Abstract
INTRODUCTION
Oncoplastic breast-conserving surgery (OBCS) can cause breast asymmetry. Although contralateral breast surgery to achieve symmetry was offered to these patients, the uptake of symmetrisation was variable. We aimed to determine the factors that deter patients with breast cancer undergoing OBCS from opting for symmetrisation.
METHODS
All patients with breast cancer who underwent OBCS of displacement type with no symmetrisation were prospectively surveyed to explore the social, economic, psychological and physical reasons against symmetrisation.
RESULTS
A total of 28 patients participated in a survey administered at a mean 21.6 (range 2–47) months after OBCS. A combination of factors, such as worry and desire to treat breast cancer first (67.9%), not being overly concerned about breast cosmesis (57.1%) and fear of pain from additional operation (28.6%), deterred patients from immediate symmetrisation. Worry and desire to treat breast cancer first was the most important single factor for 50% of the patients. Reasons for no delayed symmetrisation included not being overly concerned about breast cosmesis (70.4%), fear of breast cancer recurrence (48.1%) and being happy with current breast cosmesis (33.3%), with the former two reasons equally cited as the single most important deterrent by 30% of patients each.
CONCLUSION
A combination of factors may deter patients from symmetrisation. The most significant factors deterring OBCS among patients were worry and desire to treat breast cancer first for immediate symmetrisation, and not being overly concerned about breast cosmesis and fear of breast cancer recurrence for delayed symmetrisation. Reassuring these patients may increase their uptake of symmetrisation, thereby improving patient cosmesis and satisfaction.
INTRODUCTION
Oncoplastic breast-conserving surgery (OBCS) allows resection of larger tumours with a lower re-excision rate than that of standard lumpectomy, thereby averting a potential mastectomy. However, as asymmetry of the breasts is likely to occur subsequent to OBCS, contralateral breast symmetrisation has been offered to patients undergoing OBCS as an integral part of the procedure. However, the uptake of contralateral symmetrisation is not well reported in the literature and ranges from 0% to 100%.(1,2)
To our knowledge, the reasons for not opting for contralateral symmetrisation among patients undergoing OBCS are not well studied. We aimed to determine the various factors that may influence decisions made by patients with breast cancer regarding undergoing contralateral symmetrisation along with or subsequent to the OBCS procedure.
METHODS
All patients with breast cancer who underwent OBCS at our tertiary healthcare institution from 1 May 2014 to 28 February 2018 were recruited for the study. The study was approved by the SingHealth institutional review board.
These patients were offered the option of breast conservation or mastectomy, with or without reconstruction. They had opted for OBCS, as they were keen on breast conservation but had a large tumour-to-breast-size ratio or multifocal/multicentric tumours. Patients with asymmetric breasts and cancer on the larger breast were also offered OBCS. The type of OBCS performed depended on the patient’s breast size, degree of ptosis, and the size and location of the tumour.
All patients were offered concurrent contralateral breast symmetrisation. Patients who had undergone symmetrisation, lumpectomy with partial breast reconstruction and those with cancer on a larger asymmetric breast were excluded. Patients with breast cancer with contralateral breast cancer/lesion requiring surgery were also excluded. All patients received adjuvant treatment, as recommended by a multidisciplinary team.
Patients who met the inclusion criteria were prospectively invited to participate in a survey using a self-administered questionnaire that consisted of ten multiple-choice questions on social, economic, psychological and physical factors that may have influenced their decision-making. The questionnaire was administered during routine outpatient follow-up visits. If there were any problems with survey interpretation, a breast care nurse was available for assistance. Patients rated breast asymmetry as ‘very’, ‘slight’ or ‘no’. ‘Very’ was defined as marked asymmetry, ‘slight’ as noticeable but not marked asymmetry and ‘no’ as no asymmetry.
