Abstract
Acute cholecystitis is a common cause of right upper quadrant pain in patients presenting at the emergency department. Early diagnosis and recognition of associated complications, though challenging, are essential for timely management. Imaging studies, including ultrasonography, computed tomography and magnetic resonance imaging, are increasingly utilised for the evaluation of suspected cases of cholecystitis. These investigations help in diagnosis, identification of complications and surgical planning. Imaging features of acute cholecystitis have been described in the literature and are variable, depending on the stage of inflammation. This article discusses the spectrum of cholecystitis-associated complications and their imaging manifestations. We also suggest a checklist for the prompt and accurate identification of complications in acute cholecystitis.
INTRODUCTION
Acute cholecystitis is an acute inflammatory condition of the gallbladder; 95% of cases of acute cholecystitis are due to an obstructing calculus in the gallbladder neck or cystic duct.(1) Obstruction of the cystic duct results in an overdistension of the gallbladder and a rise in intraluminal pressure. This increased pressure, along with cholesterol-supersaturated bile, triggers an acute inflammatory response. Gallstones contribute to the inflammatory response by stimulating prostaglandins I2 and E2.(2) Secondary bacterial infection is present in 20% of cases of acute cholecystitis. Mural ischaemia resulting from the increased intraluminal pressure may also contribute to complications such as gangrenous cholecystitis and perforation.(3) Pathologically, there are three stages of inflammatory disease: (a) oedematous cholecystitis; (b) necrotising cholecystitis; and (c) suppurative cholecystitis.(1)
Due to the wide availability of computed tomography (CT) scanners in emergency departments, increasing numbers of patients undergo CT examinations for suspected acute cholecystitis. Ultrasonography (US) remains the preferred initial imaging modality for the evaluation of suspected acute calculous cholecystitis due to its relatively low cost, easy accessibility, short examination duration and lack of ionising radiation (
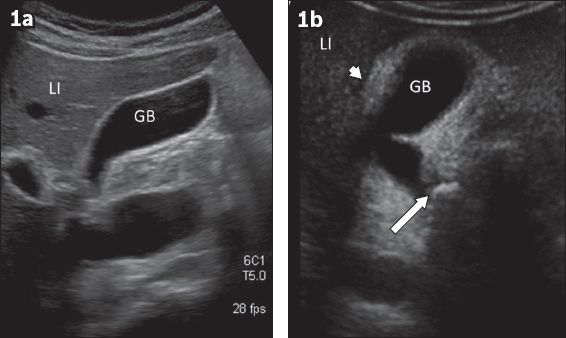
Fig. 1
Oblique coronal US images show (a) a normal gallbladder (GB); and (b) a thickened GB wall and thin layer of pericholecystic fluid (arrowhead), with an impacted calculus in the neck of the GB (arrow) in a patient with acute cholecystitis. LI: liver
CT OF ACUTE CHOLECYSTITIS AND ASSOCIATED COMPLICATIONS
CT features of uncomplicated acute cholecystitis include a combination of overdistended gallbladder, mural thickening, mural enhancement, pericholecystic fat stranding and pericholecystic fluid.(6,7) Characteristically, there is an enhancement rim in the adjacent liver.(8) Classically, a calculus can be seen impacted in the gallbladder neck or cystic duct (
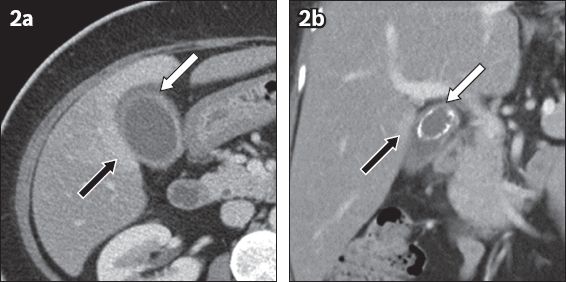
Fig. 2
CT images of classical acute calculous cholecystitis show (a) a thickened enhancing gallbladder wall, pericholecystic fat stranding (white arrow) and reactive hyperaemia in the adjacent liver (black arrow) in the axial plane; and (b) a large calculus in the neck of the gallbladder (white arrow) and reactive hyperaemia (black arrow) in the adjacent liver in the coronal plane.
