Abstract
INTRODUCTION
There is limited data on the psychopathology of eating disorders in Singapore. This study: (a) described levels of eating psychopathology and psychosocial impairment among individuals diagnosed with eating disorders at our hospital; and (b) compared the related psychopathology of these patients.
METHODS
Between 1 August 2010 and 31 July 2012, 257 individuals who met the diagnostic criteria for eating disorders completed the Eating Disorder Examination Questionnaire (EDE-Q) and Clinical Impairment Assessment questionnaire (CIA).
RESULTS
A majority of participants were women and of Chinese ethnicity. Diagnoses included anorexia nervosa (AN; 41.6%), bulimia nervosa (BN; 29.6%) and eating disorder not otherwise specified (EDNOS; 28.8%). Mean age at presentation was 20.52 ± 7.14 years and mean body mass index was 17.84 ± 4.18 kg/m2. Individuals with AN were significantly younger at presentation and had shorter duration of untreated illness compared to those with BN and EDNOS. There were no significant differences in the CIA scores of the diagnostic groups. Participants with BN scored higher in all subscales of the EDE-Q than those with AN and EDNOS. Our sample scored lower in most subscales of EDE-Q when compared to treatment centres in Sweden, Australia and the United States.
CONCLUSION
Our clinical sample reported lower scores of psychopathology compared to overseas centres. This could be attributed to the higher percentages of BN and EDNOS diagnosed in overseas populations. Individuals with AN showed higher levels of psychopathology in our study compared to patients from the United States.
INTRODUCTION
A recent epidemiological study in the United States based on the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders reported that the lifetime prevalence of anorexia nervosa (AN) among women might be as high as 4% and that of bulimia nervosa (BN) to be around 2%.(1) This is a large increase when compared to another study done nearly a decade ago that reported prevalence rates of 0.3%–1% across diagnoses.(2) Such trends toward thinness or features of AN were once associated with high socioeconomic status among young female North European Caucasians.(3) The disorder and its associated behaviours and cognitions were once thought to be rare outside of Western countries, but appear to have now become more prevalent in various Asian countries, such as Taiwan,(4) Hong Kong(5) and Japan.(6) Similarly, the number of individuals in Singapore diagnosed with eating disorders has been on the rise over the years(7-9) – from six new presentations in 1994 to 24 in 2002;(7) a decade later in 2012, the numbers have increased to 163 newly diagnosed individuals(9) at the Singapore General Hospital (SGH), Singapore.
Eating disorder psychopathology can be experienced in various domains, such as restricting one’s diet, concerns over one’s body size and shape, and fear of weight gain. Such domains can be measured using the Eating Disorder Examination Questionnaire (EDE-Q). A study reported that preference for thinness is the ideal among young Chinese Singapore women, even though they might be underweight.(10) This echoes the findings of a large sample study that investigated the degree of body dissatisfaction among Chinese undergraduates in Hong Kong.(5) Another study that examined the restraint and eating concerns of young women in Australia and Singapore revealed that Singaporean Chinese women in the control group had greater overall eating disorder psychopathology compared to other cultural groups and greater restraint than North European Australians or expatriates.(11) However, a study from the United States that investigated the profile and clinical features of adolescents who underwent family therapy trial for AN reported that Asian American adolescents scored lower in the EDE-Q than their non-Asian peers, significantly in the restraint and weight concern subscales.(12)
A study that compared the psychopathology of young women of different ethnicities in Australia and Singapore reported that those with eating disorders had similar psychopathology across ethnicities, whereas a higher level of eating disorder psychopathology was found in Singaporean controls than their Australian counterparts and expatriate Singaporeans.(11,13) Another study examined the level of eating disorder behaviour in healthy controls from Australia and Singapore using the EDE-Q.(14) It reported that even though the overall levels of eating disorder psychopathology were very similar between the two populations, Singaporean women were found to be more fearful of losing control over their eating and of weight gain or becoming fat, and more anxious at the prospect of weighing themselves regularly. Such findings seem to suggest that levels of eating psychopathology may be high in the general Singapore population.
