Dear Sir,
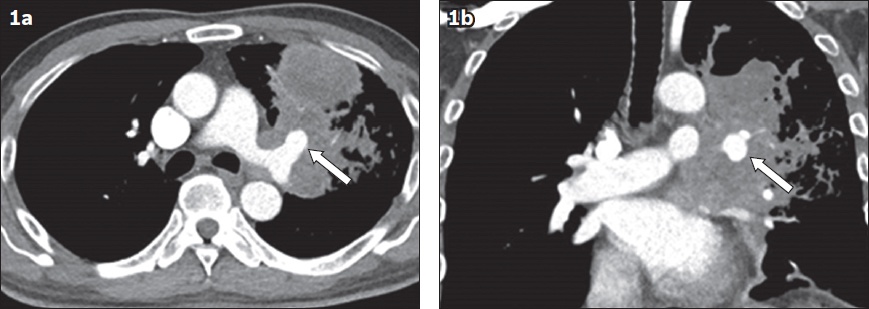
We herein describe the case of a 59-year-old Chinese man with a history of Stage IV squamous cell carcinoma of the lung, which was recently diagnosed in January 2017. He was referred to our department after presenting with massive haemoptysis (140 mL). At the time, his oxygen saturation was 94%, heart rate 136 beats per minute, blood pressure 97/59 mmHg and haemoglobin level 8.4 g/dL. Computed tomography (CT) pulmonary angiography showed a pulmonary artery pseudoaneurysm (PAP) of the left upper lobe pulmonary artery, which measured 1.9 cm × 1.4 cm × 1.7 cm and was encased by the large left upper lobe mass (
Fig 1
(a) Contrast-enhanced axial CT pulmonary angiogram shows the left upper lobe pulmonary artery pseudoaneurysm (arrow) encased by the left upper lobe mass. (b) Coronal image shows the height of the pseudoaneurysm (arrow).
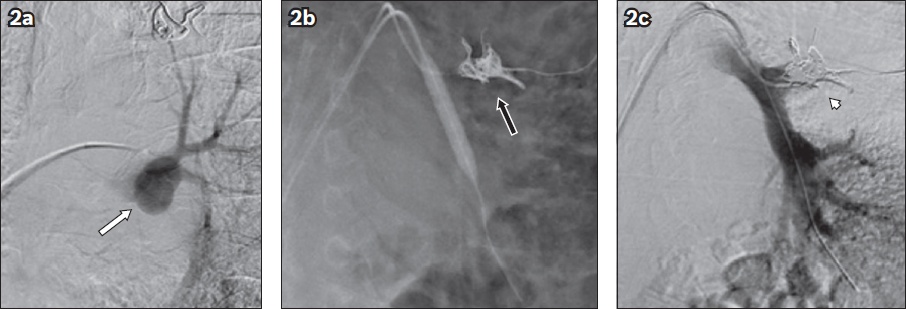
The patient then underwent balloon-assisted coiling of the pseudoaneurysm and the left upper lobe pulmonary artery. A 8 mm × 4 cm balloon (Mustang™; Boston Scientific, Natick, MA, USA) was inflated across the left pulmonary artery bifurcation via an 8-French (Fr) long sheath (BRITE TIP™; Cordis, Hialeah, FL, USA). The aneurysm was subsequently packed with one 14 mm × 60 cm and two 16 mm × 60 cm detachable coils (Ruby®; Penumbra Inc, Alameda, CA, USA), introduced by a 2.7-Fr microcatheter (PROGREAT®; Terumo, Tokyo, Japan) via the same 8-Fr sheath (Figs.
Fig 2
Pulmonary artery angiogram shows (a) the left upper lobe pulmonary artery pseudoaneurysm (arrow) and (b) the deployment of Ruby coils with the assistance of an 8-mm balloon (black arrow). (c) Post-embolisation digital subtraction angiogram shows no flow into the left upper lobe pulmonary artery (arrowhead).