Gangrenous cholecystitis results from the downhill course of an episode of acute cholecystitis and occurs in up to 39% of patients with acute calculous cholecystitis.(12) It is associated with higher morbidity and mortality rates than uncomplicated acute cholecystitis. Elderly patients, and patients with a history of diabetes mellitus and white blood cell count > 15,000 cells/mL are at an increased risk of having gangrenous changes at presentation.(12) In addition to the typical imaging features of cholecystitis, CT findings of poorly enhancing walls, intraluminal membranes, striated and reduced mural enhancement, focal mural defects and pericholecystic abscesses have been described in cases of gangrenous cholecystitis, with specificity close to 90% (Figs.
Fig. 3
Axial CT image of acute gangrenous cholecystitis shows thickened walls and focal defects (black arrow) in an enhancing mucosa with hyperdense sloughed mucosa floating in the dependent gallbladder (white arrow). Note the ‘sunburst’ pattern of pericholecystic fat stranding.
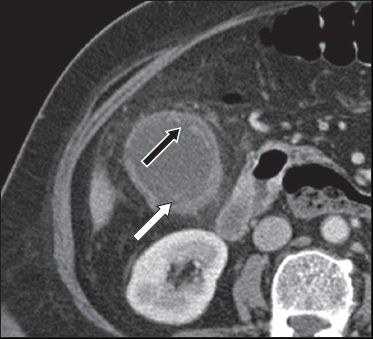
Fig. 4
Axial CT images of acute gangrenous cholecystitis show (a) a poorly enhancing gallbladder wall (black arrows) and a striated appearance of the medial wall (white arrow); and (b) poorly enhancing walls (black arrow) and a calculus (white arrow) impacted in the neck of the gallbladder. Note the presence of a few other gallstones.
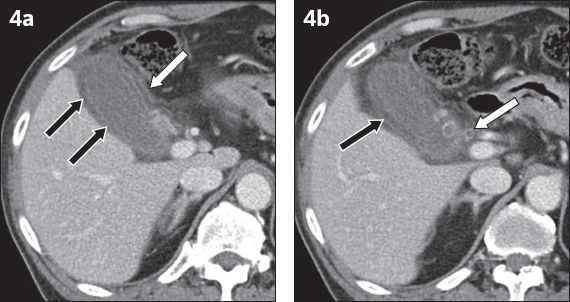
Fig. 5
Evolving gangrenous cholecystitis in a 34-year-old man presenting with right hypochondrial pain. (a) Axial CT image on the day of presentation shows poor enhancement of the gallbladder wall (black arrow). No gallstone or definite cholecystic fat stranding was identified, and the patient was kept on conservative management. (b) Axial CT image on Day 3 shows a poorly enhancing wall (black arrow) and pericholecystic fat stranding (white arrow). (c) Axial CT image on Day 10 shows intramural abscesses (white arrows), a sign of gangrenous cholecystitis. The patient underwent urgent cholecystectomy, which confirmed gangrenous cholecystitis with mucosal ulcers and mural abscesses.
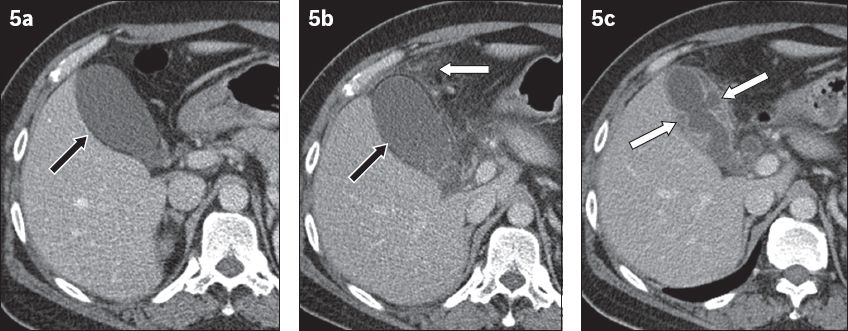
Fig. 6
Evolving gangrenous cholecystitis in a 55-year-old woman. (a) Axial CT image on the day of presentation shows pericholecystic inflammation and fluid with a focal bulge in the gallbladder wall (arrow). (b) CT image after one week of conservative treatment shows an increase in the size and number of bulges (arrows). (c) Axial T2-HASTE MR image one day after the second CT shows a further increase in the number of bulges (arrows). Laparotomy findings confirmed gangrenous cholecystitis with extensive inflammation around the gallbladder. Histopathological examination confirmed that these bulges corresponded to mucosal ulcers with mural abscesses.
