Abstract
INTRODUCTION
The stillbirth rate (SBR) is an important public health indicator. We studied the distribution of maternal and fetal characteristics and time trends of the SBR at KK Women’s and Children’s Hospital (KKH), Singapore, from 2004 to 2016 based on various definitions of stillbirth.
METHODS
Data was obtained from the Data Warehouse and Stillbirth Reporting System of KKH from 2004 to 2016. SBRs were calculated based on three definitions (fetal deaths at ≥ 20 weeks, 24 weeks or 28 weeks of gestation per 1,000 total births) and were described with maternal and fetal characteristics, and by year.
RESULTS
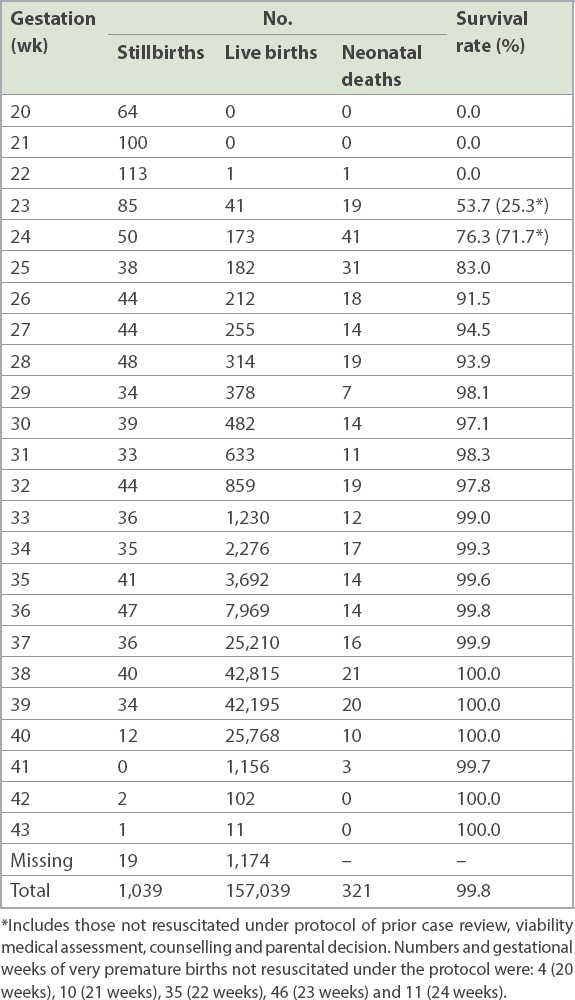
From 2004 to 2016, the SBR declined by 44.7%, 25.5% and 18.9% based on Definitions I, II and III, respectively. The SBR at KKH in 2016 was 5.2 (Definition I), 4.1 (Definition II) and 3.0 (Definition III) per 1,000 total births. The SBR was significantly higher in women aged ≥ 35 years, nulliparas and female fetuses. The number of live births at 24–27+6 weeks of gestation was more than four times higher than that of stillbirths (822 vs. 176). There were 104 (12.7%) neonatal deaths during this gestation period, giving a high survival rate of 87.3%.
CONCLUSION
The SBR in KKH is relatively lower than that in other developed countries. There is a need to consider revising our hospital and national definitions of the stillbirth lower boundary from 28 weeks to 24 weeks of gestation. This would allow us to make better comparisons with other developed countries, in line with improvements in healthcare.