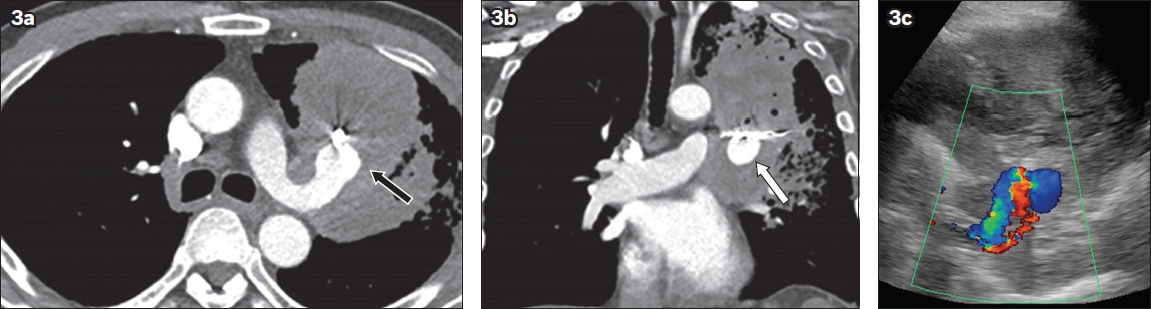
However, the haemoptysis recurred eight days later. Repeat CT pulmonary angiography demonstrated flow and an interval increase in the size of the left upper lobe PAP, now measuring 2.3 cm × 2.2 cm × 2.0 cm (Figs.
Fig 3
(a) Contrast-enhanced axial CT pulmonary angiogram shows an interval increase in size of the left upper lobe pulmonary artery pseudoaneurysm (black arrow). (b) Coronal CT pulmonary angiogram shows the interval increase in height of the pseudoaneurysm (white arrow). (c) Transthoracic Doppler US image shows persistent flow in the pulmonary pseudoaneurysm.
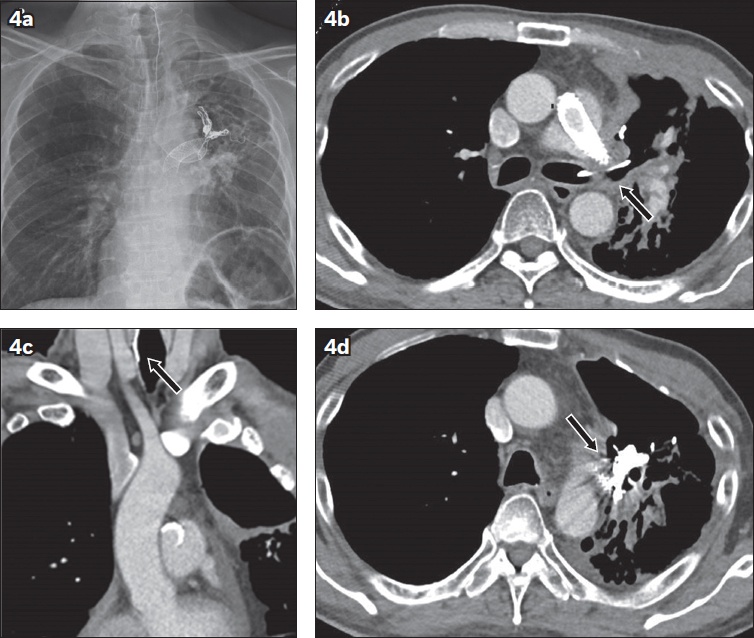
Nine months later, the patient presented with fever, cough and blood-stained sputum. Chest radiography showed further retraction of the stent and migration of a coil up the trachea, indicating fistulisation of the coil through the tumour and into the bronchus (
Fig 4
(a) Chest radiograph shows migration of an uncoiled portion of the embolisation coil superiorly into the neck. (b) Contrast-enhanced axial CT image shows protrusion of the embolisation coil into the left main bronchus (arrow). (c) Coronal CT image shows that the upper margin of the coil is located in the trachea but the tip cannot be visualised in this study (arrow). (d) Axial image shows that the pulmonary artery pseudoaneurysm is partially thrombosed(arrow).