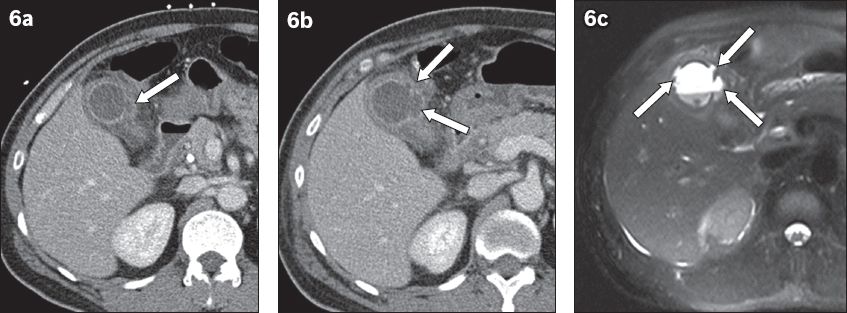
Fig. 7
Intrahepatic perforation of the gallbladder. Axial CT image depicts a large hepatic abscess (white arrow) with air pockets. Outline of the neck of the gallbladder is identified (black arrow), but the rest of the gallbladder is not seen as separate from the abscess.
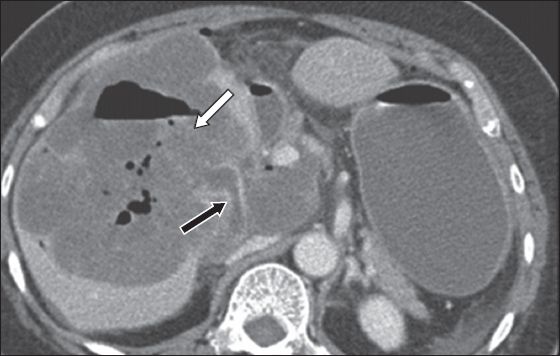
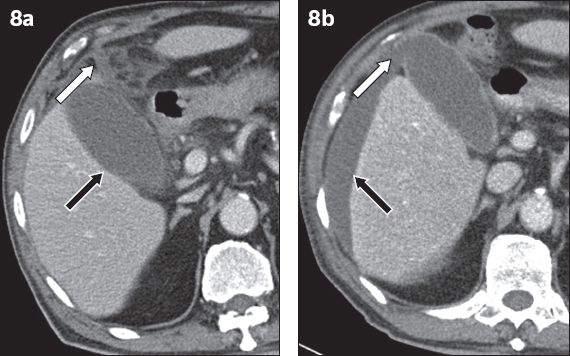
Fig. 8
Perforated cholecystitis in a 70-year-old woman presenting with abdominal pain at the emergency department. (a) Axial CT image shows a poorly enhancing gallbladder wall (black arrow), with pericholecystic fat stranding and minimal fluid (white arrow). (b) CT image after two days, due to worsening symptoms, shows a wall defect in the fundus of the gallbladder (white arrow) with a significant increase in perihepatic fluid (black arrow).