RESULTS
A total of 55 patients underwent OBCS during the study period. Of these, 27 (49.1%) patients were excluded, as two patients were lost to follow-up, two patients underwent completion mastectomy, one patient underwent symmetrisation, six patients underwent bilateral breast surgeries, 13 patients underwent lumpectomy with partial breast reconstruction using local chest wall flap reconstruction, and three patients had asymmetrical breasts and cancer on the larger breast. While one patient had immediate symmetrisation, 28 (50.9%) patients did not, resulting in an immediate symmetrisation rate of 3.4%. These 28 patients were prospectively enrolled, and the survey participation rate was 100.0%. The survey was administered at a mean of 21.6 (range 2–47) months after the OBCS procedure.
The median and mean patient age were 53.0 years and 54.0 (range 36–74) years, respectively. Various OBCS techniques were used, namely round block mammoplasty (n = 18), wise pattern mammoplasty (n = 7), vertical mammoplasty (n = 2) and batwing mammoplasty (n = 1) (
Table I
Demographics and cosmetic outcomes of patients who underwent OBCS without contralateral symmetrisation (n = 28).
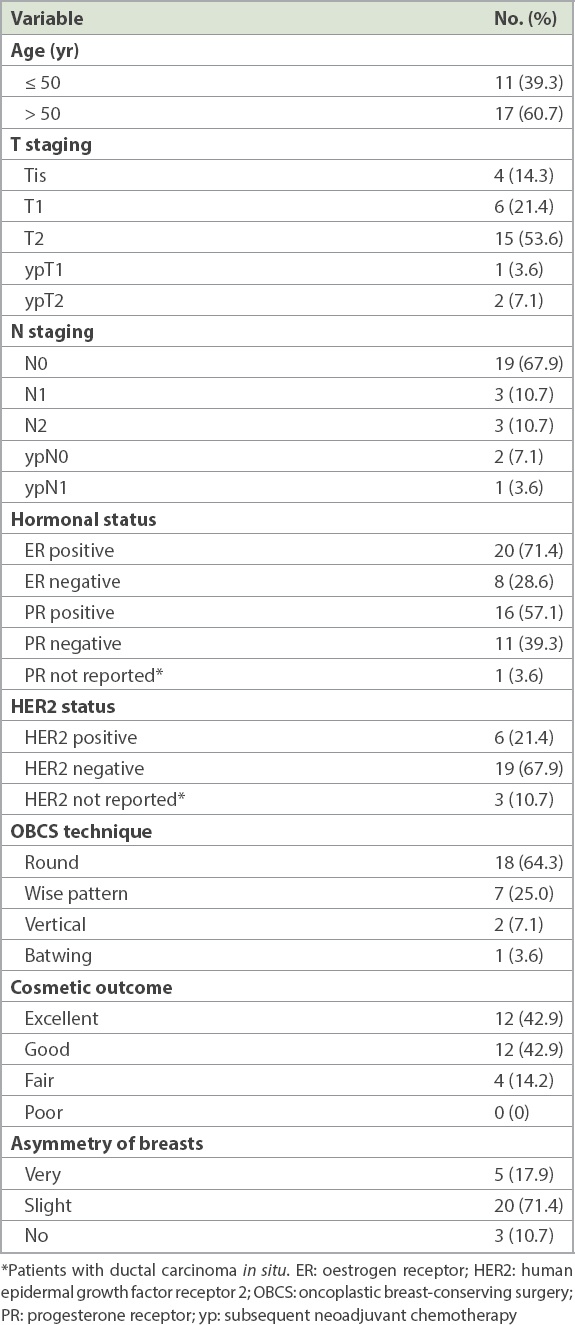
Three patients received neoadjuvant chemotherapy and all except one patient underwent adjuvant radiotherapy. No locoregional recurrence was reported. 85.8% of patients rated their postoperative breast cosmetic appearance as excellent or good. Of the remaining four patients who rated their breast cosmetic appearance as fair, one patient required repeated re-excisions to obtain clear margins.
