Dear Sir,
A 45-year-old man had an industrial accident in which a metallic foreign body penetrated his left orbit transcutaneously. Following failed attempted endoscopic removal at the referring institution, the patient was sent to our institution for assessment and management. On the initial formal review by the ophthalmology team, the patient had best-corrected Snellen visual acuity of 6/7.5. He complained of intractable diplopia secondary to complete third, fourth and sixth nerve palsies. There was a Grade 1 Marcus Gunn pupil on examination. The remainder of the ophthalmic examination was unremarkable, particularly the anterior and posterior pole examination. A healed cutaneous entry wound was noted in the superior eyelid. Computed tomography of the orbits demonstrated a large intraconal foreign body in the posterior orbit adjacent to the superior orbital fissure and the orbital apex (
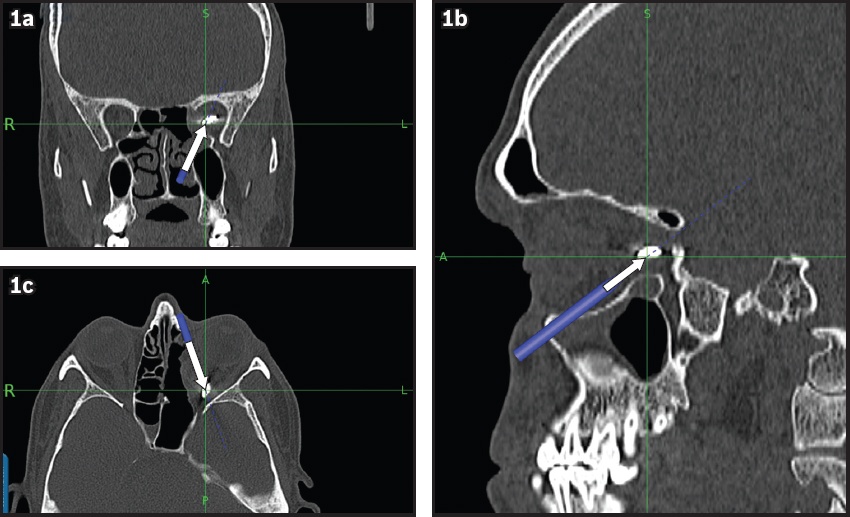
Fig. 1
Image-guidance reformatted CT image in (a) coronal, (b) sagittal and (c) axial views shows the large intraconal metallic foreign body (arrows) in all three planes. Proximity to the optic nerve and extraocular musculature is observed.
The patient was reviewed by the otolaryngology and oculoplastic surgery teams. Intravenous antibiotics (ceftriaxone 1 g twice a day) were started and continued for the duration of his two-day admission. A decision was made to attempt endoscopic removal, with consent to proceed to medial lid-split and/or lateral orbitotomy if required. Risks including blindness and persistent diplopia were discussed with the patient.
The lamina papyracea was removed completely and slings were placed around the medial and inferior recti muscles for retraction. A nasal septectomy was performed to further improve retraction. The inferior boundary of the orbital apex was drilled, creating a trajectory between the medial and inferior recti. Despite the use of image guidance, the object proved difficult to locate due to the mobile nature of intraorbital structures. As there was concern about migration, intraoperative radiography was employed to confirm the position of the object (
Fig. 2
Intraoperative radiograph shows a Weil-Blakesley forceps positioned within the orbital apex to confirm the location of the foreign body.

Fig. 3
Photograph shows the metallic, crescent-shaped foreign body (9 mm × 10 mm × 3 mm) that was retrieved from our patient.

The patient was discharged the following day on oral and topical antibiotics (augmentin one tablet twice a day for two weeks and chloramphenicol eye ointment one application to the left eye three times a day for 30 days). Visual acuity was preserved and there was gradual improvement in his diplopia due to resolving orbital apex oedema. At the three-month postoperative review, visual acuity was preserved at 6/7.5 in the affected eye, ocular motility was improved, with residual palsy of the superior branch of the third cranial nerve, and partial fourth and sixth nerve palsies, that resulted in persistent binocular diplopia.
Foreign bodies situated in the orbital apex are rare and may be associated with significant ocular and orbital injury, especially if the foreign body is a metallic projectile.(1,2) More posteriorly located foreign bodies are associated with worse injuries.(1) Most cases involve young male patients, often while they are working on industrial sites.(1,3) Some cases may be indolent and present after several months.(3) Complications of intraorbital foreign bodies include blindness, orbital or cerebral abscess, limited extraocular motility, proptosis, ptosis, cellulitis, orbitocutaneous fistula and osteomyelitis.(3)
Surgery to remove orbital foreign bodies is not without risks. These include failure to locate the foreign body, fragmentation during removal causing collateral damage, and inadvertent injury to orbital structures including the optic nerve and extraocular muscles. Some authors may therefore advocate ‘watchful waiting’ as an option for inert foreign bodies not causing significant symptoms. However, others believe that clinical suspicion or radiological confirmation should prompt surgical exploration, with most patients achieving visual improvement following removal of the foreign body.(3)
The traditional approach to foreign bodies in the orbital apex is a lateral orbitotomy. With the advent of minimally invasive endoscopic sinus surgery, authors began describing successful endonasal removal two decades ago; however, most of these foreign bodies lay partially within the paranasal sinuses.(4) For foreign bodies with or without a sinonasal component, a combined approach with a lateral orbitotomy and endoscopic sinus surgery is an option.(5,6) In 2009, Koo Ng et al reported the successful removal of an orbital apex foreign body with an entirely transnasal approach.(7)
To our knowledge, there are only a few published cases in the literature in which an orbital apex foreign body abutting the optic nerve is successfully removed in an entirely endoscopic procedure. We found that while image-guidance computed tomography may be useful for fixed bony anatomy, real-time imaging with plain radiography proved to be more useful in navigating the intraorbital space due to the mobile nature of its contents.
Yours sincerely,


