INTRODUCTION
Immunoglobulin G4-related disease (IgG4-RD) is predominantly diagnosed through serum IgG4 levels and biopsy findings, although imaging findings can provide clues to the diagnosis. IgG4-RD is a systemic disease characterised by abundant infiltration of IgG4-positive plasma cells and lymphocytes as well as storiform fibrosis.(1,2) The serum IgG4 level is often, but not always, elevated in patients with IgG4-RD. However, serum IgG4 level may also be elevated in other diseases, including microscopic polyangiitis and granulomatosis with polyangiitis; therefore, elevation of serum IgG4 level is not a specific finding for IgG4-RD.(3) IgG4-RD often involves multiple organs and may mimic malignancy, infection or other autoimmune diseases. Differentiating IgG4-RD from malignancy is crucial, because many cases show good response to corticosteroid therapy. IgG4-RD can cause organ failure(1) and thus must be diagnosed promptly and accurately. It is important to be familiar with the imaging findings of IgG4-RD, as it may present with characteristic findings on computed tomography (CT) and magnetic resonance (MR) imaging. The most important step in diagnosing IgG4-RD is performing a systematic survey while carefully considering all the varied presentations of the disease, because some imaging findings are non-specific for IgG4-RD. We should be aware of the fact that most cases have multi-organ lesions, especially in autoimmune pancreatitis. Thus, this study aims to describe the wide range of CT and MR imaging findings of IgG4-RD across the whole body.
INTRACRANIAL FINDINGS
Hypertrophic pachymeningitis
Hypertrophic pachymeningitis is a rare but increasingly recognised manifestation of IgG4-RD. The most common symptom is headache, and visual or hearing impairment can occur owing to local dural involvement in the periorbital areas or vestibular structures.(4) On CT and MR imaging, it may appear as a linear dural thickening with homogeneous enhancement (
Fig. 1
(a) Immunoglobulin G4 (IgG4)-related hypertrophic pachymeningitis in a 49-year-old man with a history of autoimmune pancreatitis who presented with diplopia and abducens nerve palsy. Contrast-enhanced coronal MR image shows linear dural thickening with homogeneous enhancement (white arrows). (b) IgG4-related hypophysitis in a 61-year-old man with a history of autoimmune pancreatitis who presented with thirst, polydipsia and polyuria. Unenhanced sagittal T1-W image shows an enlarged pituitary stalk (black arrow) with no swelling of the anterior pituitary gland. A loss of high signal intensity in the posterior pituitary gland is also observed.
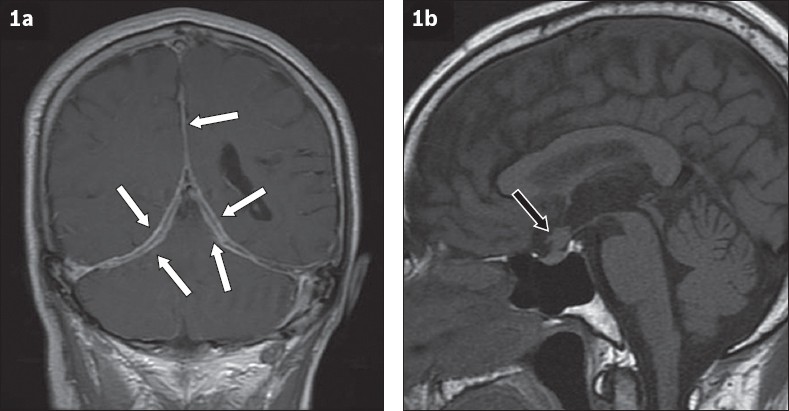
Pituitary gland
IgG4-RD represents one type of hypophysitis, based on histopathologic appearance.(2) The most common symptoms are hypopituitarism (e.g. weight loss, fatigue and appetite loss), diabetes insipidus and headache.(5) A typical MR imaging finding is pituitary gland enlargement, especially pituitary stalk thickening or a mass (
HEAD AND NECK
Perineural disease
IgG4-RD can involve the peripheral nervous system, especially the branches of the trigeminal nerve; therefore, careful evaluation along the course of the cranial nerves is crucial.(2,6) Symptoms are related to other organ lesions or mass effects of peripheral nerve lesions.(7) On MR imaging, perineural disease is characterised by distinct masses along the affected nerve fascicles or enlarged nerves.(2,7) These lesions show hypointense signal on T2-W imaging, reflecting fibrosis (
Fig. 2
IgG4-related perineural disease in a 50-year-old woman with visual impairment. (a) Contrast-enhanced coronal MR image shows diffuse enlargement of the ophthalmic (white arrows) and maxillary (black arrows) nerves with homogeneous enhancement. (b) T2-W MR image shows enlarged ophthalmic nerves with a relatively hypointense signal (arrowheads).