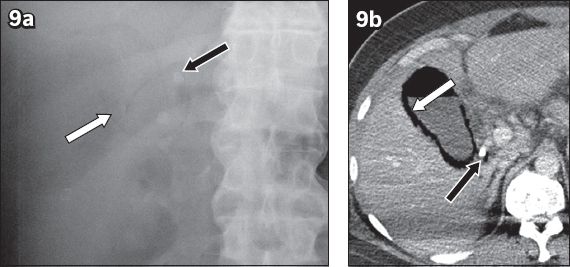
Emphysematous cholecystitis refers to the presence of gas in the gallbladder wall and is secondary to infections by gas-forming organisms such as Clostridium welchi. Patients with diabetes mellitus are at a greater risk of developing this condition and may present initially with relatively milder symptoms. Plain radiography often shows the gallbladder wall being outlined by radiolucent gas (
Fig. 9
Emphysematous cholecystitis. (a) Supine abdomen radiograph shows a pear-shaped curvilinear lucent line (white arrow) in the right upper quadrant with two radiopacities (black arrow) within it. (b) Axial CT image shows gas within the wall (white arrow) and in the lumen of the gallbladder. There is an impacted calculus in the gallbladder neck (black arrow).
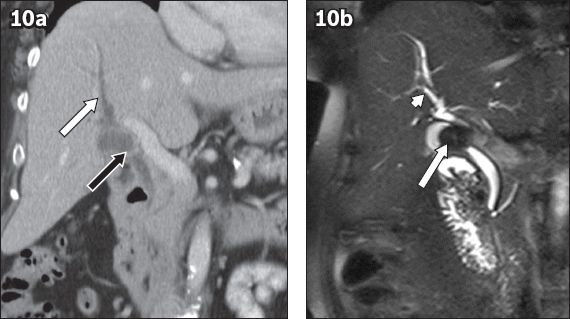
Mirizzi syndrome results from an impacted gallstone in the gallbladder neck or cystic duct that causes extrinsic compression of the common hepatic duct. The result is biliary obstruction with dilatation of the intrahepatic bile ducts. A cholecystocholedochal fistula may form due to recurrent inflammation around the impacted gallstone in the cystic duct. Patients with this condition often present with abdominal pain, fever and jaundice, without any pathognomonic pattern, which therefore makes clinical diagnosis difficult.(16) Preoperative diagnosis of Mirizzi syndrome is essential in planning surgeries, in view of the possibility of open cholecystectomy. CT can show the dilated intrahepatic bile ducts with the common bile duct of normal calibre (
Fig. 10
Mirizzi syndrome in a 42-year-old woman presenting at the emergency department with fever and abdominal pain. (a) Coronal CT image shows a bulbous expansion of the neck of the gallbladder, due to a radiolucent calculus compressing the proximal hepatic duct (black arrow), with resultant dilatation of the central intrahepatic ducts (white arrow) but a normal distal duct. (b) Coronal MRCP image shows a large gallstone (arrow) compressing the proximal hepatic duct, with dilatation of the central intrahepatic ducts (arrowhead).
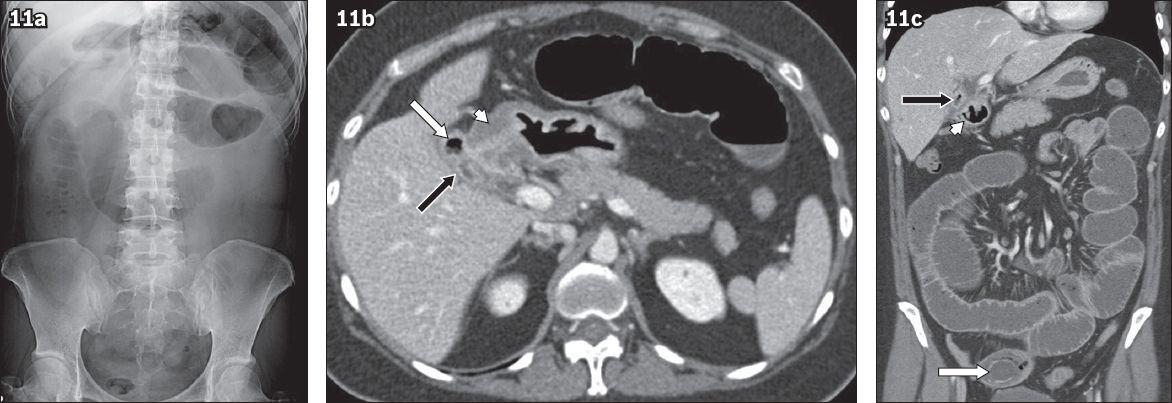
Gallstone ileus is a rare complication associated with a subclinical or milder episode of cholecystitis. Instead of right upper quadrant pain, the patient presents at the emergency department with signs and symptoms of bowel obstruction.(19) Intestinal obstruction is the outcome of an impacted ectopic gallstone, usually in the distal ileum. These gallstones are usually larger than 2.5 cm and enter the gastrointestinal tract via a fistulous communication between the gallbladder and duodenum or, in rare occasions, between the gallbladder and stomach.