89.3% of patients reported asymmetry of their breasts, with 5 (17.9%) patients and 20 (71.4%) patients reporting great and slight asymmetry, respectively (
Fig. 1
Photographs show patient with (a) great asymmetry in the breasts one year after right-wise pattern mammoplasty without contralateral symmetrisation and (b) slight asymmetry nine months after right round block mammoplasty without contralateral symmetrisation.

23 (82.1%) patients did not consider undergoing surgery on the normal breast at the time of OBCS to achieve symmetry of both breasts. 5 (17.9%) patients considered immediate symmetrisation but did not proceed with it. In these 28 patients, a combination of factors was the reason for deferring symmetrisation at the time of OBCS, such as worry and desire to treat breast cancer first (67.9%), not being overly concerned about the cosmetic appearance of their breasts (57.1%) and fear of pain from additional operation (28.6%) (
Fig. 2
Chart shows perceived factors deterring patients undergoing oncoplastic breast-conserving surgery from opting for immediate symmetrisation.
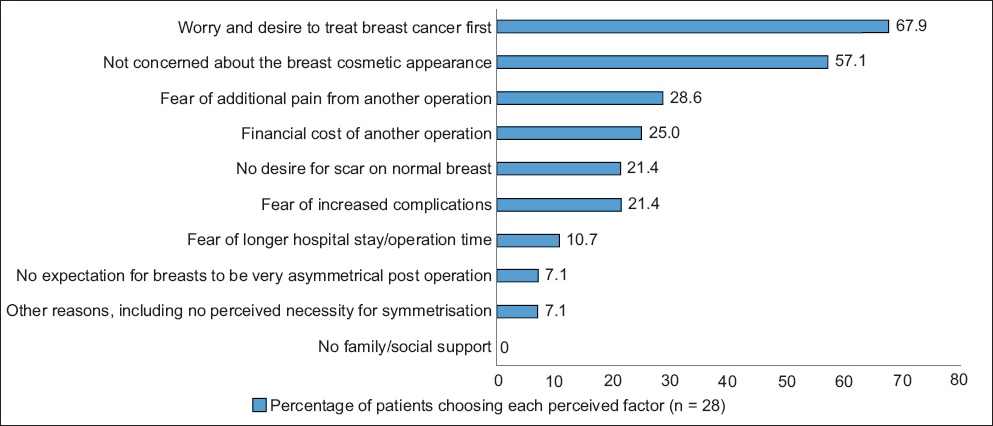
Among the various reasons for not considering immediate symmetrisation, worry and desire to treat breast cancer first was cited as the single-most important contributing factor by 50% of the patients.
With regard to delayed symmetrisation of the normal breast to achieve symmetrical breast appearance, 25 (89.3%) patients indicated that they would not consider undergoing the procedure. While 3 (10.7%) patients considered delayed symmetrisation, only one patient actually underwent delayed symmetrisation, resulting in a delayed symmetrisation rate of 3.6%. The most commonly cited reasons for not opting for delayed symmetrisation in these 27 patients were: not being overly concerned about the cosmetic appearance of breasts (70.4%), fear of breast cancer recurrence and thus not giving much thought to symmetrisation (48.1%), and being happy with their current breast cosmetic appearance (33.3%) (
Fig. 3
Chart shows perceived factors deterring patients undergoing oncoplastic breast-conserving surgery from opting for delayed symmetrisation.