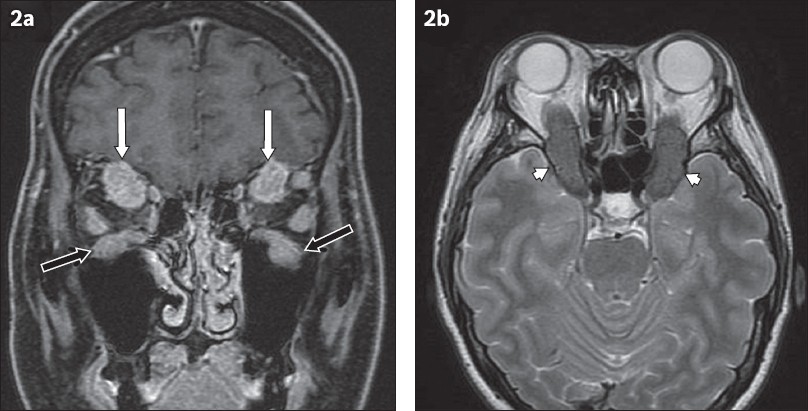
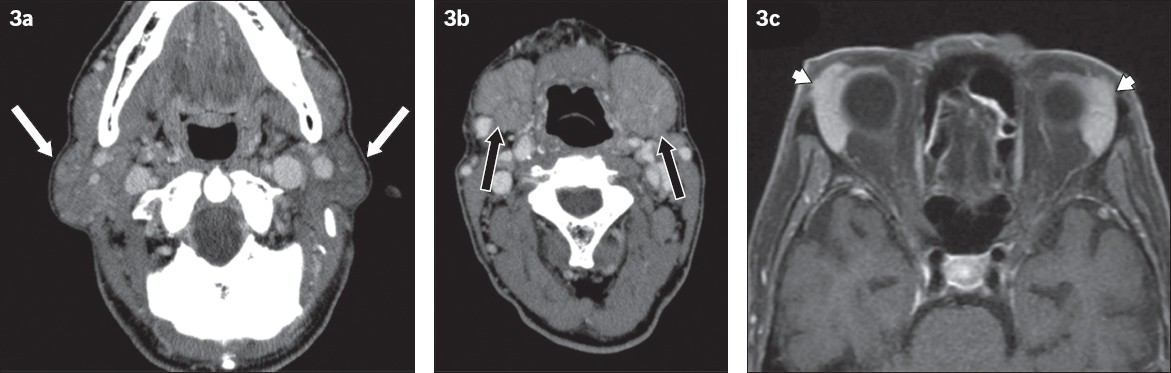
Salivary and lacrimal glands
The salivary glands are the most frequently involved organs in IgG4-RD of the head and neck area.(2) Involvement of the lacrimal glands often accompanies salivary gland lesions. Mikulicz’s disease and Küttner’s tumour, both of which are well-known in this area, are now considered a part of the spectrum of IgG4-RD.(2,6,8) Mikulicz’s disease is characterised by bilateral painless swelling of at least two of the lacrimal, submandibular and parotid glands.(2,6,8) Küttner’s tumour, also known as chronic sclerosing sialadenitis, was originally described as unilateral or bilateral hard swelling of the submandibular glands.(2,6,8) It is challenging to distinguish Mikulicz’s disease and Küttner’s tumour owing to their similar imaging findings. IgG4-related salivary and lacrimal gland lesions demonstrate bilateral gland swelling with relatively low signal intensity on T2-W imaging and homogeneous enhancement due to fibrosis (
Fig. 3
IgG4-related dacryoadenitis and sialadenitis in a 74-year-old man who presented with bilateral submandibular swelling. Contrast-enhanced CT images of the (a) parotid glands and (b) submandibular glands show bilateral parotid (white arrows) and submandibular gland swelling (black arrows). (c) Contrast-enhanced MR image shows bilateral lacrimal gland swelling with homogeneous enhancement (arrowheads).