The Eating Disorder Examination Interview (EDE)(15) is considered the gold standard for assessing eating disorder psychopathology, but is more time-consuming and costly, as a trained assessor is required to administer the semi-structured interview. The adapted EDE-Q, however, has good psychometric properties(16) and can be used as a clinical measure of treatment response. Being a self-reported instrument, a possible advantage of the EDE-Q is that the respondent may be more willing to disclose certain sensitive behaviours deemed to be shameful and secretive.(17) On the one hand, eating disorders are associated with negative impact on psychosocial functioning and lower quality of life;(18) on the other, this psychosocial impairment leads one to seek help and treatment.(19) The Clinical Impairment Assessment questionnaire (CIA) is a tool designed to specifically assess the severity of psychosocial impairment due to an eating disorder and is to be filled in by the respondent immediately after completing a measure of current eating disorder symptoms.(20)
We aimed to use the above instruments to determine: (a) the level of eating psychopathology and psychosocial impairment among individuals diagnosed with an eating disorder at our hospital; and (b) if there were any differences in levels of eating psychopathology and psychosocial impairment among individuals with different eating disorder classifications. We hypothesised that the level of eating psychopathology and psychosocial impairment of our clinical population would be similar to that in overseas treatment centres. We also hypothesised that participants with BN would experience higher levels of psychopathology when compared to those with AN.
METHODS
Participants were recruited from our hospital’s eating disorder treatment programme for patients aged ≥ 12 years. Referrals were from multiple sources, including inpatient wards, clinics, other hospitals, community clinics and self-referrals.
Individuals who saw a psychiatrist at SGH for the first time between 1 August 2010 and 31 July 2012 were asked to complete a set of self-reported questionnaires, consisting of a demographical data sheet, the EDE-Q and CIA. The study was approved by the institutional research review board. Written consent was obtained from participants aged ≥ 21 years, while for participants who were minors, consent was obtained from both the individual and parent. Eating disorder diagnoses were made by the treating psychiatrist according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition. Participants were included if they were diagnosed with AN, BN or eating disorder not otherwise specified (EDNOS) and had completed both questionnaires. Within the study’s time frame, 257 individuals met the inclusion criteria. Individuals were excluded from the study if they were not diagnosed with an eating disorder, had not completed the questionnaires or did not provide consent.
The EDE-Q version 6.0 is a self-reported, adapted version of the widely used EDE. It focuses on the past 28 days and scores on a 7-point Likert scale. It comprises four subscales designed to measure the domains of dietary restraint, weight concern, shape concern and eating concern.(17) An average of the subscale score is calculated when at least half of the items in each subscale have been completed. Higher scores indicate higher levels of psychopathology severity or frequency. A global score is obtained from the average of four subscales and has been shown to have high internal consistency (Cronbach’s alpha 0.93).(21) It must be noted, however, that EDE-Q validity studies have not been done with a Singaporean population.
The CIA is a 16-item self-reported questionnaire that measures the severity of psychosocial impairment due to features of eating disorders(20) in the past 28 days. It is designed to be administered immediately after the EDE-Q or an equivalent eating disorder psychopathology measurement tool. Each item is scored against a 4-point Likert scale and the scores are calculated to generate a single global score, with the requirement that at least 12 items have to be completed. The CIA has been shown to have good internal consistency (Cronbach’s alpha 0.97) and acceptable overall test-retest reliability, with an intraclass correlation coefficient of 0.86.(19) The best cutoff point was seen to be a global CIA score of 16, with 76% sensitivity and 86% specificity.(19) It was also reported that the global CIA score can predict case status,(19) with a higher score being indicative of a higher level of psychosocial impairment. However, CIA validity studies have also not been conducted on a Singaporean population.
SPSS Statistics version 17.0 for Windows XP (SPSS Inc, Chicago, IL, USA) was used for data analysis. Categorical data was presented as frequencies and percentages, and Pearson’s chi-square test was used to analyse demographic differences between types of eating disorders. For continuous variables, differences between the various eating disorder diagnoses were compared using one-way analysis of variance and Tukey post-hoc tests, with statistical significance set at p < 0.05.
RESULTS
A majority of participants were women and of Chinese ethnicity (
Table I
Demographics of individuals diagnosed with eating disorders (n = 257).