INTRODUCTION
Stillbirth rates (SBRs), including antepartum and intrapartum fetal deaths, are important public health indicators and directly reflect the quality of care provided to women during pregnancy and the peripartum period. For decades, neonatal death has attracted most attention worldwide,(1-3) but stillbirth, particularly the antepartum fetal death, has been understudied. Antepartum fetal death accounts for approximately half of stillbirths in developing countries and nine-tenths in developed countries.(4) Many countries do not have vital statistics reporting systems. Even in some developed countries, stillbirths, especially at an earlier gestational age,(5) are frequently under-reported. In surveys, stillbirths are frequently combined with early neonatal deaths and reported as perinatal mortality. The combination may mask reporting differences, systematic misclassification, variation in trends and different solutions.(6)
In developed countries, the main prevention strategy for antepartum fetal death involves identification of stillbirth risk factors, such as maternal diabetes mellitus, preeclampsia, fetal distress, intrauterine growth retardation and postdate pregnancies, and timely delivery by induction of labour or Caesarean section.(7) Unfortunately, these strategies have not been very successful in reducing antepartum fetal death, compared to the efforts to reduce intrapartum fetal death. This may explain the approximately tenfold greater prevalence of antepartum fetal deaths in developed countries compared to intrapartum fetal deaths.(8)
In addition, stillbirth is often inconsistently defined with regard to the lower boundary of gestational age. Some studies showed that moving from a 28-week to a 22-week threshold can lead to a 40% increase in the number of stillbirths.(9,10) The variation in the thresholds not only causes misunderstanding about the SBR but also may impede international comparisons.
Singapore is a developed country and has had a low SBR for decades.(11) However, the lower boundary of gestational age for stillbirth remains at 28 weeks of gestation. This is in contrast to other developed countries, such as the United Kingdom (UK), the United States (USA) and Australia, where the boundary of gestational age for stillbirths has been lowered (24 weeks in the UK and 20 weeks in the USA and Australia). Our institution, KK Women’s and Children’s Hospital (KKH), is the largest women and children’s hospital in Singapore, accounting for approximately one-third of all births locally. In May 2001, an extended stillbirth reporting system was introduced. Fetal deaths (stillbirths) at 20 weeks of gestation or more have been recorded since then, which makes it possible to estimate an SBR that is compatible with rates in other developed countries.
Our study aimed to (a) present the distribution of maternal and fetal characteristics and the time trends of SBR at KKH from 2004 to 2016 according to different definitions of stillbirth; (b) examine risk factors for stillbirths; and (c) compare our SBR with those of other developed countries.
METHODS
Data was extracted from the hospital clinical database, Data Warehouse and KKH Extended Stillbirth Reporting System. A total of 1,538 cases from 2004 to 2016 were extracted for possible inclusion. We excluded 14 fetal deaths whose gestational age was less than 20 weeks, 12 fetuses with poor-quality data and 367 abortus from social terminations of pregnancy. We also excluded 106 cases of severe prematurity born with very dismal prospect of viability where, after review, assessment and counselling, it was decided prior to or immediately after delivery that resuscitation would be futile in view of very extreme prematurity (20–23+6 weeks’ gestation) and poor medical condition. In general, resuscitation guidelines at KKH for previable gestations (20–22+6 weeks’ gestation) and borderline viability (23–24+6 weeks’ gestation) deliveries are based on recommendations by the Nuffield Council on Bioethics.(12) Live births from 20 to 22+6 weeks’ gestation are provided comfort care until death. At 23–24+6 weeks’ gestation, parents are counselled prior to delivery by a multidisciplinary team of neonatologists and obstetricians (i.e. High Risk Consult perinatal team) regarding the decision for resuscitation. Statistics based on survival and morbidities(13,14) and the obstetric and fetal conditions are shared with parents. Based on the parental decision, live births at these gestations are resuscitated or provided comfort care. Of the live births in the present study, 46 at 23–23+6 weeks’ gestation and 11 at 24–24+6 weeks’ gestation, respectively, were provided comfort care according to the parental decision. Therefore, 1,039 stillbirths were included in the final analysis.
The database contained information on maternal demographic characteristics such as maternal age, maternal age group (< 20 years, 20–24 years, 25–29 years, 30–34 years and ≥ 35 years) and ethnicity (Chinese, Malay, Indian and Others), as well as pregnancy information, including gestational age (20–23+6 weeks, 24–27+6 weeks and ≥ 28 weeks), parity (0 previous birth or ≥ 1 previous births) and fetal gender (male or female).