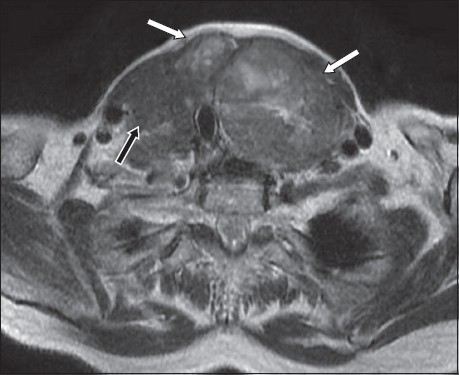
Thyroid
An association between IgG4-RD and thyroid diseases, including Hashimoto’s thyroiditis, Riedel’s thyroiditis and Graves’ disease, has recently been described.(9) Hashimoto’s thyroiditis is thought to consist of two subtypes: IgG4-related thyroiditis and non-IgG4 thyroiditis.(2,9) Riedel’s thyroiditis is commonly considered to be IgG4-RD with extensive fibrosis, resulting in a hard, painless mass that involves the thyroid parenchyma and surrounding tissues. Compressive symptoms are the most common, including dyspnoea, hoarseness of voice and dysphagia.(9) CT reveals either focal or diffuse low attenuation of the thyroid, with minimal contrast enhancement relative to the surrounding thyroid tissue. These lesions can have a hypointense signal on T2-W imaging, resulting from fibrosis (
Fig. 4
IgG4-related thyroiditis in an 81-year-old woman who presented with neck swelling and dyspnoea. T2-W image shows multiple heterogeneous masses in both thyroid lobes (white arrows). A hypointense mass is also observed in the right lobe (black arrow). Biopsy of the mass was performed, revealing a diagnosis of IgG4-related thyroiditis.
CHEST
Various conditions have been identified at several sites in the thoracic area, including the lungs, mediastinal lymph nodes, bronchial walls and pleura. These have been comprehensively classified as IgG4-related respiratory disease.(10) Generally, patients have non-specific symptoms that include cough, dyspnoea or chest pain, and they can also be asymptomatic.(10) Common CT findings include thickening of the bronchial wall (
Fig. 5
(a & b) IgG4-related respiratory disease in a 74-year-old man who presented with bilateral submandibular swelling (same case as
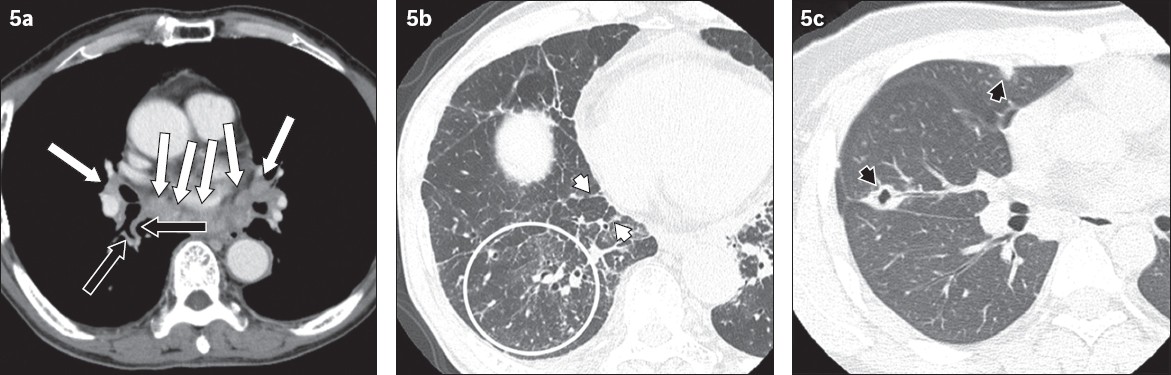
Fig. 6
IgG4-related paravertebral lesions in a 50-year-old woman with visual impairment (same case as
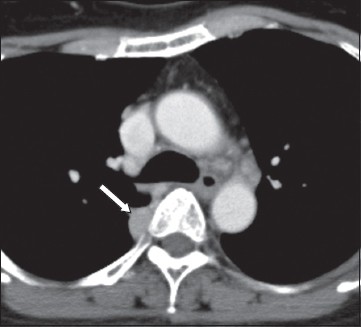
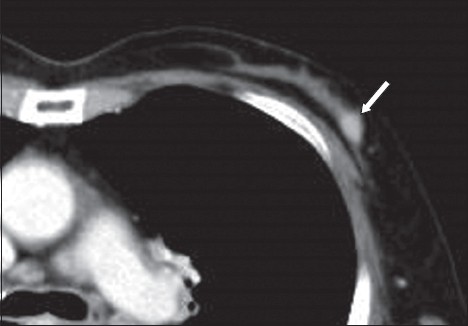
BREAST
Breast involvement in IgG4-RD (IgG4-related sclerosing mastitis) is uncommon. Most patients are asymptomatic, but some may have a painless palpable lesion.(8) On imaging, it presents as a non-specific lesion with contrast enhancement (
Fig. 7
IgG4-related sclerosing mastitis in an asymptomatic 75-year-old woman experiencing a relapse of autoimmune pancreatitis. Pre-treatment contrast-enhanced CT image shows a well-demarcated enhanced mass in the left breast (arrow). This lesion decreased in size after corticosteroid therapy (not shown).
