INTRODUCTION
Fish bones are the most commonly ingested foreign bodies in Singapore, accounting for up to 83.9% of ingested foreign bodies.(1) The use of chopsticks to consume fish, the personal habit of deboning fish in the mouth and denture usage in the elderly have been described as risk factors for the ingestion of fish bones.(2)
The first line of investigation after ingestion of fish bones would include plain radiography, but this was shown to have poor sensitivity of 23.5%–54.8%(3-5) and false negative rates of up to 40%.(6) An alternative radiological modality would be the barium study, but it is limited by its false negative rate of 40%–50%.(7) Furthermore, barium contamination can render subsequent examination and removal of the ingested fish bone more technically challenging. Therefore, the current gold standard radiological modality for diagnosis is fine-cut computed tomography (CT), which not only confirms the diagnosis and reveals associated complications but also boasts a superior sensitivity of 90.9%–100%.(4,5,8) One should, however, note the caveat that the use of oral or intravenous contrast during CT can obscure the presence of a fish bone.(8,9) Hence, for a patient with a high index of suspicion for fish bone ingestion, the ordering clinician should specifically communicate with the radiologist on the indication as well as the need for a non-contrast scan.
After the diagnosis of fish bone ingestion, endoscopic removal using laryngoscopy or oesophagogastroduodenoscopy (OGD) is usually sufficient in most cases, with surgery only required in less than 1% of patients. We herein present a series of patients who ingested fish bones and presented to a local tertiary hospital in Singapore, discussing the associated complications based on the location in the gastrointestinal tract where the bones were impacted.
UPPER GASTROINTESTINAL TRACT
