Abstract
INTRODUCTION
In line with the effort to evaluate feasible surgical options for vasectomy reversal and to increase patients’ willingness to undergo the procedure, this study reported on a technique for ambulatory mini-incision microsurgical vasovasostomy using a double-ringed clamp (i.e. Moon’s clamp). This technique does not require the use of dilators, approximators and other accessory devices.
METHODS
Ambulatory mini-incision microsurgical vasovasostomy was conducted on 263 patients who satisfied the surgical eligibility requirements for vasovasostomy and the safety criteria for local anaesthesia. The operation time, details on postoperative recovery and results of the postoperative semen analysis were recorded and retrospectively analysed.
RESULTS
The mean time used to isolate the bilateral vas deferens was 25.5 minutes. All patients were discharged on the day of surgery and all patients returned to their normal activities within 24–48 hours after surgery. No haematoma or infection occurred except in one patient. Postoperative semen analysis showed that the surgery was successful in 182 (96.8%) of the 188 patients who complied with the postoperative patient instructions.
CONCLUSION
Ambulatory mini-incision microsurgical vasectomy reversal using Moon’s clamp and under local anaesthesia is a surgically feasible option that offers the advantages of a low-risk operation. It also achieves successful vasovasostomy without other accessory devices and allows patients to return to their daily activities quickly with minimal complications.
INTRODUCTION
Successful vasectomy reversal involves surgery performed by a skilled expert, using a high-level microsurgical technique for various conditions of the scrotum and vas deferens. The procedure is associated with high surgical success rates and few complications (due to surgery or anaesthesia), with patients returning to their daily activities within a short duration of time. Different surgical and anaesthetic methods result in variations in postoperative stability and recovery time, which are related to the cessation of the patient’s social activities and the economic burden of missed employment. In an effort to increase patients’ willingness to seek vasectomy reversal, this study evaluated a surgical technique of ambulatory mini-incision microsurgical vasovasostomy performed under local anaesthesia, which involves the use of a double-ringed Moon’s clamp.(1) Dilators, approximators and other accessory devices are not required in this technique.
METHODS
Ambulatory mini-incision microsurgical vasovasostomy was conducted on 263 patients at the CR Microsurgery Center, Korea, between October 2006 and June 2011. The mean time after vasectomy (obstructive interval) was 7.05 (range 0.25–24.0) years and the mean age of the patients was 38.88 (range 26–57) years. All 263 patients satisfied the eligibility requirements for vasovasostomy, in terms of both age and obstructive interval. They also fulfilled the safety criteria for the administration of local anaesthesia within an outpatient clinical setting. Patients with the following conditions were excluded: (a) adherence of the previous vasectomy site to the testicular capsule, resulting in a high probability that vasoepididymostomy would be required; and (b) the high level at which the previous vasectomy was performed, resulting in a high possibility for the need to expand the surgical area.
Before surgery, local anaesthesia using approximately 10–15 mL of a single dose of 1% lidocaine without epinephrine was administered to both sides of the scrotal skin and spermatic cord.(2-4) For vas deferens anastomosis, three-layer anastomosis using the microdot technique with 10-0 and 9-0 nylon sutures was performed on all patients under a surgical microscope with 10–15 times magnification.(5,6) Vasovasostomy was performed on all patients, regardless of whether there was fluid leakage from the testicular vas during vas transaction, and regardless of the fluid quality.(7) The patients’ medical records were reviewed for information on the patients’ recovery after operation, and the results of the postoperative semen analysis were analysed to evaluate the surgical success rate (i.e. the patency of the vas deferens).
In the present study, mini-incision vasectomy reversal was simplified with the use of a double-ringed Moon’s clamp, a previously described tool that was used for a convenient, real no-scalpel vasectomy.(1) Moon’s clamp is particularly appropriate for minimally invasive vas surgery. Patients were instructed to lie in the supine position in the operating room, which was at room temperature. Aseptic preoperative preparations, including shaving, disinfecting and draping of the scrotal area, were performed in a manner similar to that for other scrotal surgeries. Before the administration of local anaesthesia, the presence and location of the previous vas deferens surgical area were confirmed by the surgeon via tactile examination. After a local anaesthetic agent was injected into the skin area corresponding to the level of the previous surgical area and into the nearby vas deferens of the spermatic cord, close to the external inguinal ring, an approximately 8-mm long and 10–15-mm deep incision was made using the sharp end of a narrow-width surgeon’s knife.