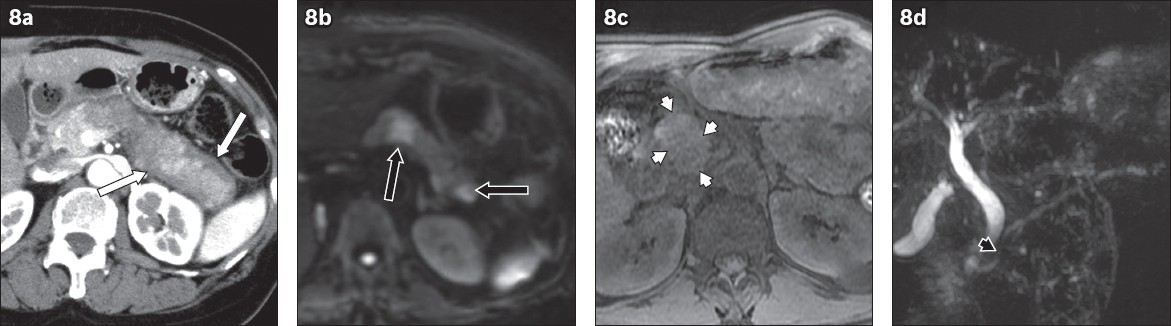
PANCREAS
Autoimmune pancreatitis (AIP) is the most common lesion in IgG4-RD, because the concept of IgG4-RD was originally established based on intense study of AIP.(1) There are two subtypes of AIP based on pathological findings: Type 1, lymphoplasmacytic sclerosing pancreatitis and Type 2, idiopathic duct-centric chronic pancreatitis.(6,12) Type 1 is the pancreatic manifestation of IgG4-RD, whereas Type 2 has distinctly different histologic and clinical features without elevation of serum IgG4 or autoantibodies.(6,12) Patients may have abdominal pain, obstructive jaundice, weight loss or new-onset diabetes mellitus, and some patients have no symptoms. There are two imaging patterns of AIP: diffuse and focal.(6) Diffuse type is the more common pattern that is characterised by a diffusely enlarged pancreas with the absence of normal lobulated contours, giving it a sausage-like appearance.(6,8,12) The affected area has a hypovascular appearance on arterial phase CT (
Fig. 8
(a) Autoimmune pancreatitis (diffuse type) in an asymptomatic 54-year-old woman with elevated serum pancreatic enzymes. Pancreatic phase CT image shows a diffusely enlarged pancreas and the absence of normal lobulated contours (sausage-like appearance) from the pancreas body to the tail. The affected area appears as a heterogeneous hypovascular lesion compared to the pancreas head. A capsule-like rim is observed surrounding the affected area (white arrows). (b) Autoimmune pancreatitis (multifocal type) in an asymptomatic 70-year-old woman in whom a pancreatic mass was incidentally detected by US imaging (not shown). Diffusion-weighted MR image (b = 1,000 s/mm2) shows two hyperintense lesions in the pancreas tail (black arrows). (c & d) Autoimmune pancreatitis (focal type) in an asymptomatic 72-year-old man. CT images performed for another disease incidentally detected a pancreatic mass. (c) Unenhanced fat-saturated T1-W image shows dotted hyperintense areas in the hypointense mass (white arrowheads). (d) MR cholangiopancreatography image shows penetration of the pancreatic duct through the mass (duct penetrating sign, black arrowhead).