The majority of ingested fish bones lodge in the upper gastrointestinal tract, most commonly in the oral cavity or pharynx.(10) A careful clinical examination of the oropharynx is required, followed by plain lateral neck radiography. Visualisation of fish bones is often challenging on plain radiography, with fish bones presenting as faint linear calcifications (
Fig. 1
(a) Plain radiograph shows a faint linear calcification suspicious of an ingested fish bone (arrow). (b) CT image of the same patient shows a linear opacity corresponding to the history of fish bone ingestion. The presence of extraluminal gas (arrow) posterior to the trachea also raises the suspicion of a localised perforation that was not detected on plain radiography.
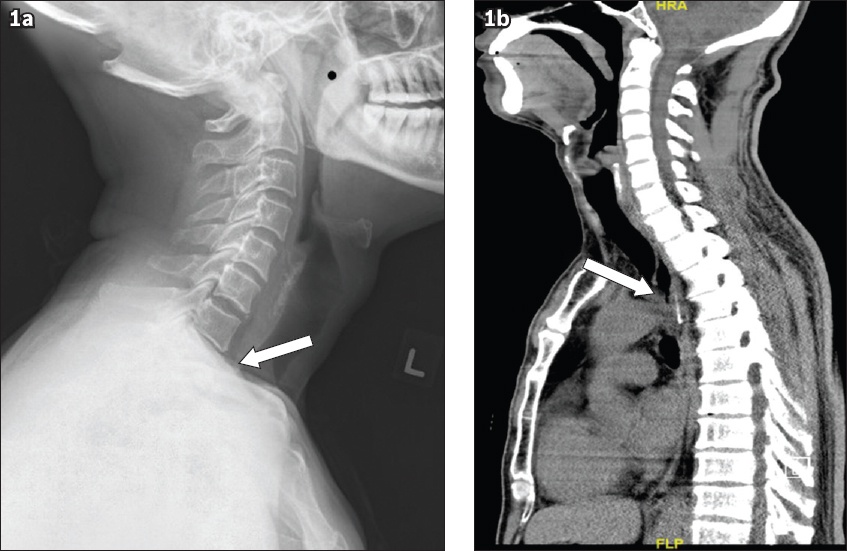
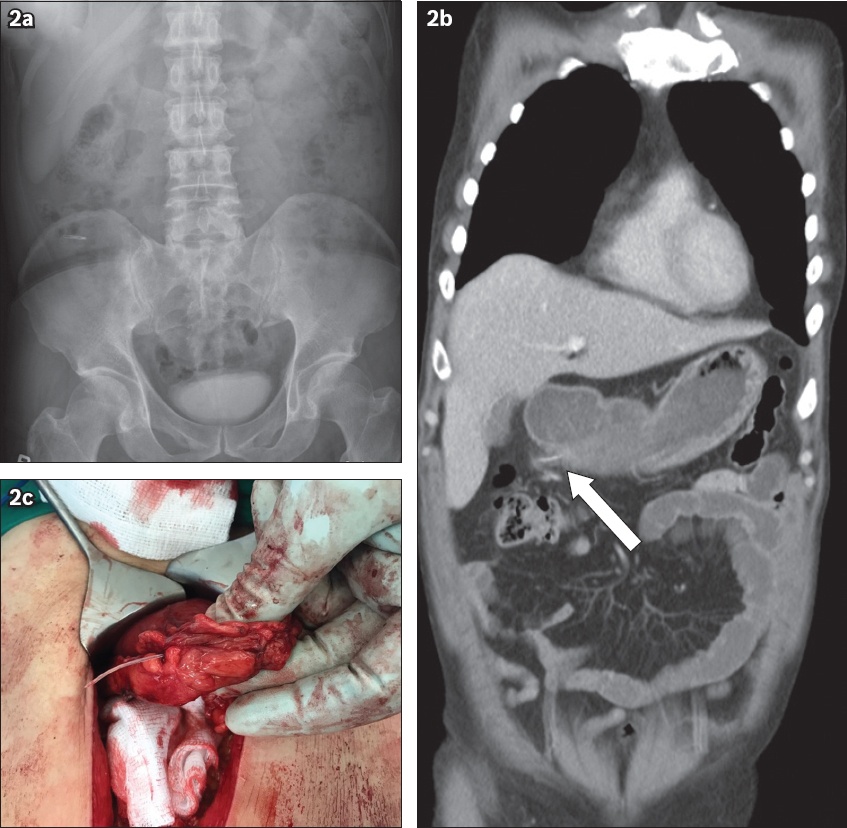
Fig. 2
(a) Abdominal radiograph shows a polypectomy clip seen in the right iliac fossa, with no other foreign body seen. (b) CT image of the abdomen shows a 3.2-cm curvilinear density that extends beyond the posterior wall of the gastric antrum (arrow), suggesting a perforation. (c) Photograph shows an exploratory laparotomy that confirmed fish bone perforation of the gastric antrum.
Removal by endoscope should be attempted for any ingested fish bone that is detected proximal to the jejunum and can be reached via endoscopy. This is in view of the potential for serious complications, such as perforation of the oesophagus and the stomach that may result in abscess formation or adjacent vascular injury.(11) Retrieval options include direct laryngoscopy, rigid oesophagoscopy or flexible OGD, depending on the location where the fish bone is impacted.
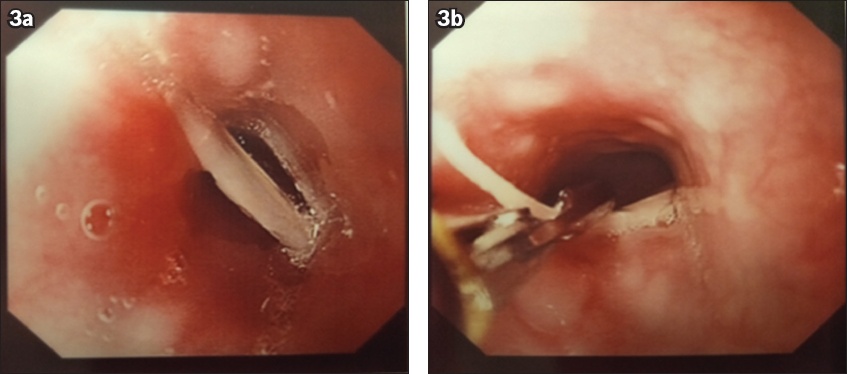
Fig. 3
(a) Oesophagogastroduodenoscopy image shows a fish bone lodged in the mid-oesophagus. (b) Endoscopy image shows the fish bone being retrieved using a pair of rat-tooth forceps.