A small, straight haemostat was pushed into the incision in a vertical position, approximately 2 cm deep, and then pulled out. The exit site of the haemostat was used as the main pathway, which was the nearest possible communicating passage from the scrotal skin to the vas deferens and nearby tissues. A Moon’s clamp was placed downwards into this communicating passage. The end of the clamp was then guided to the abdominal side of the previous vasectomy area of the vas deferens. The vas deferens, with minimal amount of adjacent tissue, was pushed into the opened major distal ring of the Moon’s clamp, which was subsequently closed.
After the Moon’s clamp was taken out of the scrotal skin, the vas deferens and the small perivasal tissues attached to the vas deferens inside the ring were examined. Next, the Moon’s clamp was positioned horizontally, and the small perivasal tissues, which were attached to the vas deferens were transferred from the distal ring to the proximal ring using a small curved haemostat, through the gap between the two rings in a layer-by-layer manner. During this process, the vas deferens of an appropriate length and the adjacent tissues were dissected, separated and left in the major distal ring. The space secured from the separation was marked with a tape or a tower clamp for subsequent procedures.
Using the same method described in the previous paragraph, the lower vas deferens at the testicular side was dissected and separated from the nearby tissues. Subsequently, all the surrounding cord structures and tissues attached to the previous vasectomy area of the vas deferens were freed to prepare the area for microsurgical anastomosis (Figs.
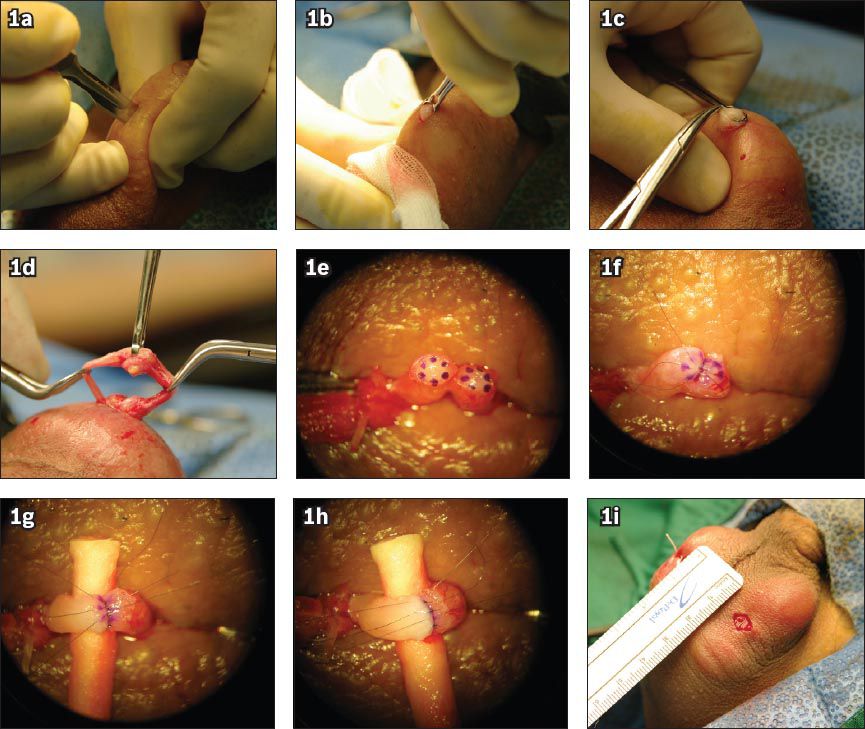
Fig. 1
(a)–(i) Photographs show minimally invasive vas isolation for vasovasostomy using a double-ringed Moon’s clamp and microsurgical vasovasostomy via three-layer anastomosis using the microdot technique. (a) A surgical window is created with the narrow width of a small surgical blade. (b) The vas deferens and nearby tissues are pulled out using the Moon’s clamp via the surgical window. (c) The Moon’s clamp is positioned horizontally, and the small perivasal tissues attached to the vas deferens are transferred from the major distal ring to the proximal ring using a small curved haemostat. (d) The vas deferens after dissection and separation from the nearby tissues. (e) The upper and lower vas deferens before anastomosis. (f) Inner mucosal layer anastomosis by microdot technique using 10-0 nylon suture. (g) Muscular layer anastomosis by microdot technique using 9-0 nylon suture. (h) Outer adventitial layer anastomosis using 9-0 nylon suture. (i) Surgical window after vasovasostomy using the Moon’s clamp.