We used three different stillbirth definitions. Definition I was fetal deaths at ≥ 20 weeks of gestation per 1,000 total births. If data on gestational age was missing, fetal deaths whose birth weights were ≥ 400 g were included. Definition II was fetal deaths at ≥ 24 weeks of gestation per 1,000 total births. If data on gestational age was missing, fetal deaths whose birth weights were ≥ 500 g were included. Definition III was fetal deaths at ≥ 28 weeks of gestation per 1,000 total births. If data on gestational age was missing, fetal deaths whose birth weights were ≥ 1,000 g were included.
Maternal and fetal characteristics were expressed as numbers and percentages for categorical variables. Logistic regression was used to examine the risk factors for stillbirth. Maternal age, ethnicity, parity, fetal gender, weeks of gestation and delivery years were included in the logistic regression model. Chi-square test for trend was performed to examine the SBR trend by years. All analyses were conducted using IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA). This study was approved by the ethics committee at KKH.
RESULTS
The total number of obstetric deliveries at KKH between 2004 and 2016 was 157,039. In the same period, there were 1,039 stillbirths at 20 weeks of gestation or more. The average maternal age was 30.6 ± 5.9 years, median birth weight was 722 (interquartile range 475–1,732) g and median gestational age was 27 (interquartile range 22–33) weeks.
Table I
Distribution of live births and stillbirths at ≥ 20 weeks of gestation by maternal and fetal characteristics.
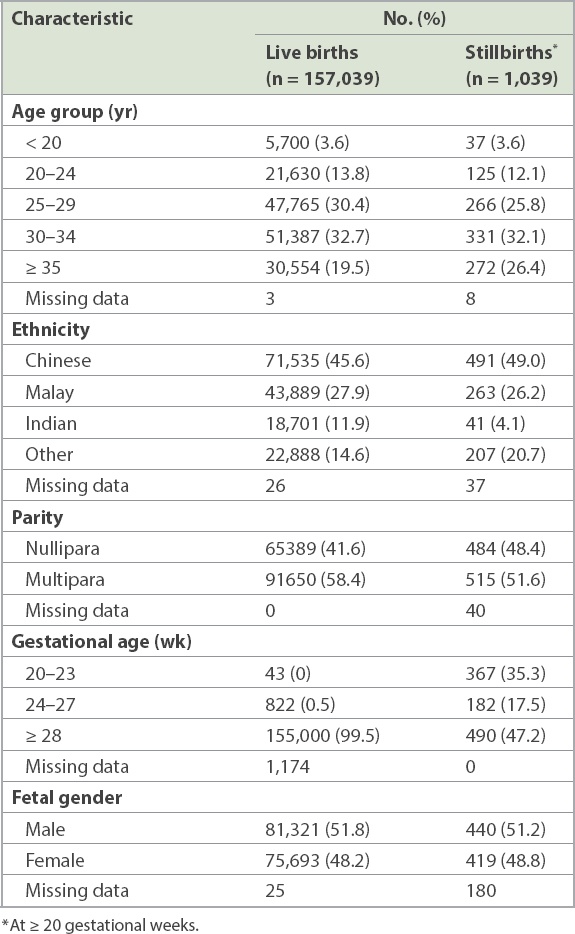
The SBR was significantly higher in women aged ≥ 35 years across the different definitions of SBR (
Table II
Stillbirth rate by maternal and fetal characteristics according to three different definitions.
