Abstract
INTRODUCTION
Temporomandibular joint disorders (TMJDs) are caused by several factors such as anatomical, neuromuscular and psychological alterations. A relationship has been established between TMJDs and postural alterations, a type of anatomical alteration. An anterior position of the head requires hyperactivity of the posterior neck region and shoulder muscles to prevent the head from falling forward. This compensatory muscular function may cause fatigue, discomfort and trigger point activation. To our knowledge, a method for assessing human postural attitude in more than one plane has not been reported. Thus, the aim of this study was to design a methodology to measure the external human postural attitude in frontal and sagittal planes, with proper validity and reliability analyses.
METHODS
The variable postures of 78 subjects (36 men, 42 women; age 18–24 years) were evaluated. The postural attitudes of the subjects were measured in the frontal and sagittal planes, using an acromiopelvimeter, grid panel and Fox plane.
RESULTS
The method we designed for measuring postural attitudes had adequate reliability and validity, both qualitatively and quantitatively, based on Cohen's Kappa coefficient (> 0.87) and Pearson's correlation coefficient (r = 0.824, > 80%).
CONCLUSION
This method exhibits adequate metrical properties and can therefore be used in further research on the association of human body posture with skeletal types and TMJDs.
INTRODUCTION
The posture of the human body has been extensively studied due to the impact generated when it is altered. Alterations in the posture of the human body are not necessarily due to deviations from normal structure or function, but may be due to the misuse of body capabilities. If these alterations become persistent, they can result in discomfort, pain and disability.
Postural attitude refers to the general posture of the joints in the body at any given time, whereas static postural alignment refers to the position of various joints and body segments. Postural alterations can affect various body systems, including the stomatognathic system. A close relationship between impaired posture and craniomandibular disorder has been described.(1,2) For example, an anterior position of the head requires hyperactivity of the posterior muscles of the neck and shoulders to prevent the head from falling forward, causing fatigue, discomfort and activation of trigger points.(1)
Temporomandibular joint disorders (TMJDs) are musculoskeletal disorders affecting the jaw joint and chewing muscles. Common symptoms are pain in the orofacial region, restricted jaw movement and sounds originating in the temporomandibular joint.(3,4) Influential factors in the aetiology of TMJDs are psychological,(5) neuromuscular(6) and anatomical.(7,8) Body posture has been described as a causal or risk factor that is often omitted.(9) TMJDs do not only relate to the position of the jaw and skull; other structures (e.g. cervical spine, suprahyoid and infrahyoid structures, shoulders and thoracolumbar spine) are also involved.(2,10-12) Several studies have described a higher prevalence of signs and symptoms of TMJDs in patients with impaired body postures, as compared to patients without impaired body postures.(13-15) TMJDs are very common and have been estimated to affect 20%–30% of the adult population, particularly those aged 20–40 years.(16)
Therapeutically, both TMJDs and cervical syndromes should receive comprehensive assessment and treatment.(17) Therefore, objective measurements of postural attitude are important. Current methods for measuring body posture have disadvantages in terms of the time of measurement, evaluator's influence on the evaluation and management, simplicity and cost of the devices used, and ability to obtain reliable results. Furthermore, these methods usually only study one plane of the patient, assuming that a line is the norm in most patients, and thus do not define a range of acceptance (i.e. normal range). Hence, these methods do not allow for the proper assessment of posture, with regard to the definition of postural attitude and static postural alignment.
Proper posture is the straight, vertical alignment of the body, from the top of the head, through the body, to the bottom of the feet. Static alignment is achieved when the body is in a position that achieves balance. In order to attain static alignment, the neck should be placed in the middle of the two sides of the body, medially aligned in relation to the frontal and sagittal (lateral) planes. It is important to be able to measure body posture using a reliable method, as it enables clinicians to establish alignment and relate it to TMJDs. Such knowledge can be used to determine the best type of physical therapy for patients with postural alterations, which is likely to include body postural adjustment.
Most studies have focused on the upper body segments(17) without evaluating the subject as a whole. A valid and adequately reliable measurement method for determining whole body posture in both the frontal and sagittal planes has yet to be reported. Thus, the purpose of the present study was to evaluate the validity and reliability of a methodology designed to clinically determine external human postural attitude in the frontal and sagittal planes, so that it may be used in future research on posture and TMJDs.
METHODS
A convenience sample of 78 subjects (36 men, 42 women; age 18–24 years), with variable postures was obtained. All of the subjects voluntarily agreed to participate in the study and signed an informed consent document. This study was approved by the Ethics Committee of Universidad de La Frontera, Chile. All measurements and data collection were performed at the Anatomy Department of Basic Sciences, Faculty of Medicine, Universidad de la Frontera, Chile.