(20) Smaller gallstones may pass through the bowel loops asymptomatically without causing obstructions. CT, which can show Rigler’s triad (small bowel obstruction, ectopic gallstone at point of transition and pneumobilia), is useful for accurate diagnosis of gallstone ileus.(21) Based on our experience, the absence of pneumobilia with equivocal features of gallbladder inflammation can be misleading for the radiologist. In such cases, the typical appearance of gallstones in the dilated small bowel proximal to the transition point provides a clue for diagnosing gallstone ileus (
Fig. 11
Gallstone ileus in a 39-year-old man presenting at the emergency department with features of subacute bowel obstruction. (a) Supine abdominal radiograph shows dilatation of small bowel loops in the central abdomen. (b) Axial CT image shows a contracted gallbladder with a thickened wall (black arrow), with air in its lumen (white arrow). The gallbladder is inseparable from the first part of duodenum (arrowhead), and the duodenal wall is oedematous. (c) Coronal oblique CT image shows small bowel dilatation with a large peripherally calcified gallstone in the distal ileum (white arrow). The ileum distal to the gallstone is collapsed. Note the contracted, air-containing gallbladder (black arrow) abutting the proximal duodenum (arrowhead).
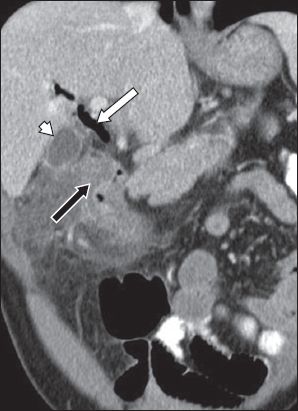
Cholecystoenteric fistulas can develop in the setting of acute cholecystitis without a small bowel obstruction or ectopic gallstone. They can also develop due to trauma, peptic ulcer disease, inflammatory bowel disease and malignancy of the bowel and gallbladder.(23) It has been postulated that recurrent cholecystitis leads to adhesions between the gallbladder and bowel, with subsequent fistula formation.(24) Diagnosis of cholecystoenteric fistulas is important for surgeons but difficult for radiologists, particularly in the presence of a contracted gallbladder. We recommend that in the presence of unexplained pneumobilia, the relationship of the gallbladder with respect to the adjacent bowel should be evaluated. In demonstrating fistulas, multiplanar reconstructions are more helpful than conventional axial imaging (
Fig. 12
Acute cholecystitis with cholecystoenteric fistula. Coronal oblique CT image shows a contracted gallbladder (arrowhead) with pericholecystic fluid and inflammation with pneumobilia (white arrow), abutting an oedematous proximal duodenum (black arrow). Laparotomy confirmed a fistulous communication between the gallbladder and the first part of the duodenum.
We have summarised the CT findings in various complications associated with acute cholecystitis (
Table I
Summary of computed tomography findings in acute cholecystitis and associated complications.