BILIARY SYSTEM
The structures of the biliary system are commonly involved in IgG4-RD. IgG4-related sclerosing cholangitis (IgG4-SC) can affect both the intrahepatic and extrahepatic bile ducts, and the main differential diagnoses are primary sclerosing cholangitis and cholangiocarcinoma.(6,8,12) Biliary involvement is observed in 60%–80% cases of Type 1 AIP, and Type 1 AIP is frequently associated with cholangiopathy and biliary tree involvement.(13) The portion on pancreas and biliary involvement is a continuum. The most common presentation of IgG4-SC is obstructive jaundice. On CT and MR imaging, IgG4-SC shows circumferential symmetric wall thickening of the bile ducts, with smooth outer and inner margins (
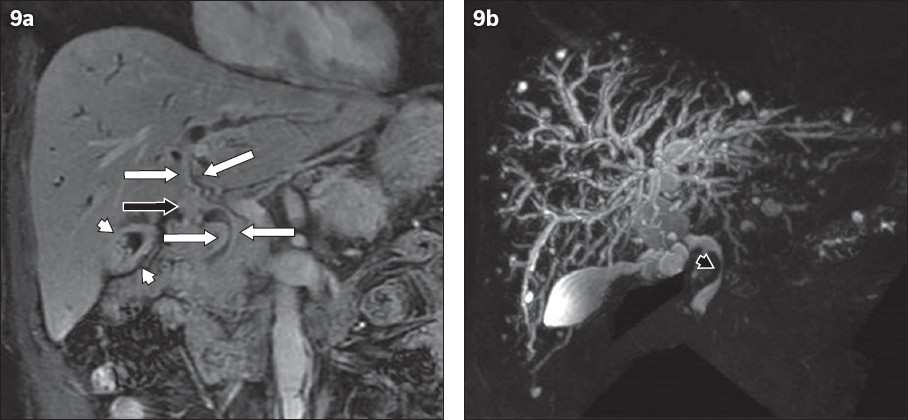
Fig. 9
IgG4-related sclerosing cholangitis in an asymptomatic 72-year-old man with elevated serum liver enzymes. (a) Contrast-enhanced coronal MR image shows circumferential symmetric wall thickening of the intrahepatic and extrahepatic bile ducts (white arrows). Mass-like thickening of the hilar ducts is also observed (black arrow). The gallbladder shows diffuse wall thickening with homogeneous delayed enhancement that indicates its involvement (white arrowheads). (b) MR cholangiopancreatography reveals multifocal narrowing and diffuse dilatation of the intrahepatic bile ducts. The involved extrahepatic bile duct shows luminal narrowing; however, the lumen is visible (black arrowhead).
LIVER
Hepatic involvement in IgG4-RD is rare. There are two types of hepatic involvement: IgG4-related autoimmune hepatitis and inflammatory pseudotumour.(8,12) The symptoms are non-specific and include fever, abdominal pain and general malaise, or patients may be asymptomatic.(8) IgG4-related inflammatory pseudotumour demonstrates variable enhancement patterns, including delayed homogenous enhancement or peripheral enhancement (
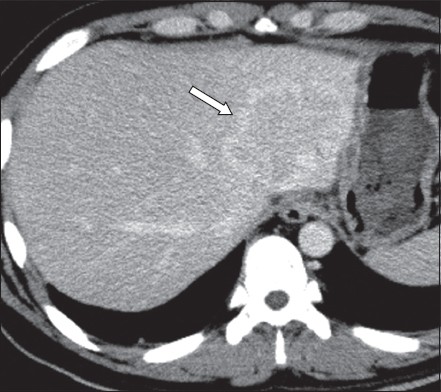
Fig. 10
IgG4-related inflammatory pseudotumor of the liver in a 25-year-old man who presented with fever, general malaise and appetite loss (same case as
KIDNEY