The following were used for the measurement of human body posture: (a) an acromiopelvimeter (AP), a system that measures the slopes from the shoulders to the height of the acromioclavicular joint and the pelvis in a horizontal base (Figs.
Fig. 1
Photographs show the (a) acromioclavicular joint, (b & c) pelvis and (d) knee joint attachment points of the plates of the acromiopelvimeter.
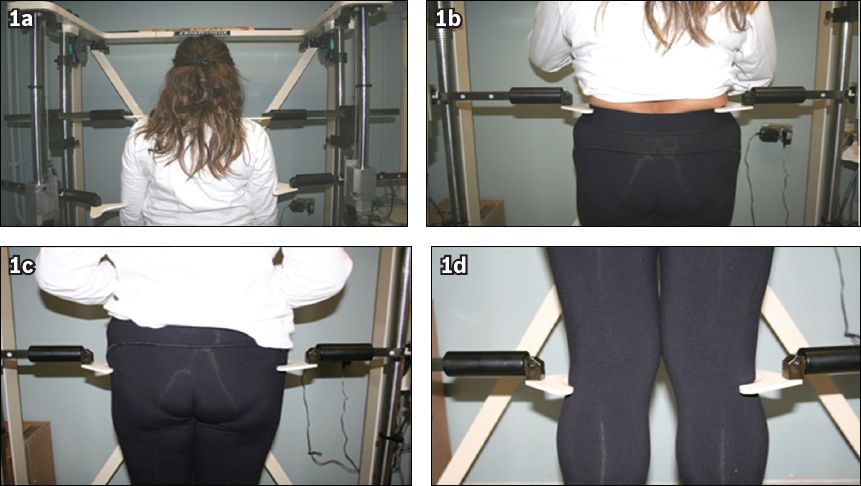
Fig. 2
Diagrams show (a) the acromioclavicular joint and pelvis attachment points of the plates of the acromiopelvimeter, and the measuring points of posture using the panel grid in the (b) frontal and (c) sagittal planes.
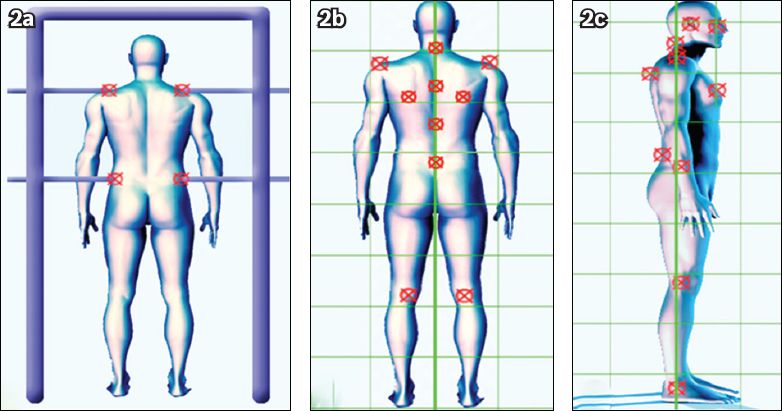
Postural attitude was measured in both the frontal and sagittal planes. In the frontal plane, the acromial and pelvic alignment was evaluated using the AP from a posterior view. The subjects were placed upright on a rigid platform, their feet 10–15 cm apart, heels in contact with a line marked on the platform and arms to their sides. To measure the pelvis and acromial height, the posterior iliac crest and acromioclavicular joint were palpated. The two plates were positioned and fixed at the level of the posterior iliac crest and acromioclavicular joint, and the difference between the fixed plates was measured.
Frontal deviations along the spine (cervical, thoracic and lumbar), alignment of the shoulders, shoulder grading and levelling of the popliteal line were measured from a posterior view, using the GP. The subjects stood with their feet 8 cm apart, with divergent points of 10°, their eyes fixed on the horizon and arms at their sides. The following structures were marked: vertebral spinous processes; acromioclavicular joint; spine of the scapula; and popliteal lines. The points were transferred to the GP and the deviations measured using a digital calliper.
In the sagittal plane, the anteroposterior position of the head, spinal curvatures (cervical, thoracic and lumbar), shoulder position, pelvis and knee joints were evaluated from a right-side view, using the GP. The GP was calibrated and the lateral plane was determined. For measurements performed in the frontal plane, the subject's position was maintained, but with the external lateral malleolus tangential to the true vertical. Points marked for measurement were the midpoint of the knee joint, anterior superior iliac spine, concave point of the lumbar curve, convex point of the thoracic curvature, upper point of the acromioclavicular joint, concave point of the cervical curvature, external acoustic meatus, most prominent point of the zygomatic bone and sternum. These points were transferred to the GP and the distances between them and the vertical were measured with the digital calliper, evaluated and compared to the zygomatic-sternal plane with the true vertical.