SMALL BOWEL AND LOWER GASTROINTESTINAL TRACT
These patients are usually asymptomatic and present to the hospital only when complications occur. Most patients may even be oblivious to their history of recent fish bone ingestion,(12) and detection is usually made on CT performed to investigate abdominal pain. Similarly, the detection of fish bones in this part of the gastrointestinal tract with plain radiography is limited, as the majority of fish bones are radiolucent and obscured by the fluid and soft tissue of the abdomen.(13)
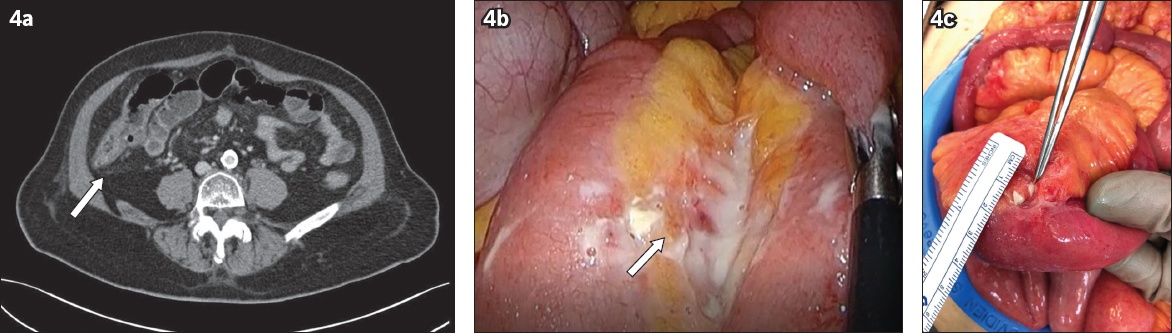
Fig. 4
A 52-year-old man presented with acute abdomen of one day’s duration, with no recollection of fish bone ingestion. (a) CT image of the abdomen shows non-specific stranding at the proximal ascending colon without any evidence of a foreign body (arrow). (b) Subsequent diagnostic laparoscopy shows interloop jejunal adhesions with purulent discharge (arrow). No perforation could be visualised on laparoscopy. (c) Laparotomy was subsequently performed as an aetiology was not identified on diagnostic laparoscopy. Photograph shows a 3-cm fish bone that perforated the mid-jejunum and was lodged in the mesentery.
COMPLICATIONS
Most ingested fish bones pass through the gastrointestinal tract uneventfully. However, the sharp edges of fish bones predispose the patient to serious complications such as perforation, migration and consequent infection when the fish bone is impacted in adjacent organs.
