, and poor communication between healthcare providers and polypharmacy.(2)
The difficulties faced are even more evident in patients with multimorbidity,(3) which is commonly defined as the presence of two or more chronic diseases.(4,5) These patients may have reduced quality of life, psychological distress, increased healthcare utilisation and admissions, and poorer outcomes.(2) Studies have described the difficulties that patients with chronic diseases face during their encounters with the healthcare system,(6-16) some of which focused on just one aspect of the difficulties, such as access to care and waiting times,(10-12) medication-related difficulties(13-15) or communication difficulties.(16)
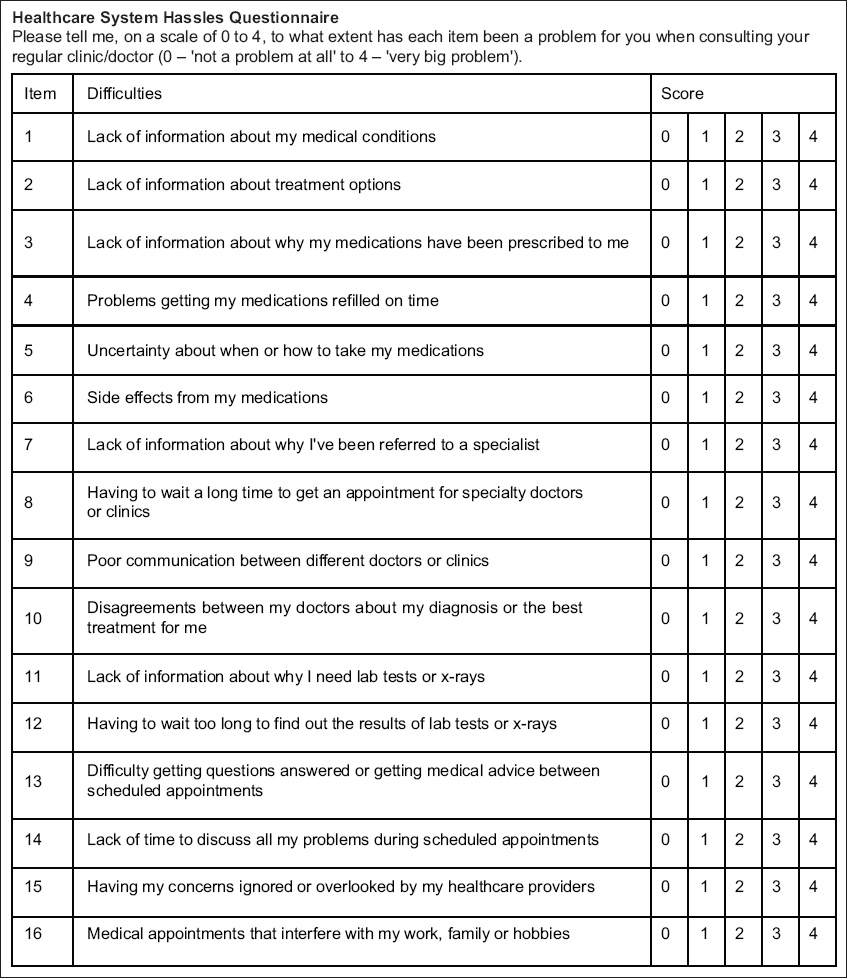
In a study conducted by Parchman et al, the Healthcare System Hassles Questionnaire (HSHQ) was constructed to enable patients with chronic diseases to report the overall difficulties experienced in accessing care within a primary healthcare setting (
Fig. 1
Image shows the Healthcare System Hassles Questionnaire.
Another study that used the HSHQ, conducted in the United Kingdom by Adeniji et al, reported that the hassles most often reported by patients with two or more diseases related to lack of information about diseases and treatment options, poor communication among health professionals and poor access to specialist care.(9)
In Singapore, the Patient Satisfaction Survey is conducted every year by the Ministry of Health to assess patient satisfaction with public healthcare institutions.(17) The survey covers the level of patient satisfaction, extent to which their expectations were met, whether they would recommend the services to others and the affordability of services. It does not cover specific difficulties faced by patients, such as problems with medications, and problems with understanding medical diseases and treatment options.
To our knowledge, broader quantitative studies have not been conducted in Singapore about the overall hassles or difficulties that patients with chronic diseases face during their encounters with the healthcare system. Studies have also shown that sociodemographic differences, such as age and ethnic differences, can affect patients’ assessments of primary healthcare, and it would be useful to identify these variables in our population.(7,18-21)
This study aimed to: (a) explore whether patients in Singapore faced the same degree of hassles when compared with the patients in the study by Parchman et al; (b) determine whether patients with more chronic diseases faced more hassles; and (c) identify the characteristics associated with higher healthcare system hassles among patients with chronic diseases.