If a double-ringed Moon’s clamp was used, dissection and separation of the vas deferens and the nearby tissues was performed concurrently in one step, without significant injury, via simple manipulation of the position of the Moon’s clamp. The use of a sharp blade or diathermy was not required. This would result in reduced operation and recovery time, thereby minimising the possibility of postoperative complications. In most cases, approximately 10–15 minutes were spent for each side, from the initial formation of the scrotal incision to the dissection and separation of the vas deferens. After the surgical area of the vas deferens was resected segmentally, and the luminal status of the upper and lower vas deferens checked, the surgeons initiated a series of microsurgical procedures for vasovasostomy. Microscopic laboratory confirmation of the presence of sperm was performed only in cases where fluid was naturally oozing from the testicular vas during the course of the surgery. This was performed so that the results obtained in this study could be compared with those obtained in other studies involving long-term monitoring of patients.
In the present study, all patients who underwent mini-incision microsurgical vasovasostomy using a double-ringed Moon’s clamp had upper and lower vas deferens portions that were naturally close to each other. Thus, no accessory device was needed for an artificial approach and for fixation of the vas deferens. In addition, the supermicrosurgical vasectomy reversal was conducted as a three-layer anastomosis, using the microdot technique (five or six dots were placed with a blue methylene marker) proposed by Goldstein et al for better suture placement.(5) The anastomosis was done using 10-0 and 9-0 nylon sutures, under a surgical microscope with 10–15 times magnification. The mini-incision used in the surgery was maintained after the surgery. A single stitch, together with an additional small amount of local skin anaesthesia, was sufficient for suturing the incision, since the length of the incision did not exceed 10 mm (Figs.
RESULTS
The mean duration from the time of injection of a local anaesthetic agent into the skin and spermatic cord of the patient to the time dissection and separation of the bilateral vas deferens was completed in preparation for anastomosis was 25.5 (range 20–40) minutes. After resection of the previous vasectomy area in the separated vas deferens, vasovasostomy was performed as a three-layer anastomosis using the microdot technique under a surgical microscope. A mean duration of 72.6 (range 70–90) minutes was spent for both anastomoses; the end time was the time after the skin incision (< 10 mm in length) was sutured (by a single stitch) and dressed. All procedures were performed in an outpatient surgery unit, with spermatic cord anaesthetic block as the only method of anaesthesia used.(4) All patients were discharged on the day of surgery after approximately one hour of relaxation and observation. A total of 221 (84.0%) patients visited the CR Microsurgery Center for follow-up one day after the surgery, while other patients visited their local hospital. All but one patient had no haematoma or infection of the incision. The patients were allowed to return to their normal activities 24–48 hours after surgery, unless a particular trauma was applied to the scrotum, and to take a quick shower 48–72 hours after the surgery. They were prohibited from engaging in sexual activity for at least one month after the surgery. When the patients visited the CR Microsurgery Center for their first follow-up to check on the patency of the vas deferens one month after surgery, semen analysis was done. Results showed surgical success (i.e. vas deferens patency); motile sperms were detected in 182 (96.8%) of the 188 (71.5%) patients who complied with postoperative patient instructions.(8)
DISCUSSION
The first choice of natural fertility recovery after vasectomy may be vasectomy reversal. Patients’ concerns include the patency rate of the vas deferens after surgery, the duration of temporary suspension from work or daily social activities due to hospitalisation, and the extent of scarring and tissue injury from the skin incision. Other concerns include the possibility of significant complications that may occur due to an extended time in surgery under general or spinal anaesthesia, and the medical costs of treating these complications. These concerns may cause economically insecure patients to hesitate or delay undergoing surgical treatment.(9)
In order to achieve successful minimally invasive microsurgical vasectomy reversal under local anaesthesia without hospitalisation, the following conditions must be fulfilled: (a) the performing surgeon should be a skilled expert in high-level microsurgical techniques; (b) the skin incision made should be small to minimise tissue and vessel injury, and to ensure sufficient bleeding control; and (c) there should be good preparation (visualisation and isolation) of the length of both vasa deferentia and sufficient vascular supply for adequate anastomosis. Other than the aforementioned conditions, vas surgery devices with the following characteristics are also required for a successful, minimally invasive surgery: (a) a small instrument for the small surgical wound; (b) a non-sharp atraumatic instrument to avoid accidental tissue damage; and (c) an all-in-one instrument that enables certain processes to be completed in a single step, if possible.
