Abstract
Failure to thrive in a child is defined as ‘lack of expected normal physical growth’ or ‘failure to gain weight’. Diagnosis requires repeated growth measurements over time using local, age-appropriate growth centile charts. Premature babies with appropriate growth velocity and children with ‘catch-down’ growth, constitutional growth delay or familial short stature show normal growth variants, and usually do not require further evaluation. In Singapore, the most common cause of failure to thrive in children is malnutrition secondary to psychosocial and caregiver factors. ‘Picky eating’ is common in the local setting and best managed with an authoritative feeding style from caregivers. Other causes are malabsorption and existing congenital or chronic medical conditions. Child neglect or abuse should always be ruled out. Iron deficiency is the most common complication. The family doctor plays a pivotal role in early detection, timely treatment, appropriate referrals and close monitoring of ‘catch-up’ growth in these children.
Mrs Thomas, a homemaker, took her only child, 18-month-old Marcy, to the family clinic for fever and running nose. You diagnosed the common flu and was about to prescribe paracetamol when Mrs Thomas mentioned her concern that Marcy was not gaining weight and looked skinny compared to other children in the neighbourhood. She asked you if there was anything seriously wrong with Marcy and requested vitamin supplements to boost her appetite.
WHAT IS FAILURE TO THRIVE?
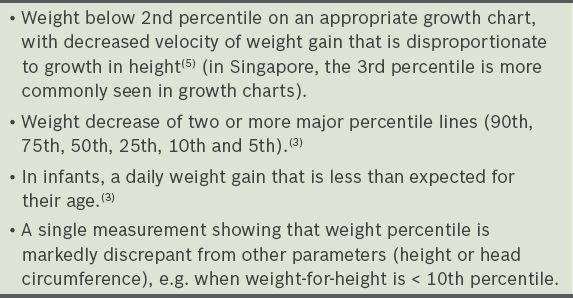
Failure to thrive (FTT) in a child is defined as ‘lack of expected normal physical growth’, ‘failure to gain weight’ or ‘lack of growth’.(1) There is no objective consensus on the definition of FTT, as no single measurement on its own appears adequate to identify nutritional growth delay.(2) Weight-for-age is the simplest parameter to assess for FTT. Other parameters that may assist in FTT diagnosis include weight-for-height and height-for-age. Diagnosis often requires repeated growth measurements over a period of time, although a single measurement of growth parameters may be sufficient in some situations (
Table I
Definitions of failure to thrive.
Normal growth variants in children
Not all children with low weights have FTT.(3) Some who fail to meet normal growth parameters may demonstrate a normal growth variant, including:
Children growing along a percentile curve, even if weight is < 2nd percentile (3rd percentile line is more common locally).
Premature babies or babies with intrauterine growth restriction who have appropriate weight-for-height and growth velocity.
‘Catch-down’ growth (decrease of ≤ 2 major percentiles)(4) – in ‘catch-down’ growth, the growth of normal children between six and 18 months of age decreases to lower growth percentile curves that match their genetic programming, then begins to follow new, lower percentile curves. These children should have normal developmental, behavioural and physical examinations. While they should be closely followed, no further evaluation is needed.
Constitutional growth delay – the hallmark of this condition is delayed bone age (below chronological age). Bone age is obtained by assessing the appearance and shape of the bones on a radiograph of the left hand and wrist. These children may have more severe and prolonged ‘catch-down’ growth; they may grow along a low growth percentile curve, with a low preadolescent growth rate and delayed pubertal development. However, ‘catch-up’ growth occurs when they enter puberty. Growth continues longer than that of other children and results in normal adult stature. There may be a family history of such delayed growth in the parent(s). Children with constitutional growth delay should be monitored closely and no further evaluation is needed.
Familial short stature – these children have a projected adult height that is within their anticipated adult height, based on mid-parental height.(6) Mid-parental height is calculated in the following ways: (a) for girls, subtract 13 cm from the father’s height and find the average with the mother’s height; (b) for boys, add 13 cm to the mother’s height and find the average with the father’s height; and (c) for both genders, 8.5 cm on either side of this calculated value represents the 3rd–97th percentiles for anticipated adult height. Projected adult height is obtained by extrapolating along the current height percentile curve for up to 18–20 years of age. For children with constitutional growth delay or accelerated growth, it is more accurate to use bone age, rather than chronological age, to determine projected height. Children with familial short stature, unlike those with constitutional growth delay, have a bone age that is consistent with their chronological age. No further evaluation is needed for these children.