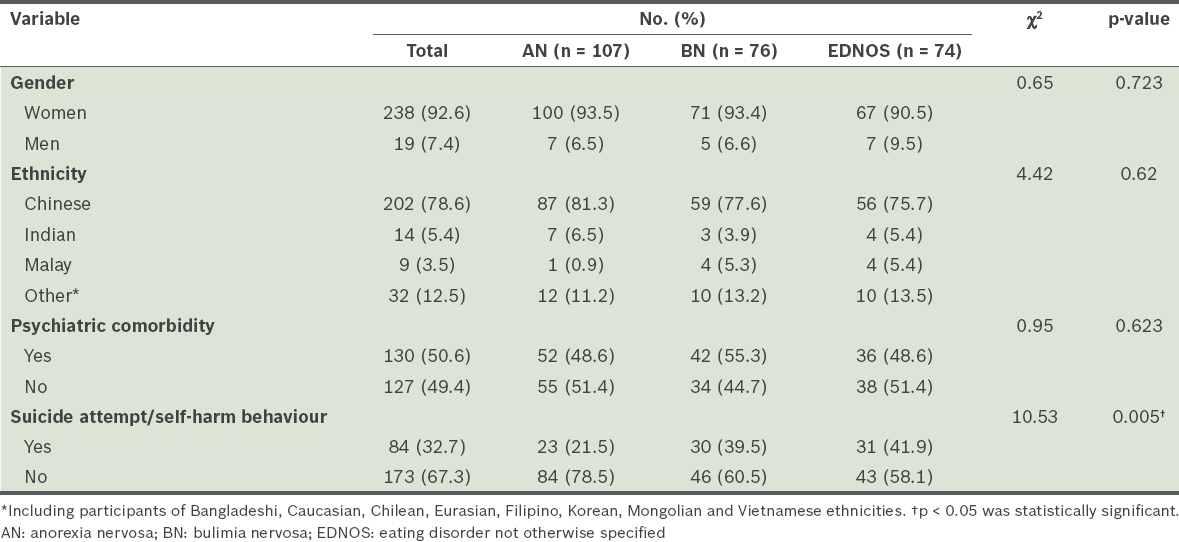
Eating disorder diagnoses among our participants included AN (41.6%), BN (29.6%) and EDNOS (28.8%). About half of our participants had at least one psychiatric comorbidity, with the top three conditions being major depressive disorder (63.8%), obsessive compulsive disorder (5.4%) and some form of anxiety disorder (4.6%). Other comorbid psychiatric conditions included bipolar disorder, personality disorder, adjustment disorder, substance abuse, alcohol dependence, conduct disorder, gender identity disorder, post-traumatic stress disorder, panic disorder, attention deficit and hyperactivity disorder, and the presence of depressive and/or anxiety traits. About a third (32.7%) of our participants had a history of suicide attempts and/or self-harm. Participants with the diagnoses of BN and EDNOS were more likely to have a history of suicide attempt or self-harm behaviours compared to those diagnosed with AN (p = 0.005). However, there were no statistically significant differences between the diagnostic groups in terms of ethnicity and comorbid psychiatric conditions. Participants with BN were more likely to have a comorbid psychiatric condition when compared to participants with other eating disorder diagnoses, although the difference did not reach significance. Some (n = 83, 32.3%) participants had a medical complication related to eating disorder, and approximately half of these participants were diagnosed with AN. The top three medical complications were bradycardia (n = 34), low bone density for chronological age (n = 18) and gastritis (n = 15). However, there was no statistically significant difference between the diagnostic groups for the occurrence of medical complications (p = 0.158).
The mean age at presentation of our study cohort was 20.52 ± 7.14 years (
Table II
Characteristics of individuals diagnosed with eating disorders.