To satisfy all the aforementioned conditions for a successful, minimally invasive surgery, this study did not adopt an extracutaneous approach for conventional no-scalpel vasectomy. In particular, devices such as the one-ringed clamp and sharp dissection forceps, which are traditionally used for no-scalpel vasectomy,(2) were not used. In general, no-scalpel vasectomy is associated with good outcomes under appropriate conditions, as reported by Li et al.(10) However, in cases where the patient has thick scrotal skin, a concealed scrotum due to lower abdominal obesity, a short, weak or thin vas deferens, or a vas deferens that is deeply positioned in the scrotum, no-scalpel vasectomy using an extracutaneous approach and sharp dissection devices may cause the surgical processes to be more challenging and result in unexpected serious complications.(11,12) Therefore, a percutaneous approach was used in the present study, so that a mini-incision could be made under various scrotal conditions and the shortest route to the vas deferens could be prepared.(3,11,12) A double-ringed Moon’s clamp was used to concurrently and conveniently dissect and separate the vas deferens without the use of a sharp blade or diathermy, while enabling exposure of a sufficient vas length for surgery.(1)
The Moon’s clamp has four distinguishing features. First, it has a ring with a diameter that is smaller than the length of the mini-incision, such that the device can be inserted into the incision, and the adjacent tissues, including the vas deferens, can be pulled out of the skin for exposure. Second, the outer and inner sides of the ring clamp have soft curved surfaces to minimise injury to the perivasal tissues when the clamp ring approaches the vas deferens via the incision. Third, the end tip of the clamp ring is designed to have the shape of a bird’s beak, with a smooth interface between the two rings. This makes it suitable for picking up and moving vessels and soft tissues without causing injury to these structures when the vas deferens is being separated via the dissection of the perivasal tissues. Fourth, it allows the dissection and separation of the vas deferens in one step using a single device with single-clamping; repeated clamping, which may be cumbersome or insecure, is unnecessary with this device (Figs.
Fig. 2
Photograph shows the double rings of the Moon’s clamp. The outer diameter of the major distal ring is 4 mm. The clamp is designed to minimise damage to adjacent tissue, thus allowing various types of surgical procedures involving the vas, including vasectomy and vasectomy reversal, to be performed safely.