HOW COMMON IS THIS IN MY PRACTICE?
In a local 2012 survey, about 50% of parents or guardians reported ‘picky eating all the time’ in their children who were aged 1–10 years.(7) The prevalence of ‘feeding difficulties’ (food refusal and selective eating) was about 15%. FTT is seen in 5%–10% of children in primary care settings and in 3%–5% of children in hospital settings in the United States.(8,9)
CAUSES, COMPLICATIONS AND RED FLAGS
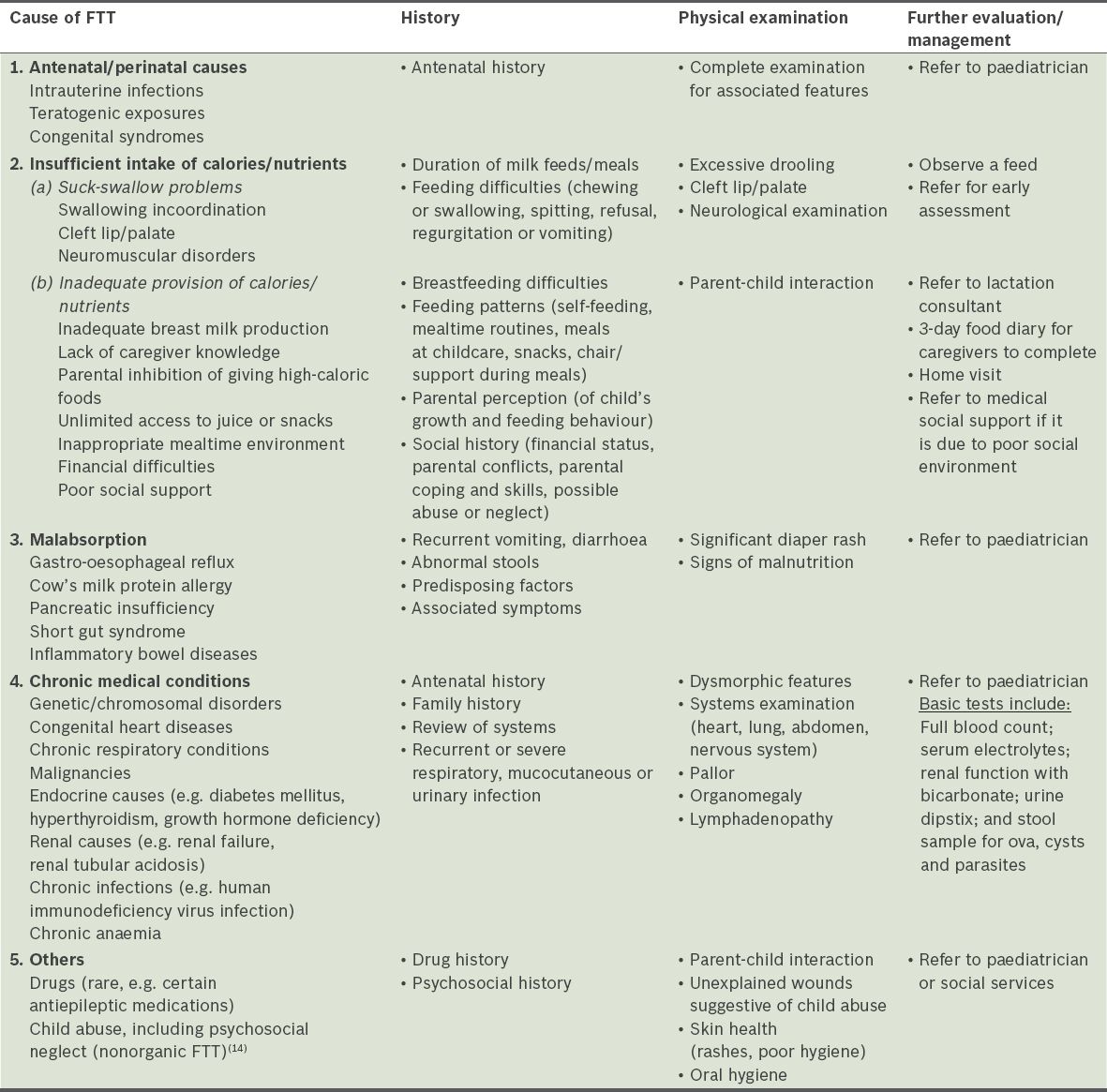
After FTT is diagnosed, the patient’s history is taken, and physical examination and further evaluation are performed to determine the causes and complications (Tables
Table III
Assessing for complications of failure to thrive (FTT).