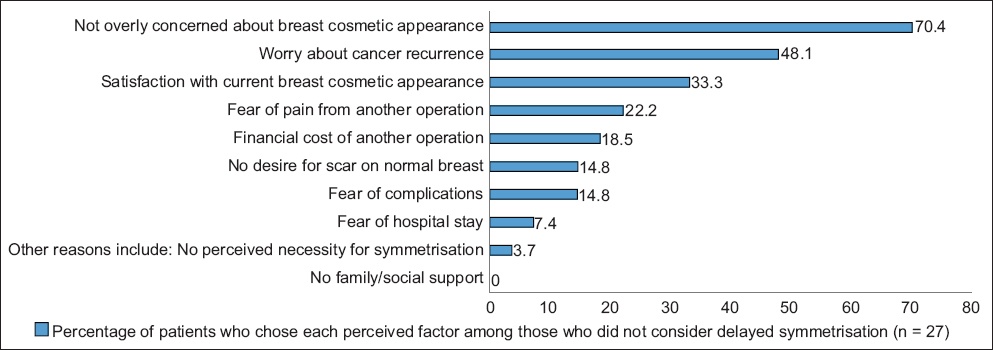
Subsequent to OBCS, although 23 (82.1%) patients reported slight or no asymmetry of breasts, only 3 (13.0%) of these patients cited satisfaction with current breast cosmetic appearance as the major factor deterring them from pursuing delayed contralateral symmetrisation.
Among all the reasons for patients not opting for delayed symmetrisation, the most important contributing factors were not being overly concerned about the cosmetic appearance of their breasts (30.0%) and fear of breast cancer recurrence (30.0%). The subgroup of patients who cited the reason of not being overly concerned about the cosmetic appearance of their breasts was older than the overall cohort, with a mean age of 60 (range 41–74) years.
DISCUSSION
We found that in our cohort of patients undergoing OBCS without contralateral symmetrisation, only 17.9% of patients initially considered immediate symmetrisation. Worry over breast cancer was the single most important deterring factor for immediate symmetrisation. Following OBCS, although 89.3% of patients reported asymmetry of breasts, only 10.7% considered delayed symmetrisation. Not being overly concerned about breast cosmesis and fear of breast cancer recurrence were cited as the top reasons for not opting for delayed symmetrisation. To our knowledge, this is the first known study to explore the reasons for not opting for symmetrisation among patients undergoing OBCS.
Symmetrisation subsequent to OBCS can undoubtedly provide better brassiere fitting and improved cosmetic outcome, which have been correlated with enhanced psychosocial functioning.(3,4) Symmetrisation procedures have also been known to pick up occult cancer, although its incidence is rare at 0.94%–5.33%.(5,6) Despite symmetrisation procedures greatly improving patient satisfaction,(7) it was found that the asymmetry of breasts was not the most crucial factor influencing patients’ overall satisfaction.(8) This earlier study was, however, conducted on patients who had undergone mastectomy with reconstruction.
Symmetrisation can be undertaken in an immediate or delayed setting.(9) The advantage of immediate symmetrisation is that both breast surgeries can be performed simultaneously. Delayed symmetrisation, on the other hand, is usually performed after the patient has completed adjuvant treatment, allowing for the effects of radiotherapy on the operated cancerous breast to stabilise before symmetrisation is attempted. This approach is also advantageous, as it could allow for reoperation or completion mastectomy that may subsequently become necessary, which could alter the final breast appearance. It also avoids the potential risk of double surgical complications that could occur during concurrent symmetrisation, such that adjuvant treatment following OBCS may need to be delayed. Finally, it avoids the need for prolonged anaesthesia and associated risks, and enables a patient with limited financial resources to focus initially on tumour management and save up for aesthetic symmetrisation at a later date.
To our knowledge, the rate of uptake of symmetrisation is not well documented in the literature. The reported rates of immediate symmetrisation vary from 0%(1) to 100%.(2) Fewer studies regarding delayed symmetrisation exist. Among patients who did not undergo immediate symmetrisation, the reported incidence of delayed symmetrisation ranged from 9.2% to 10.0%.(10,11) The incidence of immediate and delayed symmetrisation in our study was 3.4% and 3.6%, respectively.
Worry and desire to treat breast cancer first was cited as the most important factor deterring patients from undergoing concurrent symmetrisation. Prioritising treatment of cancer over cosmetic concerns was also a common reason quoted for not undergoing reconstruction following mastectomy.(12) This concern could be addressed by providing reassurance and improved patient education to increase the uptake rate of immediate symmetrisation.