METHODS
This was a cross-sectional study conducted among patients attending Hougang Polyclinic in Singapore for chronic diseases. An interviewer-administered questionnaire – including basic demographic data and the HSHQ, which is a 16-item questionnaire on a five-point Likert scale (0 denotes ‘not a problem at all’ and 4 denotes ‘very big problem’) – was administered between 31 January 2017 and 12 April 2017. Approval from the National Healthcare Group Domain Specific Review Board (approval number 2016/01130) was obtained prior to commencement of the study.
Sample size was calculated to compare the overall mean HSHQ score with that of the original study by Parchman et al that used the HSHQ (mean 15.94 ± 14.23).(8) The difference in the mean score between the two study groups in the study by Parchman et al (patients with single morbidity and those with multimorbidity) was 3.8 and, assuming the difference in the mean score between the study by Parchman et al and our present study to be 3.8 and above, using two-sample t-test with a significance level of 5%, a minimum of 215 participants were found to be necessary to achieve a statistical power of 80%.
Patients aged 21 years and above, with one or more chronic diseases, attending Hougang Polyclinic and those who were able to speak English or Mandarin were included. A total of 19 chronic diseases, which were the diseases under the Ministry of Health’s Chronic Disease Management Programme when this study was conducted, were included. The 19 chronic diseases were anxiety, asthma, benign prostatic hyperplasia, bipolar disorder, chronic obstructive pulmonary disease, dementia, diabetes mellitus, epilepsy, hypertension, lipid disorders, major depression, nephritis/nephrosis/chronic kidney disease, osteoarthritis, osteoporosis, Parkinson’s disease, psoriasis, rheumatoid arthritis, schizophrenia and stroke.(22)
Patients who had cognitive impairment and those who were unable to provide informed consent were excluded from the study. Pregnant women were also excluded.
A list of patients who were aged 21 years and above, with at least one chronic disease, and scheduled for follow-up for their chronic disease(s) at Hougang Polyclinic from January 2017 to April 2017 was obtained. From 31 January 2017 to 12 April 2017, patients were randomly selected from this list by utilising a random number generator using Microsoft Excel 2013 (Microsoft Inc, Redmond, WA, USA) and approached while they were waiting for their consultation. In total, 363 patients were approached, of which 33 patients were ineligible and excluded after applying the inclusion and exclusion criteria. Of the 330 eligible patients, 113 patients refused or had other reasons not to participate in the study (e.g. feeling unwell) and 217 patients consented to participate in the study. The response rate was 65.8%.
The study procedure was conveyed to patients and they were given sufficient time to consider their participation. Written informed consent was then obtained and the questionnaire was administered by the interviewer. The study investigators personally trained the interviewers, and each interview session lasted 20–30 minutes. Electronic medical records were accessed to obtain information regarding the number of chronic diseases that each patient had.
The test-retest reliability of the questionnaire was evaluated before the commencement of the study. Ten patients answered the HSHQ twice, two weeks apart. They also evaluated the face validity of each question, in which they were asked to comment on the clarity of wording and the likelihood that the target audience would be able to answer the questions. The HSHQ was translated into Mandarin using forward-translation and then verified via back-translation, which was carried out independently by different persons with appropriate qualifications to ensure accuracy.
The sociodemographic characteristics of the patients were analysed descriptively. The overall mean HSHQ score was compared with that in the original study by Parchman et al using two-sample t-test. The overall mean HSHQ scores for each chronic disease count were analysed to determine the significance of the relationship between the mean score and the number of chronic diseases.
Bivariate analysis (Mann-Whitney U test or Kruskal-Wallis test) was conducted to explore the relationship between each independent sociodemographic variable and the mean HSHQ score. Multivariate logistic regression analysis was used to analyse the impact of the variables on the mean HSHQ score while controlling for other sociodemographic variables.
Cronbach’s alpha coefficient was calculated to measure the internal consistency of HSHQ responses in our population. A p-value < 0.05 was considered statistically significant. Data was presented as mean and standard deviation. All analyses were conducted using Stata SE version 13.1 (StataCorp LLC, College Station, TX, USA).
