Dear Sir,
Küttner's tumour, a chronic sclerosing disease of the salivary glands, is an immunoglobin G4 (IgG4)-related disease. We herein present a case of Küttner's tumour in which the patient developed an isolated buccal nerve palsy associated with parotid gland involvement (
Fig. 1
(a) Photograph shows loss of the patient's right nasolabial fold, right parotid swelling and bilateral upper eyelid fullness. Left parotid swelling is not shown. (b) Axial CT image with intravenous contrast shows diffuse enlargement of the involved glands with patchy enhancement.
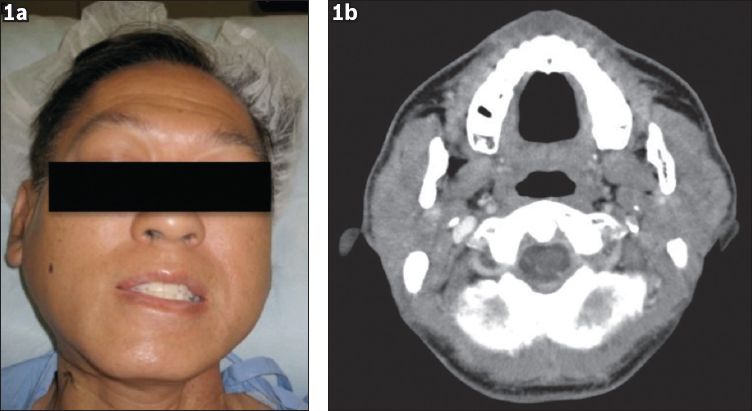
A 55-year-old Chinese man presented with a one-year history of painless left submandibular gland enlargement. The findings of fine needle aspiration, performed on two separate occasions, were consistent with those of a reactive lymph node. In view of the size of the mass, we proceeded with excision of the gland to rule out malignancy. Histology was consistent with Küttner's tumour. Almost a year after the first surgery, the patient presented with progressive swelling of his right submandibular, bilateral parotid and lacrimal glands. This was associated with a partial palsy of the buccal branch of his right facial nerve. Computed tomography showed diffuse enlargement of the involved glands with patchy enhancement (
Unfortunately, the patient's buccal nerve palsy did not resolve despite a course of oral prednisolone. In our literature review, there were reports on the involvement of the optic, trigeminal and spinal nerves, but none on facial nerve involvement.(1-4) In one study on IgG4-related neuropathy,(4) imaging of affected nerves typically showed masses along the course of the nerve. The histopathology of these lesions showed infiltrating lymphoplasmacytic cells with a high proportion of IgG4-related plasma cells. The lesions responded well to a course of systemic steroids.
In our patient, timely magnetic resonance imaging could not be performed to determine the presence of these perineural lesions; biopsy was also not performed due to potential associated morbidity. Contrary to previous findings in the literature,(4) our patient did not respond to a course of systemic steroids. In our opinion, the lack of response may suggest an alternate pathophysiology for nerve dysfunction in our patient. It is possible that the palsy may be secondary to compression of the nerve from an increase in pressure in the parotid fascial space brought on by inflammation. We hope that this report contributes to the rapidly evolving literature regarding this relatively young disease entity and may be the nidus for further research.