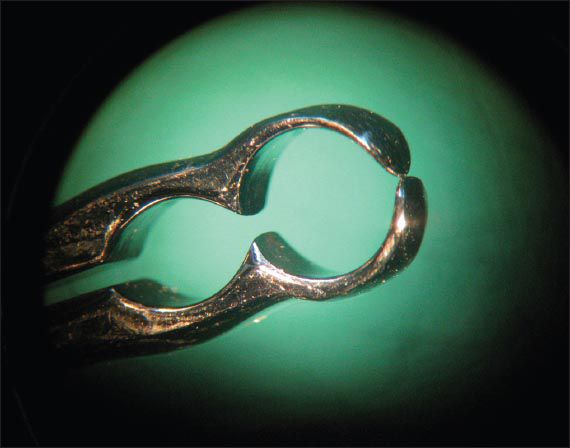
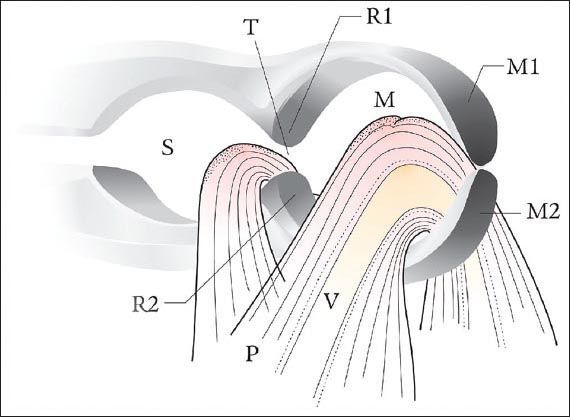
Fig. 3
Schematic diagram of the Moon’s clamp shows the main clamping zone (M) and the subclamping zone (S), which are divided by ridges (R1 and R2) that are formed at the boundary where the main clamps (M1 and M2) meet the subclamps. The throat (T) between the ridges allows the main clamping zone to communicate with the subclamping zone. It is preferable for the throat to have a width that is smaller than the diameter of the vas (V), in order to ensure that only the surrounding tissues (P) stripped from the vas can pass the throat. The ridges have sharpened tips at their distal ends. The selected sharpness of these tips is such that they are able to naturally strip the surrounding tissues from the vas without causing damage to the tissues as they are being moved into the subclamping zone. The flat inclined surfaces at the sides of the ridges facing the subclamping zone help to prevent any unwanted escape of the surrounding tissues from the subclamping zone to the main clamping zone.
Conventional accessory devices, such as a microvessel dilator and a vas approximator or holder (vasal approximating clamps), can be used to approach the upper and lower vas deferens for anastomosis of the vas deferens, to expand the inner diameter of the vas deferens and to prevent the masking of the anastomosed area by the surrounding adjacent tissues. However, in the present study, none of these accessory devices were required for the mini-incision microsurgical vasovasostomy using the double-ringed Moon’s clamp.
A dilator was not used in this study for the following reasons. First, the device dilates the lumen in such a way that the mucosa or the muscularis will be compressed, which may result in slight tearing or snapping of the mucosal ring. Second, a trained and experienced microsurgeon would have no difficulty performing the layer-to-layer anastomosis (starting from the inner mucosal layer) with accurate ratio and interval, without instrumental dilation. The reasons for not using an approximator are as follows. First, as the upper and lower bilateral vas deferens (exposed via the mini-incision) are sufficiently close together, even after resection of the previously resected area, no assistance using other accessory devices was needed for approximation. Second, if the most deeply positioned perivasal sheath of the exposed vas deferens is clamped with a small curved haemostat, an appropriate length required for anastomosis can be continuously maintained by preventing the sinking of the vas deferens into the scrotum. Third, in the case of an inexperienced surgeon performing the surgery, if the end of a hard cotton stick is inserted beneath the anastomosis and the vas deferens is rolled, the entire anastomosis can be secured under direct observation without pressure or microscopic tissue injury because of metallic adjuncts. In addition, since the upper and lower terminal vas regions are naturally in close proximity, and the area of anastomosis is already a sufficient distance away from the surrounding tissues, the use of accessory devices for the identification of the vas is not necessary.
Spinal or general anaesthesia is usually used in most cases of vasectomy reversal because of the wide surgical area and possible tissue injury associated with the procedure. As a result, patients who wish to undergo vasectomy reversal are often concerned about long-term hospitalisation and the medical costs involved. Minimally invasive microsurgical vasectomy reversal using a double-ringed Moon’s clamp, which has been used in convenient, real no-scalpel vasectomy, has the following advantages: minimal tissue injury; convenient and concurrent dissection and separation of the vas deferens; and high probability of successful microsurgical anastomosis in an outpatient surgery unit under local anaesthesia, without the use of other accessory devices. In other words, this surgical technique, which enables quick return to ordinary social activities and reduction of socioeconomic costs, could be a feasible option for vasectomy reversal.