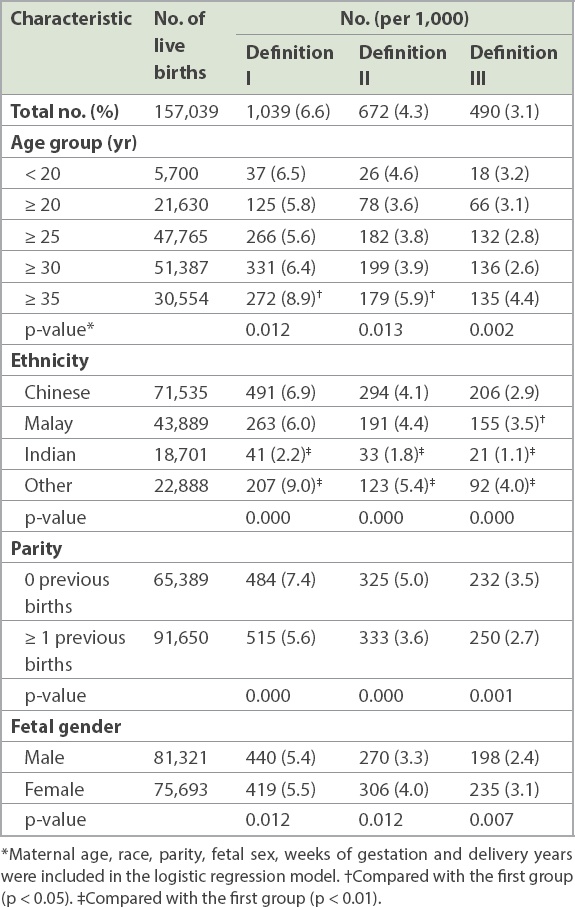
Table III
Stillbirths by number of weeks of gestation from 2004 to 2016.
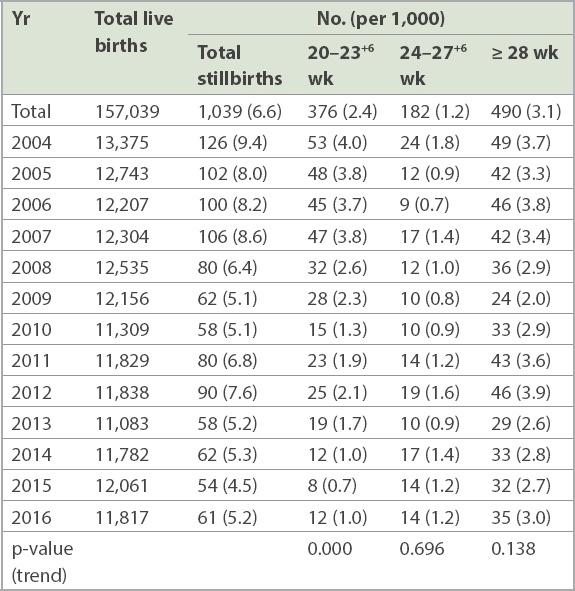
Table IV
Stillbirth rates by definition from 2004 to 2016.
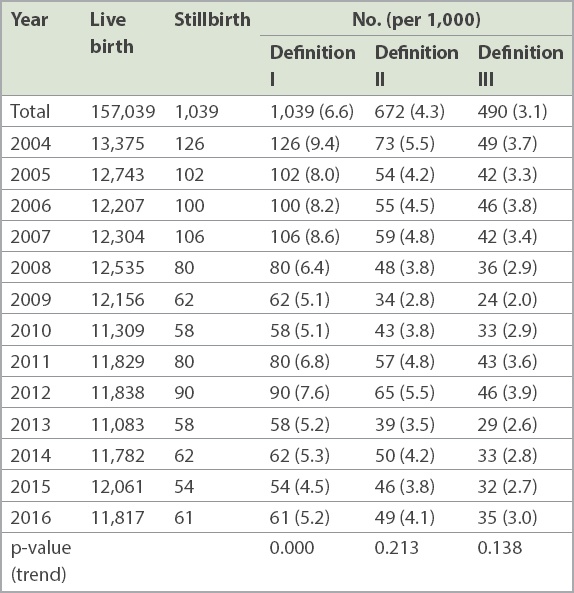
Table V
Survival rates of live births by gestational week.
DISCUSSION
Since May 2001, an extended stillbirth reporting system had been introduced at KKH. Fetal deaths or stillbirths at 20 weeks of gestation or more were reported, and basic maternal and fetal information was collected. Our study presented the epidemiology of stillbirths, allowing us to better understand and assess the SBR at KKH. Using different definitions of SBR permitted a comparison of our SBR with those of other developed countries at appropriate levels, depending on the definitions.