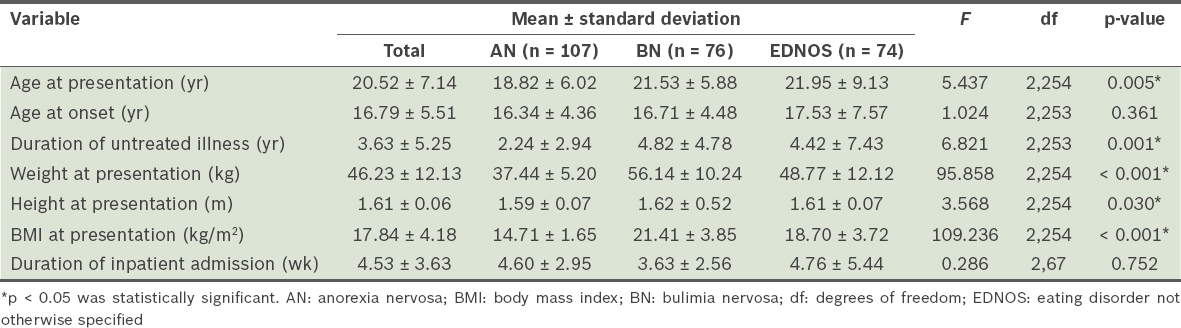
The mean body mass index (BMI) was 17.84 ± 4.18 kg/m2 and participants with AN presented with a significantly lower BMI (14.71 ± 1.65 kg/m2) than those with BN and EDNOS (F(2,254) = 109.236; p < 0.001), as expected. A Tukey post-hoc test also found that participants with EDNOS (18.70 ± 3.72 kg/m2) presented with a significantly lower BMI when compared to those with BN (21.41 ± 3.85 kg/m2; p < 0.001) (
The mean CIA and EDE-Q scores of participants are presented in
Table III
CIA and EDE-Q scores of individuals diagnosed with eating disorders (n = 257).
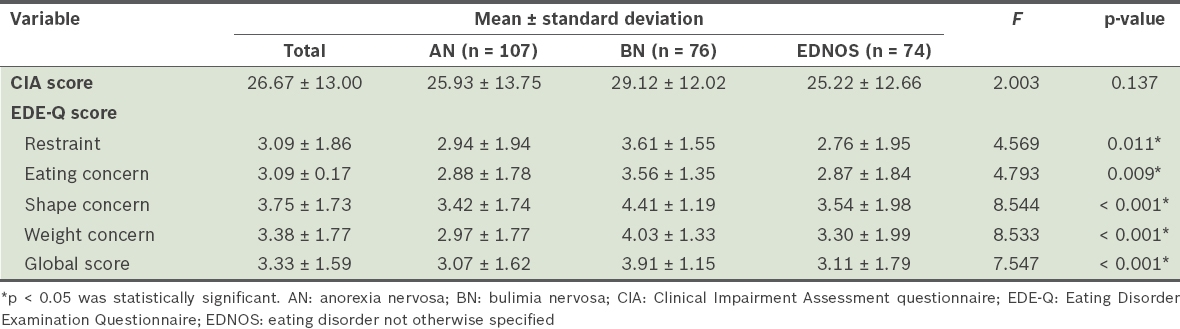
Similarly, when the shape concern scores were compared, although no significant differences were seen between the AN and EDNOS groups, the BN group had a significantly higher shape concern score when compared to the other groups (F(2,254) = 8.544; p < 0.001). A Tukey post-hoc test showed that the BN group had a significantly higher shape concern score of 4.41 ± 1.19 when compared to the AN (3.42 ± 1.74; p < 0.001) and EDNOS (3.54 ± 1.98; p = 0.005) groups (
These findings suggest that participants with BN experienced a higher intensity of eating disorder psychopathology in all domains of EDE-Q when compared to those with AN and EDNOS. Thus, it is not surprising that the BN group’s mean EDE-Q global score was also significantly higher than that of the AN and EDNOS groups (F(2,254) = 7.547; p < 0.001). As earlier, post-hoc Tukey tests revealed that the BN group had a higher EDE-Q global score (3.91 ± 1.15) when compared to the AN (3.07 ± 1.62; p = 0.001) and EDNOS (3.11 ± 1.79; p = 0.005) groups, but no significant difference was seen in the mean EDE-Q global scores between the AN and EDNOS groups (
DISCUSSION
As of June 2014, the Singapore population was 5.47 million, and its ethnic profile was 76.2% Chinese, 15.0% Malay, 7.4% Indian and 1.4% others.(22) The proportion of Chinese participants (78.6%) in our sample appeared to reflect the demographic distribution of the general Singapore population. However, this was not so for participants of other ethnicities – the Malay ethnicity was under-represented (study sample 3.5% vs. Singapore population 15.0%) while other ethnicities were over-represented (study sample 12.5% vs. Singapore population 1.4%). The over-representation of individuals of other ethnicities in our clinical sample was expected, as the treatment programme at our hospital receives referrals from overseas centres. Among participants categorised as ‘others’ in our study, nearly half were Caucasian. Another possible explanation for the over-representation of other ethnicities may be the lower stigma associated with consulting psychiatrists in Western culture, and thus, more individuals of Caucasian ethnicity may be willing to seek help at our centre.(23)
Similar to previous studies,(24) we found consistent under-representation of Malay and Indian ethnicities in our sample. In a study of 50 individuals with eating disorders treated at another general hospital in Singapore between 1991 and 1996, the ethnic make-up of patients of Malay and Indian ethnicities was both low at 10%.(25) These findings were not in agreement with an earlier study of over 4,000 Singaporean women, in which 20.6% of Malay women and 9.4% of Indian women were found to be at risk of developing eating disorder.(26) It was previously suggested that the Malay and Indian cultures may be protective factors against the development of eating disorder due to lower emphasis placed on the thin ideal therein.(7) The under-representation of Malay ethnicity in our sample could also be explained by the lower likelihood of Malay individuals seeking help for psychiatric illnesses.