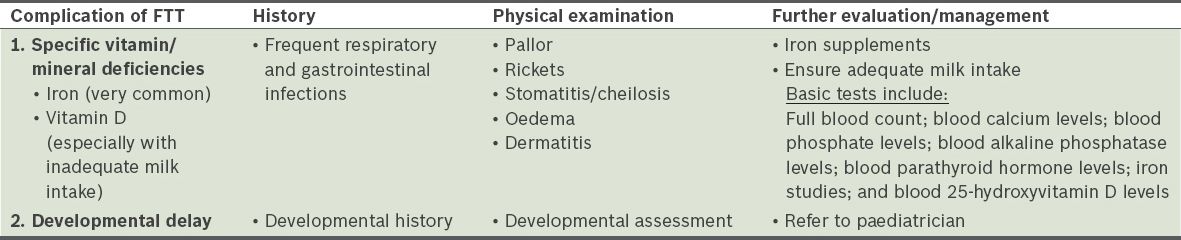
The presence of any red flags should alert the family doctor to initiate a referral to a paediatrician: (a) the child’s weight is three Z scores below the 50th percentile(11) (for a specific age, take the absolute weight difference between the 50th and 95th percentiles and divide by two to obtain the weight difference for one Z score); (b) signs of child abuse, including psychological neglect;(14) (c) clinical features of a medical cause for FTT; and (d) complications of FTT, e.g. developmental delay.
TAKING MEASUREMENTS
When taking measurements for a child with FTT, use appropriate growth charts from Singapore(15) or the World Health Organization.(16) Specific growth charts should be used for ex-premature infants and those with dysmorphology syndromes (i.e. Turner syndrome, Down syndrome and achondroplasia). Ensure that the equipment, such as the stadiometer, has appropriate accuracy and that measurement techniques are correct (e.g. child stands straight with back and heels against the stadiometer). Take the average of two height measurements. Neonates and young infants should be weighed while naked (without nappies and clothes) and consistently, before or after feeding.
WHY IS IT IMPORTANT TO MY PRACTICE?
The family doctor working in the community is best placed to detect FTT in children when they present for illnesses or health monitoring by enquiring further in cases where FTT is suspected. Through evaluation as well as timely management of FTT and any underlying psychosocial issues in the family, the outcomes for these children can be improved.
Management of FTT(13)
Medical conditions causing FTT should be treated or referred to a paediatrician for further investigations and management, while urgent psychosocial issues require counselling and referral to social services. Physicians should give age-appropriate nutritional counselling to parents or guardians, including advice on food preparation and feeding techniques.(10) The mealtimes of children with FTT should be limited to no more than 30 minutes; authoritative feeding styles are most effective.(17) Children should be monitored for ‘catch-up’ growth. If there is a limited variety of food and the child is not taking a nutritionally complete milk formula, consider checking for iron deficiency and prescribing a multivitamin supplement that contains iron. Adequate complementary foods should be introduced at the appropriate time.
Mrs Thomas revealed that Marcy, a premature baby at 35 weeks, has always been small but healthy. Marcy is a fussy eater, eating only rice, chicken and spinach. Mrs Thomas and her husband are of average height with no family history of serious medical conditions and no financial difficulties. A careful examination showed Marcy to be an alert and cheerful child who looked thin but did not have ill health, neglect, developmental delay or nutritional deficiencies. Her weight is at the 10th percentile and has not crossed any growth centile. Her head circumference and height, which are at the 25th percentile, are constant. You reassured Mrs Thomas that Marcy, though thin, is healthy and developing normally. You advised her to introduce different foods slowly and discretely, then arranged for a follow-up visit in a month’s time to monitor Marcy’s growth.
TAKE HOME MESSAGES
-
Use local and age-appropriate growth centile charts to determine if the child has FTT, being aware of normal growth variants.
-
Take a careful and thorough medical, dietary and psychosocial history to determine any underlying causes for FTT and any associated complications.
-
The most common cause of FTT worldwide is malnutrition or insufficient caloric intake due to poverty or caregiver ignorance.
-
Management of a child with FTT often requires collaboration of care between the family doctor and other healthcare colleagues such as the paediatrician, dietitian and nurse counsellor.
-
Children with FTT should be treated promptly and followed up closely for catch-up growth.
SMJ-57-291.pdf