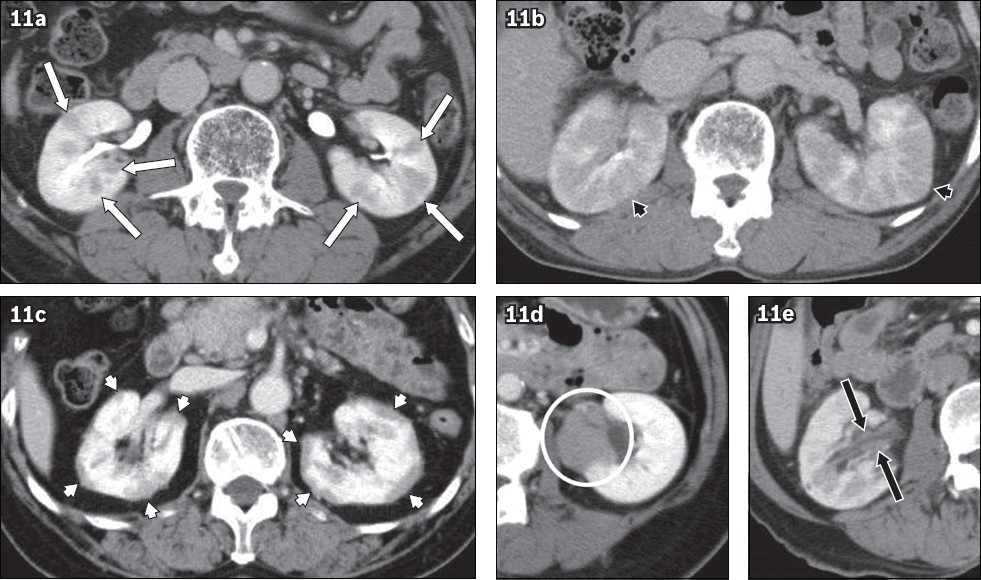
IgG4-related renal disease is found in approximately one third of patients with AIP and can present as acute or chronic renal failure.(6,12) Five imaging patterns have been described: bilateral round or wedge-shaped lesions (
Fig. 11
Five imaging patterns of IgG4-related renal disease in. (a) an asymptomatic 63-year-old man; (b) the same patient four months after the first imaging was performed; (c) an asymptomatic 68-year-old woman with elevated serum liver enzymes; (d) a 50-year-old woman with visual impairment (same case as Figs.
RETROPERITONEAL FIBROSIS
Approximately 20% of patients with AIP have retroperitoneal fibrosis, and more than two-thirds of cases of retroperitoneal fibrosis with unknown cause are thought to be related to IgG4-RD.(6,8,12) Patients may be asymptomatic or may present with back or abdominal pain.(8) On imaging, IgG4-related retroperitoneal fibrosis may manifest as a periureteral mass that entraps the ureters, leading to hydronephrosis and hydroureter (
Fig. 12
IgG4-related retroperitoneal fibrosis in a 25-year-old man who presented with fever, general malaise and appetite loss (same case as Figs.
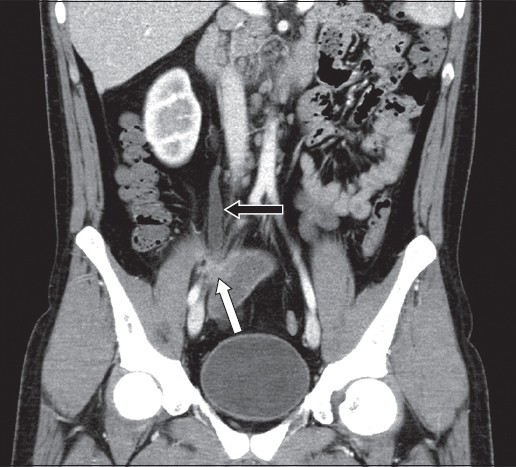
Fig. 13
IgG4-related periaortitis in a 73-year-old man with lower right abdominal pain. Delayed phase CT image shows a soft tissue mass around the abdominal aorta (arrows), demonstrating homogeneous delayed enhancement.

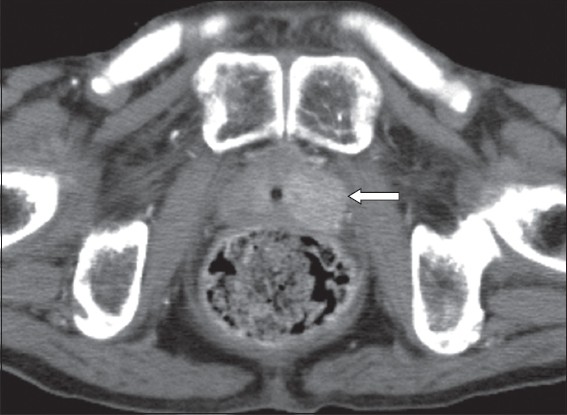
PROSTATE
IgG4-related prostatitis is rare and is associated with approximately 8% of AIP cases.(12) Patients may be asymptomatic or may present with lower urinary tract symptoms such as benign prostatic hypertrophy.(12) On imaging, IgG4-related prostatitis can show diffuse enlargement or focal lesions of the prostate (
Fig. 14
IgG4-related prostatitis in an asymptomatic 69-year-old man with a history of IgG4-related disease. Contrast-enhanced CT image shows a homogeneous enhanced mass in the left lobe of the prostate (arrow). This lesion decreased in size after corticosteroid therapy (not shown).