(27,28) To our knowledge, there is currently no literature on the help-seeking behaviour of the Indian community in Singapore. However, it was reported that Indian women in the United Kingdom were less likely to seek help for psychiatric illnesses compared to their Caucasian counterparts(29) because of the lack of knowledge about associated conditions and the belief that treatment would not be beneficial. We may extrapolate such theories to the Indian community in Singapore. Poor eating disorder literacy in Singapore could also be a compounding factor.(30) Future studies on the characteristics of eating disorders and cultural factors that influence eating disorders among individuals of Malay and Indian ethnicities would be of value.
Our study reported a significantly shorter DUI among participants with AN compared to those from the other diagnostic groups. Against the background of poor eating disorder literacy in Singapore,(30) it is likely that individuals with AN may have presented to the clinic only because of telling signs such as severe weight loss and physical manifestations of medical complications, while those with BN or EDNOS might have sought help only after a longer duration. Participants with AN in our study presented at a significantly younger age compared to those with BN and EDNOS (AN 18.82 ± 6.02 years, BN 21.53 ± 5.88 years, EDNOS 21.95 ± 9.13 years; p = 0.005), in keeping with studies from the United Kingdom.(31,32)
Participants with BN and EDNOS in our study had higher rates of suicide attempts and self-harm behaviour when compared to those with AN (p = 0.005). The BN diagnostic group also had higher rates of comorbid psychiatric conditions, although this did not reach statistical significance (p = 0.623). Our findings mirror studies from the United States – one study reported elevated rates of self-harm and substance use among patients with BN and binge eating disorder,(33) while another concluded that BN patients with a family history of drug abuse were more likely to have been treated for drug abuse problems themselves.(34) The higher rates of comorbid psychiatric conditions and self-harm behaviour among individuals with BN and EDNOS in our sample could be extrapolated to explain the need for hospitalisation, even though treatment for such patients is usually outpatient-focused.
In our study, the longer DUI among individuals with BN could explain the higher levels of eating disorder psychopathology seen among these individuals when compared to those with AN and EDNOS. Participants with AN were also closer to the adolescent age group when compared to those with BN and EDNOS. This finding echoes a previous study in which adolescents with AN tended to report lower scores of eating psychopathology, as symptoms tended to be ego-syntonic and were not recognised as pathological.(35) Although the BN group scored highest in all domains of the EDE-Q with a high corresponding CIA score, the latter did not reach statistical significance, suggesting that higher EDE-Q scores did not necessarily translate to higher levels of psychosocial impairment. This could be attributed to individuals with AN presenting with very low body weights that required longer periods of hospitalisation when compared to those with BN, possibly contributing to a degree of psychosocial impairment.
The EDE-Q subscale scores in our study were similar to those found in earlier studies,(11,13) which may imply that there was a consistent trend from 2007 to 2012 for body image concerns and eating psychopathology in our local population. The profile of participants in our study was also similar to the Singapore arm of studies by Soh et al(11,13) in terms of gender and ethnicity distributions, and average age and BMI at presentation, suggesting that the demographic characteristics of new presentations have not shifted much over the years. Although these studies had a small sample size of Singaporean Chinese patients, they were the only local studies with which we could compare our cohort.
