Dear Sir,
Neuromuscular electrical stimulation (NMES) is a treatment modality used in dysphagia management.(1,2) Owing to the limited research available on the capabilities and processes of surface electromyography (sEMG) and a combination of sEMG and NMES, clinicians are unsure about the usage of such modalities. Training programmes based on published and emerging research works have been adopted. With supporting research, standard placements of electrodes for NMES on the suprahyoid, infrahyoid and digastric muscles(1,2) for dysphagia management have been put in place. However, limited research has been conducted with regard to other options for placements.
Swallowing is a sensorimotor activity that is modulated at the level of the brainstem, influenced by both cortical and subcortical areas. There is bilateral cortical representation of the pharyngeal musculature, which explains the nature of the dysphagic symptoms, the underlying physiology and the recovery process in our patients. A recent study on stroke patients(3) concluded that stimulation of the bilateral thenar muscle leads to improved swallowing function and muscle activity. The outcomes were reportedly comparable to those observed in the study using repetitive transcranial magnetic stimulation.(4)
This case study reports the changes in swallowing noted in a patient with head and neck cancer after following a holistic management plan. The intervention involved swallowing, oral motor and voice exercises, and varied modalities such as sEMG and NMES along with stimulation of the lesser known thenar eminence in conjunction with stimulation of the suprahyoid muscle. The concept of pain was also taken into consideration for the usage of the electrodes at the thenar eminence.
A 56-year-old Chinese man presented with severe dysphagia post nasopharyngeal cancer that had been diagnosed more than 12 years prior to the consultation. He had undergone radiation therapy after left radical neck surgery. As his swallowing function was progressively deteriorating, resulting in poor voluntary intake and consequent extreme weight loss, feeding using a percutaneous endoscopic gastrostomy (PEG) tube was suggested by several specialists. The patient opted for the use of NMES as part of his treatment to aid his swallowing. He was advised to follow a regime involving a combination of modalities using suprahyoid and thenar eminence placement, and underwent an initial clinical assessment and functional endoscopic examination of swallowing (FEES).
The first clinical evaluation revealed severe oropharyngeal dysphagia with fibrosis of the neck muscles, generalised weakness, fasciculation of the tongue with minimal functional movement for swallowing and speech, poor speech intelligibility, delayed weak swallows, consistent coughing during meals owing to penetration of food/liquid into the airway and multiple swallowing attempts required to clear each bolus. The evaluation concluded that overall poor oral food intake had led to a referral for PEG tube feeding.
FEES evaluation supported the findings. The swallows were delayed and triggered at the level of the sinuses, and the white-outs for the swallows were poor. Minimal epiglottal movement was noted, with a glottal chink along the entire length of the vocal cords, and the left vocal cord was weaker than the right vocal cord. Pharyngeal wall movement on the left was also reduced. Aspiration risks were evident from the copious secretions in the pyriform sinuses and the patient’s inability to clear all of them despite multiple weak swallow attempts. He needed to use the compensatory mechanism of pharyngeal expectoration to clear the residue. The procedure revealed velopharyngeal incompetence and reduced sensation. At this point, the functional oral intake scale (FOIS) rating of the patient was 3.
A range of exercises and modalities were used throughout the treatment period, including oral motor exercises such as tongue stretches and jaw release; tongue strength training using the Iowa Oral Performance Instrument; NMES and sEMG using VitalStim Plus equipment; voice exercises such as loud vocalisations, vocal fold adduction exercises and gliding along the pitch scale; expiratory muscle strength training for follow-up at home and a home plan for oral motor exercises. FOIS,(5) a seven-point ordinal scale, was used as an outcome-measuring tool in this study, along with clinical bedside evaluations and FEES.
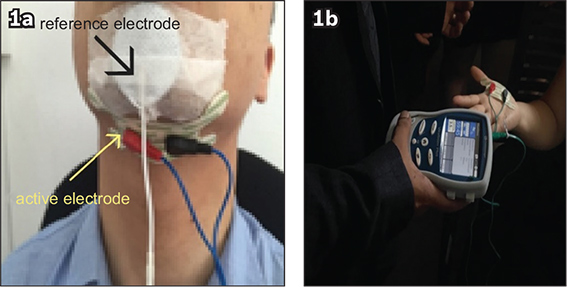
Following the initial FEES, the patient started therapy sessions at our outpatient clinic. He initially underwent daily therapy sessions (20 sessions) of NMES using Channel 1 electrodes on the suprahyoid region (
Fig. 1
Photographs show (a) suprahyoid and (b) thenar electrode placements in neuromuscular electrical stimulation.
The patient gained 2 kg of weight during the first three weeks of therapy. Clinical evaluation revealed an improvement in the latency of his swallows and a significant reduction in coughing episodes during meals. His oral intake started to build up, gradually reducing the time taken to complete a meal. His FOIS rating at the end of 20 sessions of therapy was 5. Repeat FEES revealed a reduction in post-swallow residue and improved white-out for swallows.
The patient continued to attend therapy thrice a week for the next three months, with each session lasting 45 minutes. The sessions involved the use of NMES with thenar eminence and suprahyoid placements. The intensity of the current was 7–8 mA when the electrode was placed on the suprahyoid muscle. For the second channel, the electrode was placed on the thenar prominence of the contralateral palm (
Significant clinical changes were observed on placement of the electrode on the thenar eminence and the suprahyoid muscle, which were confirmed based on the patient’s feedback. Clinically, his swallows were quicker and brisk, with improved hyolaryngeal excursions and less post-swallow residue to clear. He coughed minimally during meals, his intake of fluids improved, and he was able to tolerate a greater variety of foods and textures. The patient said that he was experiencing easier swallowing and that his tongue and oral musculature were feeling much more relaxed. His vocal quality improved, with increased volume, and his speech was more intelligible. During the second phase, he continued to gain weight and maintain it. As his immunity started to improve, he reported feeling less lethargic, and episodes of common colds and fever started to reduce. He was able to socialise much more and reported that the positive outcomes had improved his quality of life. The FOIS rating at the end of Phase 2 increased to 6.
We postulate that the additional improvements observed in the second phase of management could be attributed to the stimulation of the thenar eminence, which is known to reduce the excitability of the inhibitory networks of the motor cortex that influence the swallows. This finding is consistent with those reported in previous studies.(3)
Dysphagia associated with head and neck cancers is very common and tends to persist even after the tumour is removed or treated. The resulting functional deficits often tend to prolong and increase the magnitude of swallowing disorders, and patients tend to experience xerostomia; pain; loss of energy; impaired sensation of taste, smell and hearing; trismus; dental issues; dysarthria and voice disorders. Traditional therapy methods have limited benefits, and patients often have to live with challenges related to communication and feeding. Quality-of-life measures, which are often not studied in detail, have a direct implication for societies where food plays an important role in the social facets of day-to-day living. This case study highlights the value of an eclectic approach using NMES with novel electrode placements and sEMG in the management of severe dysphagia, enhancing overall therapy outcomes, including the quality of life. Incorporation of stimulation of the thenar eminence is promising; however, more case studies in this regard are warranted across different aetiological groups.