Finally, facial parallelism was evaluated from an anterior view using the FP. Measurements were taken with the subject standing comfortably and looking over the horizon. The subject was asked to sustain the FP against the jaw to project the occlusal plane. The bilateral pupil plane was projected through a ruler attached to the FP. By measuring a point in each plane perpendicular to the pupils, the plane parallels were compared.
Analysis of the reliability of the data was performed using Cohen's Kappa coefficient, which quantifies the degree of agreement between examiners, and adjusted for chance agreements. Interobserver analysis was performed between the measurements made by Assessors A and B, and the results were compared with the measurements made by Assessor C. Differences between 0–5 mm were tolerated. A Cohen's Kappa coefficient of 1 was deemed as perfect agreement, while values > 0.75 were deemed excellent and values ≥ 0.40 were considered acceptable.(18) The validity of the measurements was analysed using Pearson's correlation coefficient; values ≥ 80% were considered to have an acceptable degree of validity.
RESULTS
Based on Cohen's Kappa coefficient, most of the variables had excellent interobserver agreement (> 0.87); seven variables had perfect interobserver agreement (data not shown). The acromioclavicular joint variable evaluated in the sagittal plane using the GP yielded a Cohen's Kappa coefficient of 0.65 (i.e. good agreement). The slope of the acromion at the acromioclavicular joint yielded a Cohen's Kappa coefficient of 0.55 (i.e. moderate agreement). The following variables were classified as not applicable, as we were unable to obtain their Cohen's Kappa coefficient: acromioclavicular gap presence; shoulder slope presence; acoustic meatus; and thoracic curvature convex point.
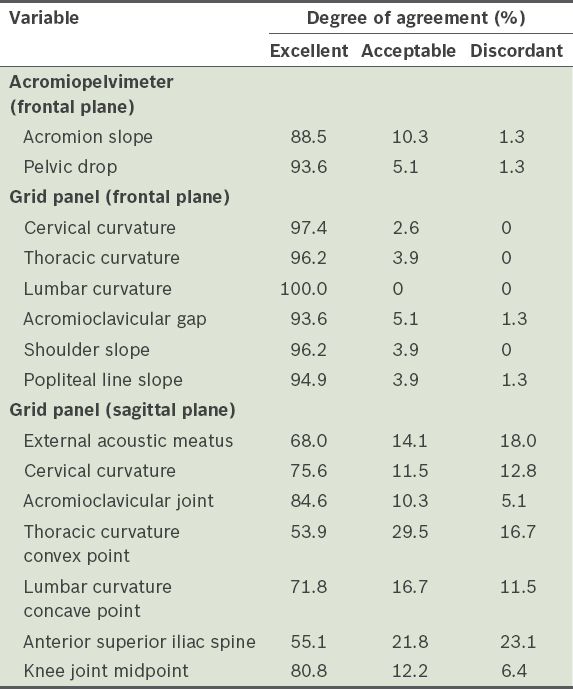
Assessment of the degree of concordance of the quantitative variables found excellent concordance (> 80%) in all variables measured in the frontal plane, using the AP and GP. In the sagittal plane, only the acromioclavicular joint total difference and knee midpoint total difference (84.6% and 80.8%, respectively) had excellent agreement. The degree of agreement varied from 53.9%–75.6% for the remaining variables (
Table I
Degree of agreement of the quantitative measurements of total difference.
Validity was determined by the sensitivity and specificity of the measurements made by Assessors A and B as compared to those made by Assessor C (
Table II
Validity of the qualitative measurements made by Assessors A and B, as compared to those made by Assessor C.