RESULTS
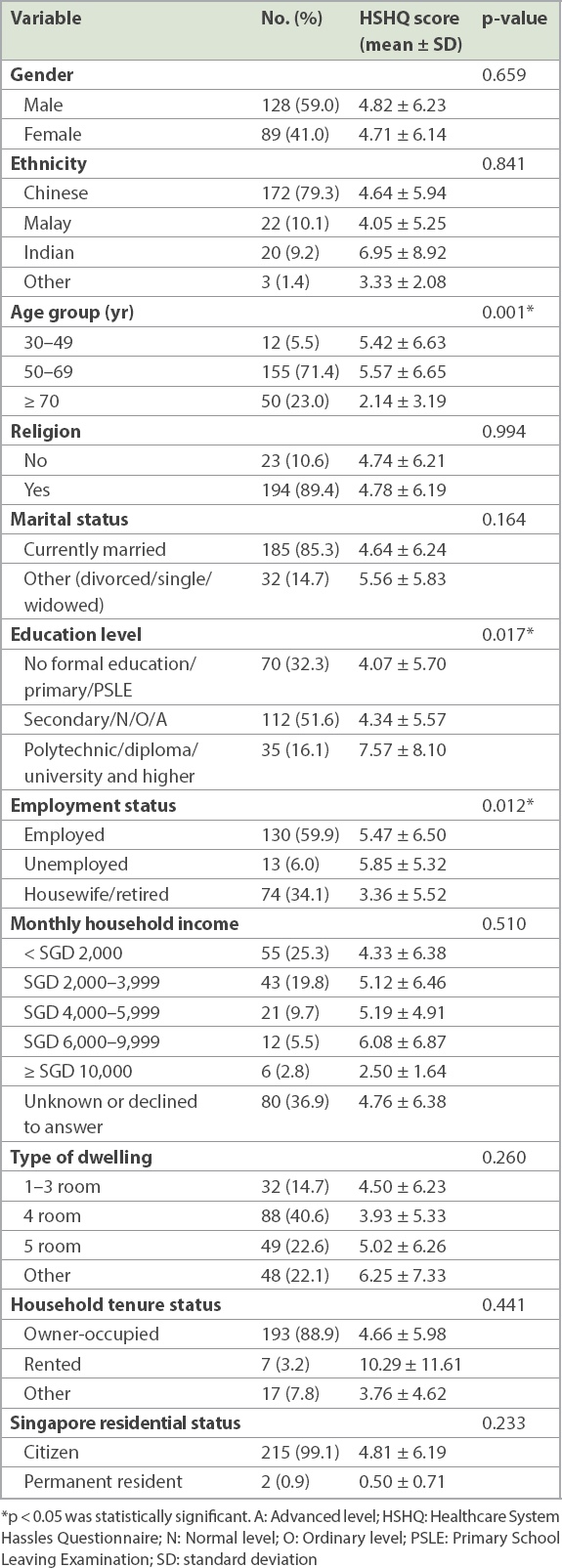
In total, 217 participants aged 21 years and above who had at least one chronic disease and who were on follow-up for chronic disease(s) at the polyclinic were enrolled. Their mean age was 63.0 ± 8.9 years and the average number of chronic diseases was 2.9 ± 1.0. All participants were Singapore citizens or permanent residents, and a majority of them were ethnically Chinese (79.3%), aged 50 years and above (94.4%), married (85.3%) and with a religion (89.4%) (
Table I
Sociodemographic characteristics (n = 217) and mean HSHQ score.
The HSHQ scores showed good internal consistency for our study population, with a Cronbach’s alpha of 0.8. It also demonstrated excellent test-retest reliability, with an intraclass correlation coefficient of 0.98 (95% confidence interval [CI] 0.93–0.99).
The top three hassles reported by our participants (items that scored the three highest mean HSHQ scores) were long waiting times for clinic or specialist appointments; poor communication between different doctors or clinics; and medical appointments interfering with work, family or hobbies.
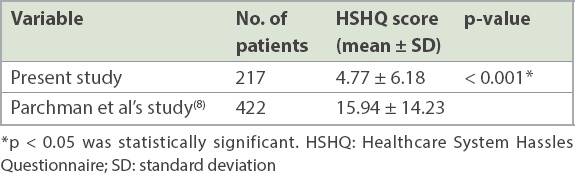
The overall mean HSHQ score in our study population (4.77 ± 6.18) was significantly lower (p < 0.001) than that in the original study by Parchman et al (15.94 ± 14.23) (
Table II
Mean HSHQ scores in the present study and that by Parchman et al.
