Dear Sir,
Peripherally inserted central catheters (PICCs) are commonly inserted in very low birth weight infants, but these insertions are not without risks. We herein report a case of an inadvertent arterial cannulation of a radial artery branch during the insertion of a PICC, with subsequent infusion of parenteral nutrition, in a preterm infant of 32 weeks gestational age and weighing 970 g.
The cannulation insertion site was the dorsum of the hand and was close to, but not within, the anatomical snuffbox. There was no excessive bleeding during the insertion. Soon after parenteral nutrition was infused, the limb was noted to be pale from the cubital fossa downwards, with reduced perfusion and absent distal pulses (Figs.
Fig. 1
Photograph of the dorsum of the neonate’s hand shows (a) areas of pallor and duskiness distal to the cubital fossa soon after infusion of parenteral nutrition through the peripherally inserted central catheter; (b) duskiness confined to the tip of the index finger after initiation of anticoagulation; and (c & d) a warm and pink appearance, with minimal ischaemia of the index fingertip pulp, after stopping anticoagulation.
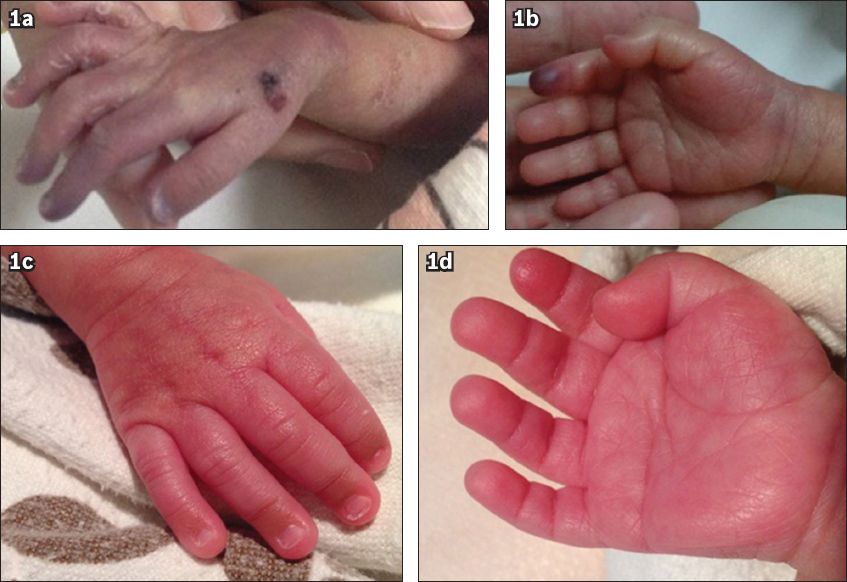
Unfractionated heparin was started within 12 hours of the event at a dose of 15 units/kg/hour, but was subsequently replaced with enoxaparin after 12 hours due to a rapid rise in partial thromboplastin time and a high risk of bleeding in the neonate. Enoxaparin was initiated at 1 mg/kg/dose every 12 hours with monitoring of the anti-factor Xa levels and was continued for two weeks. To achieve a targeted therapeutic anti-factor Xa level of 0.5–1.0 IU/mL, maximum enoxaparin of 1.65 mg/kg/dose every 12 hours was administered and the highest anti-factor Xa level (i.e. 0.47 IU/mL) was achieved on Day 14. Anticoagulation dosing and monitoring was managed, with advice from a paediatric haematologist, and the patient did not develop any abnormal bleeding or thrombocytopenia. A transdermal glyceryl trinitrate patch was applied to the cubital fossa about 12 hours after the initiation of unfractionated heparin and was continued for one week. Repeat Doppler ultrasonography performed on Days 2 and 3 still showed no flow to the brachial artery. There was clinical improvement in the limb by Day 5 and minimal ischaemia of the index fingertip pulp, with full range of movement of the fingers and good grasp clinically, by Day 13 (Figs.
Arterial cannulation as a complication of PICCs has been reported in adults, but this is the first case reported in a neonate. There has been only one published case series of two neonates with significant digital ischaemia following intravenous cannulation and administration of parenteral nutrition, crystalloid and blood products.(1) Familiarity with the normal arterial anatomy of the hand is essential in preventing vascular compromise. The anatomical snuffbox is a potentially dangerous insertion site, as it contains the radial artery after it has curved dorsally and distally at the lateral aspect of the wrist to reach the deep palmar arch.(2) The first web space is the second area to avoid, as the princeps pollicis artery, a branch of the radial artery that provides the blood supply to the thumb, transverses the first web space superficial to the muscles to reach the thumb.(1) Radial artery anomalies, though uncommon, may also exist and be predisposed to inadvertent arterial cannulation. One example of the anomaly is the antebrachialis superficialis dorsalis artery, which has an estimated incidence of 0.5%–1%.(3) The anomaly involves a radial artery bifurcation in the forearm, resulting in an anomalous superficial branch that will cross underneath a terminal branch of the cephalic vein superficial to the radial styloid process, a common insertion site of intravenous catheters.(3) Finally, abnormal vasculatures, such as arteriovenous malformations or fistulas, may result in arterial compromise during PICC insertion.
Both mechanical and chemical injuries contribute to arterial vessel damage, resulting in intimal damage and thrombosis.(1) The use of low-molecular-weight heparin is less established in neonates than in older patients. Studies have shown that preterm neonates require a longer time and higher doses to achieve and maintain target anti-factor Xa levels.(4) There have been published case reports and case series of the use of topical glyceryl trinitrate for the reversal of peripheral ischaemia due to arterial cannulation in preterm infants, and the outcomes are uniformly positive.(5)
To reduce arterial damage, it is important to recognise the malposition of PICCs early, by means of close circulation monitoring of the respective limb and necessary imaging, and not infuse potentially damaging substances until correct line placement is ascertained. In the event of inadvertent arterial cannulation, early removal of the PICC and initiation of anticoagulation therapy may reduce the likelihood of the development of distal ischaemia and gangrene.(6)
Yours sincerely,