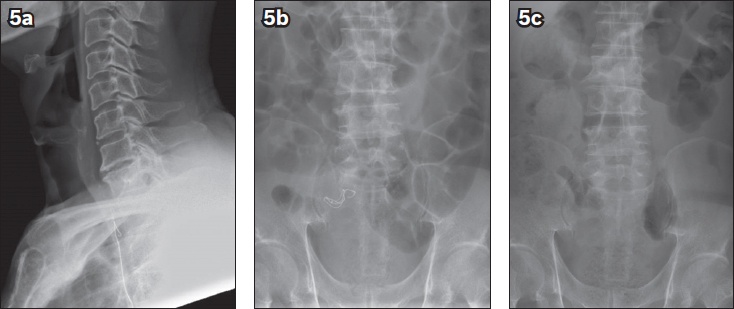
While bronchoscopic retrieval was an option, we elected to manage this conservatively, as the patient remained asymptomatic apart from a mild globus sensation. Lateral neck radiography performed the following day showed that the coil had been swallowed and was in the oesophagus (Fig. 5a). Subsequent radiographs showed that the coil moved through the bowel and was eventually passed out (Figs.
Fig 5
(a) Lateral neck radiograph shows migration of the coil from the trachea into the upper oesophagus. (b) Abdominal radiograph taken the following day shows interval migration of the coil from the upper oesophagus into the lower abdomen. (c) Abdominal radiograph taken seven days later confirms that the coil is no longer visualised.
PAP can lead to potentially life-threatening haemoptysis, especially when it occurs within a consolidated area of lung where the potential for tissue breakdown is high, and can lead to uncontrolled rupture. Swift and accurate diagnosis is crucial because the mortality rate associated with a ruptured PAP can be as high as 50%.(1) The prevalence of PAPs ranges from 5% to 11% in those presenting with haemoptysis and who underwent either bronchial or pulmonary angiography, or both.(2) To our knowledge, only five previous reports have been published on spontaneous PAPs arising within primary lung neoplasms, with four of these five cases involving squamous cell carcinomas.(3-7)
Various embolisation techniques for PAPs have been described in the literature. They usually involve either coil embolisation of the arterial branch supplying the aneurysmal sac(8) or filling of the sac itself with coils.(9) Embolisation has also been accomplished with detachable silicone balloons, gelfoam, polyvinyl alcohol particles, N-butyl cyanoacrylate glue(10) and plug embolisation devices.(11) Reports of the use of covered stents are rare and, to our knowledge, none have been described for a PAP.(12) Ultimately, the choice of embolisation technique used depends on the site, type and anatomy of the pseudoaneurysm and also the comfort, ability and experience of the interventionist. Embolisation-related complications in the context of pseudoaneurysms are infrequently encountered and mainly consist of coil migration, damage to the vessel wall and delayed bacterial contamination of the thrombus.(13) In the literature, there were only two reported cases of coil extrusion following embolisation procedures involving the pulmonary arteries, and both patients underwent a lobectomy.(14,15)
Considering that a pseudoaneurysm does not possess a true intact wall, any interventional procedure for pseudoaneurysm repair is at risk of primary failure, especially if it involves coil deployment, which may easily penetrate the weak wall. Our case report demonstrates the difficulty of treating PAPs. It is our view that deploying a covered stent in this region may yield unexpected results due to the aforementioned reasons, and this patient may have benefited from embolisation of the entire left pulmonary artery after the initial failure. Secondly, we demonstrated that procedure-related complications such as coil migration may be managed conservatively if the coil is extruded via the aerodigestive tract, as long as the haemoptysis does not recur and the patient remains hemodynamically stable. Finding the most suitable embolisation agent that is both effective in treating a pseudoaneurysm and has a low risk of complications remains a challenge.
Yours sincerely,