Some sociodemographic variables were found to be associated with lower or higher mean HSHQ scores. Patients aged 70 years and above had a lower mean score (2.14 ± 3.19) than those aged 30–49 years (5.42 ± 6.63) and 50–69 years (5.57 ± 6.65) (p = 0.001). Patients with a polytechnic/diploma/university education and higher (7.57 ± 8.10) had higher HSHQ scores when compared with those with primary education (4.07 ± 5.70) and lower and secondary/N/O/A-level education (4.34 ± 5.57) (p = 0.017). Those who were housewives or retired (3.36 ± 5.52) had lower HSHQ scores than those who were working (5.47 ± 6.50) or unemployed (5.85 ± 5.32) (p = 0.012).
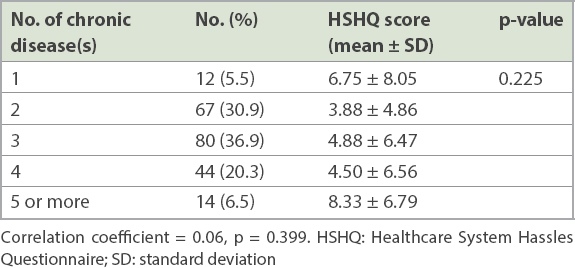
When analysed with respect to the number of chronic diseases (
Table III
Relationship between the number of chronic diseases (n = 217) and the mean HSHQ score.
Multivariate linear logistic regression analysis with backward elimination was performed with respect to all demographic variables in
Table IV
Multivariate linear logistic regression analysis with backward elimination.
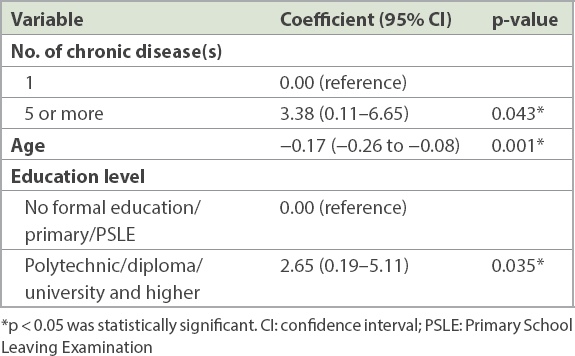
Participants with five or more chronic diseases were found to have a mean HSHQ score that was 3.38 (95% CI 0.11–6.65, p = 0.043) points higher than the score of those with one chronic disease. With each increasing year of age, the mean score was found to decrease by 0.17 (95% CI −0.26 to −0.08, p = 0.001) points. Those with primary education and lower were found to have a mean score that was 2.65 (95% CI 0.19–5.11, p = 0.035) points higher than the score of those with polytechnic/diploma/university education and higher.
DISCUSSION
The ethnic (79.3% Chinese, 10.1% Malay and 9.2% Indian participants) and age composition of our study population was consistent with the overall ethnic and age composition of patients attending Hougang Polyclinic in 2014 (77% Chinese, 10% Malay, and 10% Indian). The median age of the patients in our study was 63.0 ± 8.9 years, and the age of patients attending Hougang Polyclinic in 2014 ranged from 40 to 64 years.
The overall mean HSHQ score for our study population was lower than that for the patients in the original study by Parchman et al, and this difference could be attributable to several reasons. Parchman et al’s study was conducted among veterans in a veteran healthcare system and the surveys were administered by mail, with a response rate of 59%. Self-administration of questionnaires may increase participants’ willingness to disclose information when compared with face-to-face or telephone interviews. The greater anonymity offered by mail has been reported to lead to more accurate reporting on topics such as health and behaviour.(23)
Parchman et al’s study population of veterans in the US setting may also have had other socioeconomic reasons that resulted in a higher proportion of self-reported hassles. The mean patient age in their study was also lower (53.8 years) than the mean patient age in our study (63.0 years) and, as proven in our study and other studies, older patients rated healthcare more favourably.(7,18-20)
The participants in our study were also likely to have had concerns that negative responses would affect the healthcare provided to them, although they were reassured that their responses would not affect their quality of care.
Quantitative studies may not be the best way to assess the difficulties that patients encounter, and further studies, such as qualitative studies, can be conducted to investigate these difficulties.
Both Parchman et al and Adeniji et al found that a higher number of chronic diseases was associated with more healthcare hassles.(8,9) Our study found that participants with five or more chronic diseases had a higher mean HSHQ score than those with one chronic disease did. However, we did not find a linear relationship between mean HSHQ score and the number of chronic diseases in our participants. This could, in part, be attributable to the types of chronic diseases included rather than the absolute number of chronic diseases present.