Numerous studies have demonstrated that older maternal age (≥ 35 years old) is an independent risk factor for stillbirth.(15-18) This may be related to the presence of more pregnancy complications in older women, such as hypertension, diabetes mellitus, placental problems and multiple gestation.(19) Apart from these, having a first birth at an advanced maternal age may be another important factor at KKH. Like other high-income countries, an increasing number of women are delaying childbearing in Singapore, leading to a growing proportion of primiparous women who are older than 35 years. According to KKH’s clinical database, the average age of women at first birth in 2015 was 28.8 years, and 11.3% of first-birth mothers were over 35 years of age. Various studies suggested an increased risk of unexplained stillbirth in older women, even after controlling for risk factors such as hypertension, diabetes mellitus, placenta praevia and multiple gestation.(18,20,21) An interaction between first birth and advanced maternal age appeared to increase the risk of stillbirth in primiparous older women.(18) The estimated risk of stillbirth is one in 116 in a 40-year-old nulliparous woman after 37 weeks of gestation, compared with one in 304 in a multiparous woman of the same age.(18) Since more than one-fourth of stillbirths are in this group in KKH, an incidence that is higher than that in the United States (16.3%) and Sweden (19.5%),(18,22) more focus should be given to this group.
A study conducted in the United States showed a racial disparity in SBR that may be contributed by genetics, environment, stress, social issues, access to quality medical care and behaviour.(23) In contrast, Singapore is a multiethnic country, and our study population comprised 45.6% Chinese, 27.9% Malay and 11.9% Indian patients. While Malay patients had a significantly higher SBR than Chinese patients for Definition III (≥ 28 weeks), after adjusting for maternal age, parity, fetal gender, weeks of gestation and delivery years, there was no significant difference in SBR between Chinese and Malay patients for Definitions I and II. Notably, Indians had a significantly lower SBR than Chinese and Malay patients. This may need further investigation, although Indians from different parts of the Indian subcontinent are a heterogenous group, and there may have been classification errors, especially when the ‘Others’ group had a significantly higher SBR.
While the number of male stillbirths was more than that of female stillbirths, there were also more male births in proportion to the total birth population; this is consistent with the typical gender ratio at birth, which is biased towards the male gender. Thus, the male stillbirth rate for Definition I was marginally lower than that of the female stillbirth rate (5.4 per 1,000 births, 440/81,231 vs. 5.5 per 1,000 births, 419/75,693). This statistically significant elevated risk of stillbirth in females, albeit small, is not consistent with overseas studies, which showed an elevated risk of stillbirth in males.(24) As stillbirth data below 28 weeks is not routinely collected in Singapore, this information was hitherto not available, and it can add valuable insights to previous studies on stillbirths, especially those in Singapore that were based on the ‘28 weeks of gestation or more’ definition.(25-29)
Over the past 20 years, SBRs in developed countries have declined at rates of 3.0–6.8 per 1,000.(30,31) It was estimated that the SBR in developed regions was 4.5 per 1,000 in 2000 and 3.4 per 1,000 in 2015 (at ≥ 28 weeks of gestation).(32) The SBR at KKH (at ≥ 28 weeks of gestation) is slightly lower than the average SBR in developed countries. Comparing the SBR using the other two definitions from the United States and England, we found that the crude mean SBR at ≥ 20 weeks of gestation at KKH (5.2 per 1,000 in 2013) was slightly lower than that of the United States (5.96 per 1,000 in 2013),(33) and the SBR at ≥ 24 weeks of gestation in 2016 (4.1 per 1,000) was also lower than that observed in England in 2016 (4.3 per 1,000).(34) The SBR (at ≥ 24 weeks of gestation) in KKH was 3.8 per 1,000 total births in 2015, which was lower than the rate of 4.08 (3.51–4.37) per 1,000 in the United Kingdom but higher than the rate of 2.24 (1.81–2.75) per 1,000 in the Netherlands in 2015.(35) Despite minor fluctuations from 2010 to 2012, SBR using all three different definitions showed downward trends from 2004 to 2016. The average percentage decline per year using the three different definitions was 1.5%–3.4%, which was larger than the global rate (estimated at 1.1% per year at ≥ 28 weeks of gestation).(36)