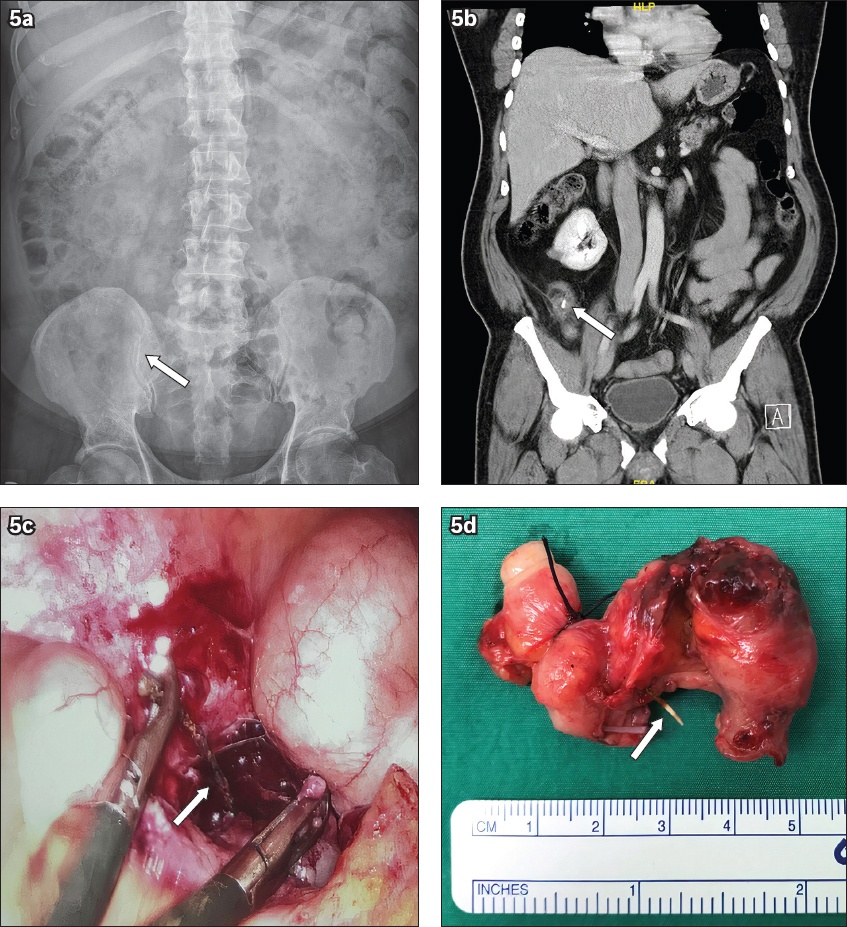
The most common complication, hollow viscus perforation, tends to occur at immobile segments of the gastrointestinal tract such as the ileocecal or rectosigmoid junction.(14) Unusual sites of perforation through a Meckel’s diverticulum or even the appendix (
Fig. 5
A 35-year-old man presented with right iliac fossa pain and fever. (a) Abdominal radiograph shows a curvilinear opacity projected over the right iliac fossa (arrow). (b) CT image shows acute appendicitis with a linear foreign body within the appendix lumen (arrow). (c) Diagnostic laparoscopy image shows a fish bone (arrow) penetrating through the posterior wall of appendix with localised abscess in the right iliac fossa identified. (d) Photograph shows the appendiceal specimen with the fish bone (arrow) lodged in the mid body.
Surgical intervention is almost certainly required in the event of perforation. The option of laparoscopic retrieval (
Fig. 6
A 65-year-old man presented with a history of fish bone ingestion and epigastric pain. (a) CT image shows a 2.1-cm linear density traversing the pyloric end of the stomach. (b) Laparoscopy image shows the removal of fish bone perforating stomach pylorus. The patient subsequently underwent omental patch repair of the site of perforation.
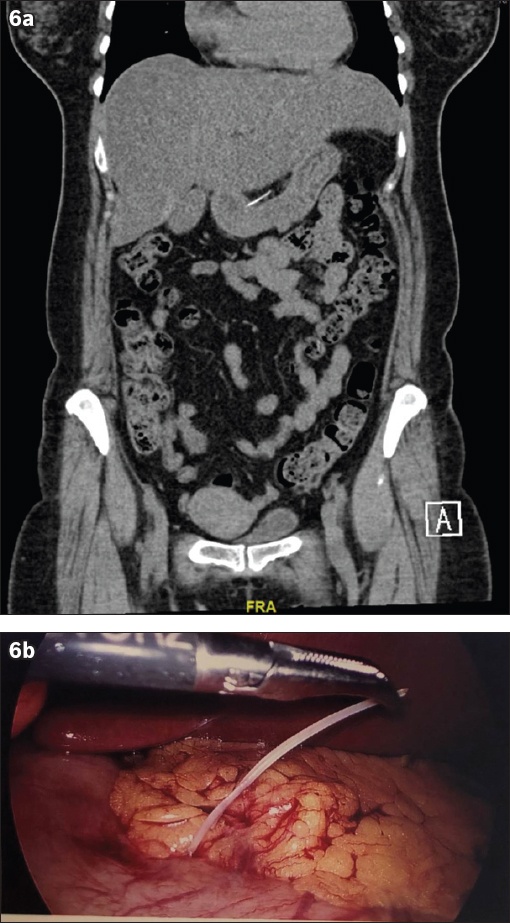
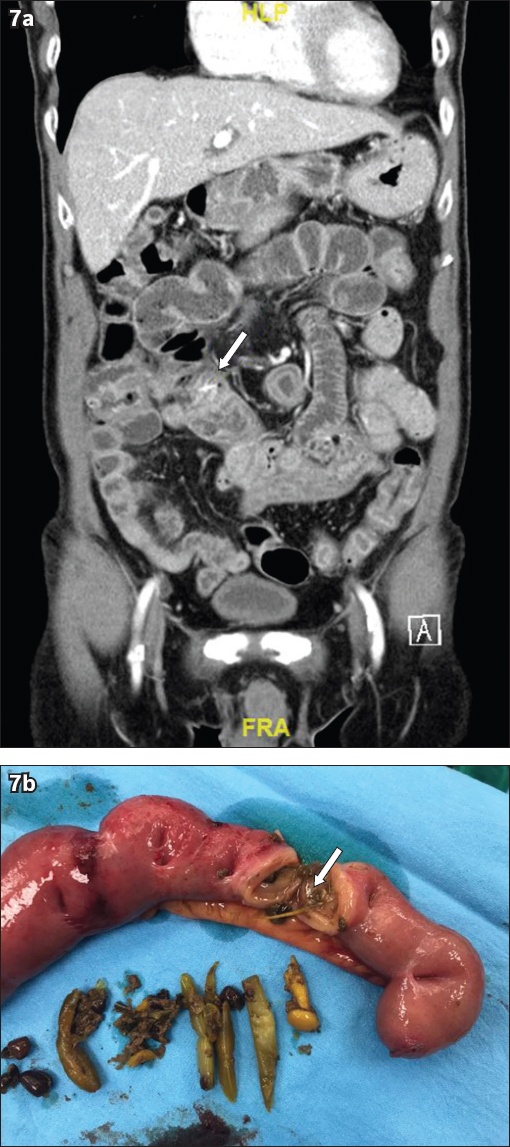
Fig. 7