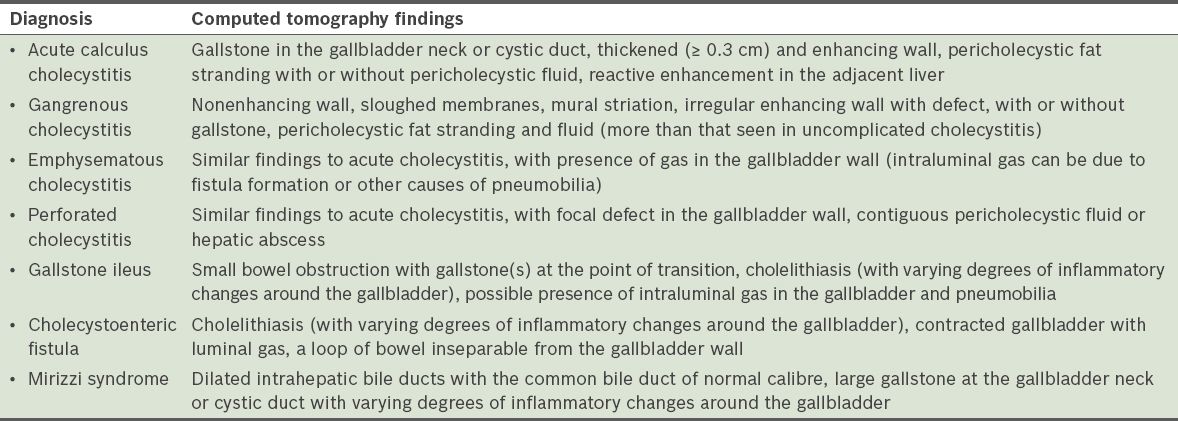
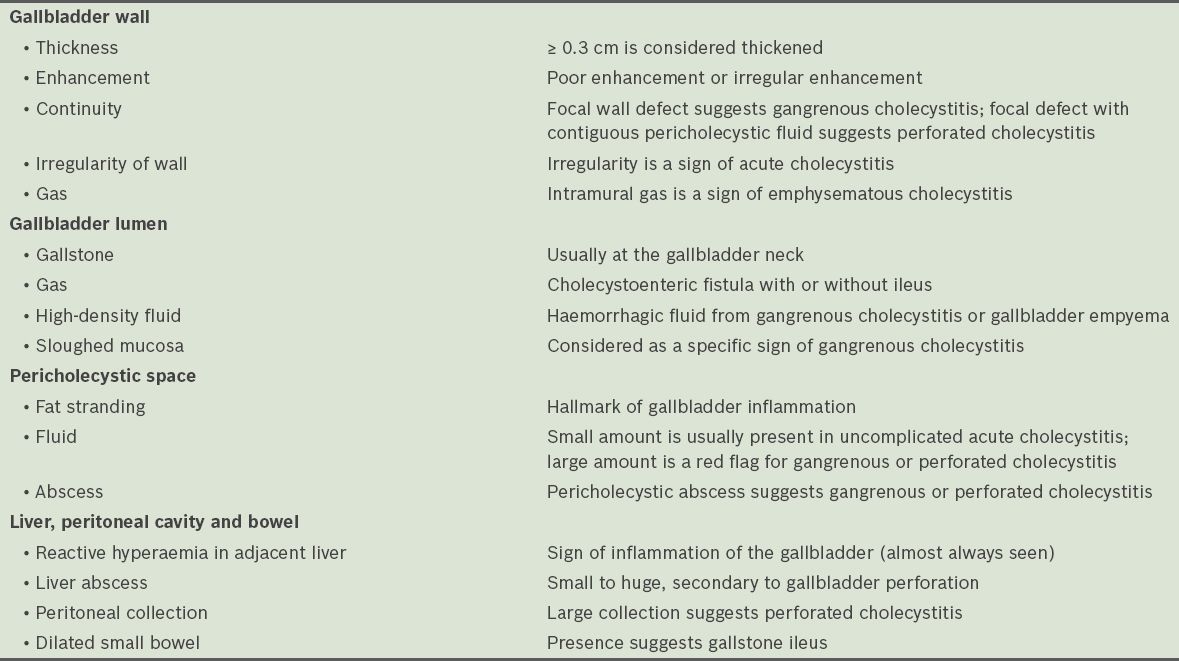
Table II
Checklist for identification of complications from cholecystitis.
CONCLUSION
Patients with acute cholecystitis, as well as those with associated complications, present at the emergency department with nonspecific symptoms, such as pain in the right upper quadrant. The severity of clinical presentation may not be representative of the underlying complications. Cross-sectional imaging is critical in identifying the complications associated with acute cholecystitis. Familiarity with the spectrum of relevant imaging features, as presented here, is imperative for the emergency radiology team.