Different combinations of diseases pose different burdens to patients. Some multimorbidity studies have clustered the diseases by gathering them into groups of non-random associations. Examples of common non-random associations of diseases are groups of cardiovascular and metabolic disorders, mental health problems and musculoskeletal disorders.(2,24-26) A patient who has one disease from all three clusters – one each from the cardiovascular and metabolic group, mental health group and musculoskeletal group – could suffer from more problems, such as poor coordination of care and having to attend many different appointments, compared with a patient with three diseases that are all from the same cluster, such as hypertension, hyperlipidaemia and diabetes mellitus.
The burden of different diseases varies as well. For example, a patient suffering from stroke with hemiplegia would likely experience more difficulties than a patient with hypertension.
These reasons could partly account for the lack of an expected linear relationship between the number of chronic diseases and the mean HSHQ score. Further information could be gathered and further analyses could be conducted to determine whether patients with diseases across different clusters score higher than patients with single-cluster multimorbidity do and whether the type of disease(s) affect the mean HSHQ score.
Elderly patients (aged 70 years and above) and those with primary education and lower were found to have lower HSHQ scores in our study. Previous studies have shown that older patients tend to rate care more favourably than younger patients do.(7,18-20) The reasons postulated included cultural differences in the willingness to report unfavourable assessments among older patients, and the higher morbidity and consulting rates among older patients may mean that this group may have more contact with primary care facilities and may be more acquainted with the system.(18) Studies in Asian populations have also shown that patients with lower education levels or those who were illiterate reported greater satisfaction with healthcare.(27,28)
Measures should be taken to address the difficulties that patients face during their interactions with the healthcare system. In Singapore, patients with chronic diseases often attend polyclinics, which are public primary care clinics. Although private general practitioners currently provide around 80% of primary care in Singapore, only 55% of all patients with chronic diseases are managed by them; polyclinics manage the remaining 45%.(29) A majority of these patients are randomly assigned a doctor at each consultation and often do not get to consult the same doctor at the next visit. Some polyclinics in Singapore have piloted a new model of care, based on a patient empanelment healthcare model in the US, wherein patients with chronic diseases are grouped with the same team of healthcare providers and are cared for by the same few doctors and nurses.(30,31) This may be an avenue to increase rapport and familiarity between patients and doctors, improve continuity of care and reduce the difficulties that patients face. When this is implemented more widely, and if other measures to reduce the difficulties that patients face are implemented, follow-up studies could be conducted to assess whether the degree of hassles (or mean HSHQ score) decreases.
Future studies could relate the degree of hassles faced to the healthcare outcomes of patients and also compare the types of hassles faced between the different studies. Qualitative studies could also explore patient interpretations of the various questions.
This study has some limitations. We did not track whether language barrier was a reason for rejecting participation in our study and, hence, were unable to ascertain whether there was responder bias in our study population owing to conducting the survey in English and Mandarin only. However, we noted that almost all of the Malay and Indian participants we approached were able to converse in English. This study was conducted in only one polyclinic in Singapore and, had resources allowed, the inclusion of more sites of primary care would have been ideal. Although measures were taken to optimise the translation of the questionnaire to Mandarin (using forward and backward translations), there might still have been terms and/or concepts that were not conveyed accurately in the Mandarin questionnaire.
In conclusion, patients in our population reported a significantly lower level of hassles than those in the original study by Parchman et al did, and further studies, such as qualitative studies, could be conducted to elucidate the reasons for this. The characteristics associated with less hassles were increasing patient age and lower education level. Further analysis of the types of chronic diseases in our population may yield new information about the association between the number and types of chronic diseases included and the healthcare hassles reported. It is suggested that after measures to reduce the difficulties that patients face have been implemented, a follow-up study be conducted to assess whether patients subsequently report less hassles.
ACKNOWLEDGEMENTS
We would like to thank Prof Doris Young, Research Advisor, Clinical Research Unit, National Healthcare Group Polyclinics (NHGP), Singapore for advising on this study and Dr Michael Parchman, Kaiser Permanente Washington Health Research Institute, WA, USA, for the use of the Healthcare Systems Hassles Questionnaire, which is available in the public domain. We would also like to thank Ms Kyreen Lee, NHGP Clinical Research Unit, Singapore and all clinic staff at Hougang Polyclinic, Singapore for their contribution to this study. This research was supported by National Medical Research Council, Ministry of Health, Singapore under the Centre Grant Programme (reference no.: CGAug16C019).