There was a downward trend in SBR for the three groups (≥ 28 weeks, 24–27+6 weeks and 20–23+6 weeks of gestation), and the trend was statistically significant for the 20–23+6 weeks’ group. This may be related to improved overall obstetric care for all three groups. Other probable reasons for the significant fall in the number of early gestation stillbirths include the fact that voluntary notification was used at KKH. Stillbirths and fetal deaths at 20–27+6 weeks of gestation are voluntarily reported by the staff for the purpose of audit, and such voluntary systems, especially for earlier gestational ages,(5) are prone to under-reporting. This may contribute to the under-ascertainment of cases at later periods, as high rates of voluntary reporting are challenging to maintain. This supports the argument that reporting should be mandatory so that accurate statistics can be obtained. Other possible reasons are the increasing use of interventions at earlier gestation periods such as cervical cerclage at 20–23+6 weeks (which would prolong gestation beyond 24 weeks); the increasing use of early prenatal diagnosis leading to earlier termination of pregnancy for lethal fetal anomalies diagnosed in the later first trimester and early second trimester; and the increasing use of social termination of pregnancy for pregnancies with complications, especially at 20–23+6 weeks’ gestation before the legal limit of 24 weeks’ gestation.
The total number of live births at KKH at 24–27+6 weeks of gestation was 822 (more than four times the number of stillbirths for the same period) from 2004 to 2016, of which there were 104 (12.7%) neonatal deaths from this group, thus giving a high survival rate of 87.3%. Moving from a 28-week to a 24-week threshold would lead to an approximately 37% increase in the number of stillbirths (adding 182 more cases to the 490 cases in 2004–2016), similar to international rates.(9,10)
It is noteworthy that in Singapore, reporting of stillbirths at ≥ 28 weeks of gestation is mandated by law. KKH’s extended reporting system for stillbirths and fetal deaths at 20–27+6 weeks of gestation is based on voluntary reporting by staff for audit purposes. This study showed that KKH experienced a significant decline in SBR from 2004 to 2016. Its SBR has been low compared to that in other developed countries. The information that would be derived from extending the definition of stillbirths is substantial. Singapore is now a developed country with good socioeconomic and health statistics. KKH has excellent perinatal care that is comparable to some of the best in the world, with a high survival rate of 87.3% for births in the 24–27+6 group. It may be appropriate to consider revising national and hospital definitions to be in line with those of developed countries.(37) Extended perinatal mortality reporting on a routine basis would allow us to better compare perinatal performance and statistics at all levels.
High-quality data and comprehensive information are very important for evaluating the SBR and comparing it with those of other countries. We found that the current extended stillbirth reporting system at KKH was useful, necessary and feasible, and can be adopted and adapted by other institutions across the country.
About the First Author

Prof Tan Kok Hian is a Senior Consultant in Maternal Fetal Medicine and Head of Perinatal Audit and Epidemiology at KK Women’s and Children’s Hospital (KKH), Singapore. His special interests are prenatal diagnosis and perinatal epidemiology. Prof Tan received the World Health Organization United Arab Emirates Health Foundation Prize as KKH Integrated Perinatal Care Project Team Leader in 2019 and the Singapore Inaugural National Outstanding Clinical Quality Activist Award in 2010. He was conferred the Benjamin Henry Sheares Professorship by Duke-NUS Medical School for his outstanding contributions in Obstetrics and Gynaecology since 2019. He has led national evidence-based guidelines development in gestational diabetes, perinatal nutrition, and physical activity and exercise in pregnancy.
ACKNOWLEDGEMENTS
We would like to acknowledge and thank all the staff who participated in data collection and management.