Meanwhile, fear of breast cancer recurrence and not being overly concerned about the cosmetic appearance of breasts were the two most cited reasons for not undergoing delayed symmetrisation. Fear of breast cancer recurrence is a common problem among cancer survivors. While some amount of fear of breast cancer recurrence is understandable and can be adaptive, fear in excess can be pathological, especially if it affects patients’ psychosocial functioning. Fear of breast cancer recurrence could give rise to hypervigilant symptom checking, with inappropriate attribution of symptoms to cancer recurrence instead of other ailments, anxiety over subsequent medical follow-ups and inappropriate excessive worry about physical health, with psychosocial consequences. Fear of breast cancer recurrence could also cause behavioural changes, where the patient engages in limited future planning,(13) which could explain why patients in our cohort had not given much thought to delayed symmetrisation. Our hypothesis is that the key apprehension in this subgroup of patients is that, should cancer recur on the ipsilateral breast so that a second surgery became necessary in the future, any symmetrisation performed would become redundant, as the shape, size and volume of the cancerous breast would vary again. It is likely that patients with breast cancer may reconsider delayed symmetrisation at a later date, as some studies have suggested that fear of breast cancer recurrence may decrease with time after diagnosis.(14)
Not being overly concerned about the cosmetic appearance of the breast was also a common reason cited for not opting for delayed reconstruction following mastectomy.(15) This could be attributed to patients accepting their bodily changes over time. These patients tended to be older, with a mean age of 60 years, which was consistent with our findings.
The present study had good strength, including a very high participant response rate for completed surveys. The survey was administered at a mean 21.6 months after OBCS to allow for stability of cosmetic outcome following treatment and to more accurately assess the reasons for not undergoing delayed symmetrisation. The questionnaire explored a comprehensive range of reasons, such as physical, emotional, social and psychological aspects, with only ten questions in the survey, so that the survey could be completed quickly and participant fatigue could be avoided.
However, our study has some limitations. This was a relatively small series from a single tertiary healthcare centre. Our oncoplastic workload was around 17 OBCS a year, which was comparable to the reported oncoplastic volumes of 19.3 OBCS a year at some high-volume centres in Scotland.(16) Most OBCS in our series involved the round block technique, which is the more commonly employed oncoplastic technique for the smaller breast size in Asian women.(17) Hence, breast asymmetry in these patients was unlikely to be as marked as in patients undergoing vertical/wise pattern mammoplasty. Nevertheless, other studies(18) using round block technique have found that up to 82% of patients underwent immediate contralateral symmetrisation. An assessment of the psychological effects of breast asymmetry, with particular attention to depression, body image, sexuality and self-esteem, was also not undertaken as part of this study, as our primary aim was to determine the reasons for not undergoing symmetrisation among patients undergoing OBCS.
In conclusion, worry and the desire to treat breast cancer first were cited as the most common important contributing factors deterring patients undergoing OBCS from considering immediate symmetrisation. Among the reasons for not opting for delayed symmetrisation, not being overly concerned about the cosmetic appearance of breasts and fear about breast cancer recurrence were the top cited factors. Given these findings, improved management of patients’ worry and fear about breast cancer recurrence may be implemented to increase the rates of symmetrisation uptake, which, in turn, would help improve cosmetic outcome and patient satisfaction.
About the First Author

Dr Lim Geok Hoon is the Head and Senior Consultant of the Breast Department, KK Women’s and Children’s Hospital, and a Clinical Associate Professor at Duke-NUS Medical School, Singapore. She is an oncoplastic breast surgeon who has several publications focusing on the surgical techniques that are most applicable to Asian women. She also has a special interest in genetic breast cancer. Dr Lim founded the Singapore Breast Oncoplastic Surgery Symposium in 2015 to increase regional awareness of oncoplastic surgery. She pioneered the minimal scar mastectomy technique and is the inventor of the world’s first virtual breast oncoplastic surgery simulator (VBOSS) used for oncoplastic surgery training.