A 70-year-old man with a history of descending colon cancer and open left hemicolectomy presented with three days of abdominal pain and guarding. (a) CT image shows a linear hyperdensity coupled with fat stranding and bowel thickening suggestive of a lodged fish bone (arrow). (b) Photograph shows the fish bone (arrow) that was identified following exploratory laparotomy and small bowel resection at the site of the perforation. Multiple adhesions along segment of resected bowel could explain why the fish bone was trapped at a point of narrowing, resulting in the perforation.
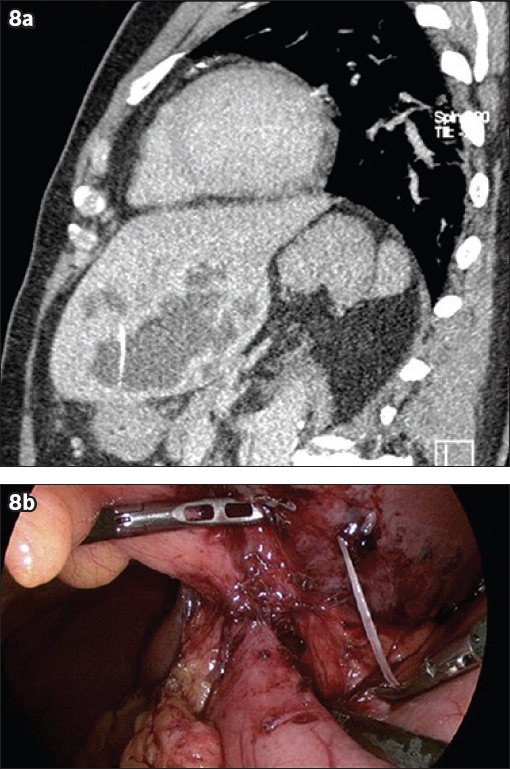
Another unusual complication would be the development of liver abscess (
Fig. 8
A 72-year-old man presented with a two-week history of fever, chills and diarrhoea. (a) CT image of the abdomen shows left hepatic liver abscess with linear density seen within the abscess cavity, likely representing a fish bone. (b) Diagnostic laparoscopy image shows the fish bone impacted on the undersurface of the left lobe of the liver; it was retrieved laparoscopically.
CONCLUSION
A high index of suspicion is required for a symptomatic patient with a recent history of fish consumption. CT should be performed even in the absence of radiographic findings due to its superior sensitivity in detecting fish bones. When complications of perforation occur, surgical options can include laparoscopy but with a low threshold for laparotomy to remove the foreign body and repair the site of perforation.
SMJ-61-583.pdf