Eating disorders were thought to be an illness associated with people of North European Caucasian ethnicity and considered relatively rare outside of Western countries. However, examining the eating disorders in our local population allows us to compare and contrast the underlying psychopathology with that of overseas centres. Comparisons with other studies of similar design suggest that our participants scored lower than their overseas counterparts(11,36-39) in most EDE-Q subscales. Compared to a study from the United Kingdom,(37) which reported an EDE-Q restraint subscale score of 3.57 (± 1.41) and EDE-Q weight concern subscale score of 2.67 (± 1.44), our participants scored lower in the respective subscales. Similarly, when compared to a study from Sweden,(38) which reported EDE-Q scores of 3.67 (± 1.60) for restraint, 3.36 (± 1.34) for eating concern, 4.72 (± 1.32) for shape concern, 4.07 (± 1.39) for weight concern and 4.06 (± 1.20) for global score, our participants scored lower in all subscales. In comparison with an Australian study(11) that reported 3.2 for restraint, 4.5 for shape concern, 3.9 for weight concern and 3.8 for global score, our cohort reported lower restraint, shape concern, weight concern and global EDE-Q scores but had similar CIA scores.(39) These differences in scores may be explained by the higher proportion of patients with AN having low body weight in our sample, while the other quoted studies included older participants who had BN and EDNOS as major diagnoses.(36-39)
We compared our scores differentially with one American study(40) that reported the EDE-Q scores for patients with AN and BN. Their study comprised a sample of AN patients with mean BMI of 16.49 kg/m2 who scored 1.7 (± 1.98) for restraint, 1.39 (± 1.43) for eating concern, 1.88 (± 1.84) for weight concern and 2.21 (± 1.95) for shape concern subscales on the EDE-Q. Their sample of BN patients reported 4.50 (± 1.16) for restraint, 4.40 (± 1.16) for eating concern, 4.81 (± 1.39) for weight concern and 4.95 (± 1.19) for shape concern. In comparison, individuals who had AN in our study scored higher in all EDE-Q subscales, while those with BN scored lower in all subscales. Individuals with AN also presented with lower mean BMI. Indeed, EDE-Q scores and perceived societal norms for eating behaviours and body image can vary between countries and cultures.(38) From our comparisons, we can perhaps extrapolate that when compared to their overseas counterparts, individuals with AN in Singapore experienced higher levels of eating disorder psychopathology, whereas those with BN did not. Further evaluation of other studies with EDE-Q and CIA scores specific to each diagnostic group is needed to lend more weight to these findings.
Our study was not without limitations. First, retrospective recall of information was part of our study design, particularly for the scoring of the EDE-Q and CIA questionnaires. Second, the EDE-Q and CIA questionnaires have not yet been validated for the Singapore context. Nonetheless, they remain useful for measuring the degree of eating disorder psychopathology in the Singapore clinical population. Third, our eating disorder treatment programme caters not only to adults but also underage patients. It is possible that some participants were reluctantly taken to treatment by their parents and that the severity of their symptoms was downplayed, falsely influencing the EDE-Q and CIA scores reported. Fourth, participants were diagnosed based on the clinical assessment of the treating psychiatrist rather than by using a validated diagnostic tool. Fifth, given that our data was collected from a single centre and there was under-representation of the Malay and Indian ethnicities when compared to the general Singapore population, the generalisability of our findings could be questioned. These shortcomings notwithstanding, our study still represents a valuable addition to the existing literature on individuals with eating disorders in Singapore.
Our findings suggested that the eating psychopathology of our local population, which appeared unchanged over time, still differed from that of a Caucasian population. Significant findings were: (a) under-representation of Malay and Indian ethnicities; (b) participants with AN presented earlier in the course of illness, had lower rates of self-harm behaviours, and scored lower in the EDE-Q and CIA subscales; and (c) participants with BN reported high scores in all domains of the EDE-Q. These findings suggest the need for an individualised approach when treating individuals with eating disorders, taking into account the possible effects of ethnicity and cultural differences. Nevertheless, ethnic and cultural practices could also be tapped into as complements that may aid in a patient’s recovery. Future studies that look into how ethnicity and cultural factors impact the course of eating disorders would be valuable.