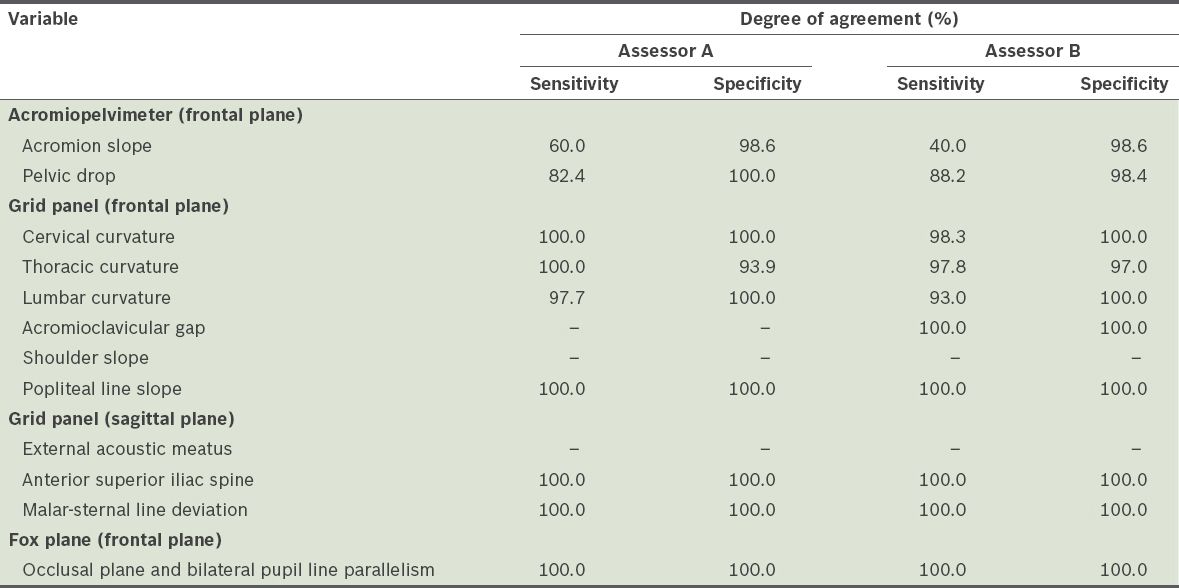
When the validity of the quantitative variables were examined, most of the variables had a Pearson's correlation coefficient > 0.824; there was a high correlation between the measurements made by Assessors A and B, and those by Assessor C. For Assessors A and B, the Pearson's correlation coefficient was 0.78 (i.e. high correlation) for the total difference in the slope of the acromion and 0.53 (i.e. moderate correlation) for the pelvic drop total difference.
DISCUSSION
In correct posture, the line of gravity passes through the axes of all joints of the vertically aligned body segments. It is important for the head, trunk, shoulders and pelvic girdle to be in mechanical and muscular balance. Statistical analysis performed on the methodology of the present study, which was designed to clinically determine the external human postural attitude in the frontal and sagittal planes, showed that it has adequate reliability and validity, unlike other methods in the literature; moreover, most of the other methods were not tested by validation statistics.(19) Thus, the methodology used in this study shows adequate metric properties.
The variables that were measured using an AP (i.e. acromion slope and pelvic drop) showed a high degree of specificity, in contrast to sensitivity, in the validity analysis. Thus, this tool can be used to determine the presence of disease. The other methods, using a GP or FP, had predominantly higher rates, reflecting their sensitivity in detecting the presence of pathology.
A previous study by Fuentes et al(13) showed that individuals who had an imbalance at the level of the shoulders had more tenderness in their temporal and masseter muscles, as compared to those with hip misalignment; similar results were reported by Zonnenberg et al.(12) Hansson et al(2) reported that an imbalance of the pelvis can cause TMJDs and Guo et al(16) established that the prevalence of TMJDs in the adult population is around 20%–30%, affecting adults aged 20–40 years.
A study by Nicolakis et al(10) examining the relationship between TMJDs and postural abnormalities reported a significant association between postural abnormalities and impaired muscle function in individuals with TMJDs, when compared with healthy subjects. These abnormalities included changes in the cervical region, dysfunction of the trunk in the frontal and sagittal planes (e.g. increased thoracic kyphosis and lumbar lordosis), protruding abdomen, and shoulder abduction. Farias et al(20) evaluated the posture of patients diagnosed with a TMJD and noted that most had their heads turned and/or sloped, and a high shoulder on the side of the temporomandibular joint (i.e. suffering a major disruption). In that study, the patients who reported pain on palpation of the sternocleidomastoid muscle presented with anterior head placement, corrected cervical and thoracic spine, and a lumbar region with increased physiologic lordosis. They also had hip anteversion, bilateral hyperextension with talar valgus knees and flat feet. Lippold et al(21) demonstrated a correlation between craniofacial parameters and the shape of the back profile, thoracic area, and lumbar and pelvic angles.
Saito et al(17) assessed the body posture of patients with TMJDs, and made measurements by marking bony landmarks with adhesive tape and taking digital photographs. Their study concluded that there was a close relationship between body posture and TMJDs, warranting the need for postural assessment as an essential component of the general management of such disorders. However, the authors of that study stated that the diagnostic methods used were a limitation of their study, as they resulted in the inclusion of false-positive disc displacement diagnoses. Furthermore, as it was a transverse study, subjects were only evaluated once; therefore, individual variation over time was not considered.(17)
The present study was not without limitations. Our sample size was small and it was difficult to monitor the patients continuously throughout the study period. Nonetheless, the present study contained adequate measurement properties for statistical analysis. The methodology presented in the present study can also supply much information on the various joints and body segments, as it consisted of evaluations of posture in the frontal (from a posterior and anterior view to assess facial parallelism) and sagittal planes, and lateral view. With the development of a valid and reliable methodology for measuring posture, investigations to establish the normal range of human posture in different populations, ethnic groups and skeletal types can be performed. The development of a valid and reliable methodology for measuring posture will also facilitate investigations into the relationship between posture and TMJDs, as well as other human postural disorders.