GASTROINTESTINAL TRACT AND MESENTERY
Gastrointestinal tract lesions in IgG4-RD have been reported sporadically in the stomach and duodenum, and small bowel lesions are extremely rare.(15) The lesions can cause wall thickening and ulcer formation; therefore, they often mimic malignancy (
Fig. 15
(a) IgG4-related enteritis in an 84-year-old man with abdominal pain. (a) Contrast-enhanced CT image shows wall thickening of the ileum with surrounding fat stranding (white arrows). The proximal small bowel is dilated owing to stenosis of the lesion (black arrows). (b) IgG4-related sclerosing mesenteritis in an asymptomatic 75-year-old man with a history of IgG4-related disease. Contrast-enhanced CT image shows fat stranding around the superior mesenteric artery and vein with a rim-like soft tissue mass (white arrowheads). This lesion decreased in size after corticosteroid therapy (not shown). A soft tissue mass around the abdominal aorta that represents IgG4-related periaortitis is also observed (black arrowhead).
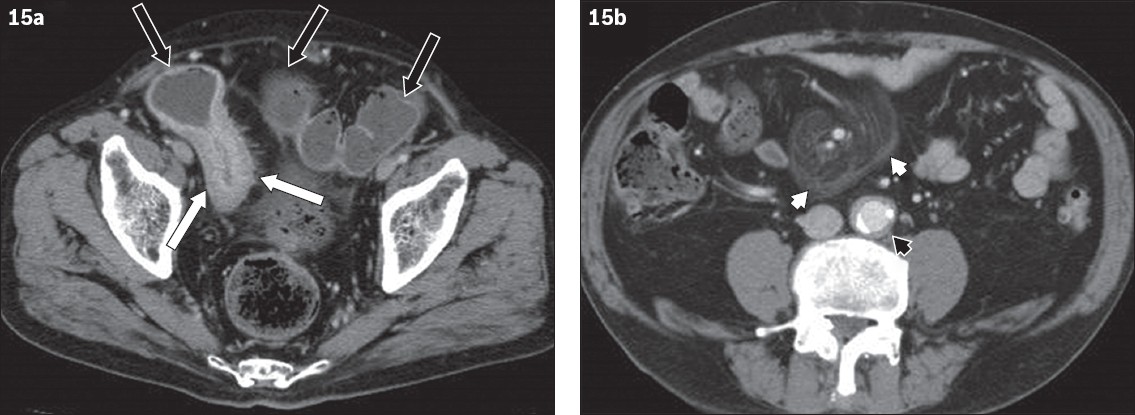
IgG4-related sclerosing mesenteritis is a rare entity characterised by focal or diffuse fibrosis and inflammation in the small bowel mesentery that can appear as a soft tissue mass. On imaging, it appears as a soft tissue mass enveloping the mesenteric vessels (
LYMPH NODES
Lymphadenopathy is often observed in patients with IgG4-RD. IgG4-related lymphadenopathy is common in the porta hepatis, cervical, mediastinal (
CONCLUSION
IgG4-RD is sometimes challenging to differentiate from other inflammatory or neoplastic diseases. However, characteristic imaging features can aid in the diagnosis of IgG4-RD. Moreover, multiorgan involvement can be a helpful clue to the possibility of IgG4-RD, especially in cases in which the multitude of findings initially seem unrelated. Radiologists should be familiar with the imaging presentations of IgG4-RD to avoid delayed diagnosis and unnecessary invasive interventions. This article illustrates the many characteristic CT and MR imaging findings of IgG4-RD across the whole body and is a useful compilation to aid in the diagnosis of IgG4-RD.
Supplementary Material
SMJ-62-581.pdf


