INTRODUCTION
In recent years, substantial research efforts have focused on reducing the global burden of mental illness. However, translation of research into real-world clinical services has lagged behind.(1) Large gaps in the provision of mental health services persist, even in developed countries.(2-4) Although there has been a burgeoning focus on improving mental health services in Singapore,(5) recent studies have demonstrated a significant treatment gap for mental disorders.(6-8)
There is a high prevalence of mental disorders in Singapore.(9,10) However, the 2010 Singapore Mental Health Study found that only 31.7% of individuals with mental disorders had ever sought help, and only 8.4% of those were managed by primary care physicians (PCPs).(8) Many mental disorders can be effectively managed in primary care settings,(11) and the integration of mental health services in community settings has been shown to improve patient outcomes.(12) Community mental health services have well-documented advantages, including better accessibility and acceptability of care, and reduced stigma and social discrimination.(13-15) Therefore, a key thrust of the Community Mental Health Masterplan of 2012 was to strengthen primary care to deliver accessible mental health services in the community.(16) Nevertheless, the follow-up Singapore Mental Health Study in 2016 found that the treatment gap for mental disorders remained high at 78.6%.(7) A local study found that PCPs in Singapore tend to shy away from managing mental conditions because of inadequate support and perceived lack of training.(17) These findings underscore the pressing need to continually enhance primary care mental health services and develop real-world interventions to bridge the treatment gap in Singapore.
Integrated care programmes have been developed in many countries worldwide to support the significant demand for mental health services in primary care settings.(18) In these programmes, patients who are within the patient base of primary care service networks receive integrated mental healthcare with input from specialist mental health professionals within the community. PCPs remain the primary treating physicians and work in close collaboration with specialist mental health professionals to support the mental health needs of their patients.
To enhance the integration of mental health in primary care in Singapore, Changi General Hospital launched the Health Wellness Programme (HWP), a pilot integrated care programme, in 2013. The HWP is a restructured hospital-led, integrated community mental health programme comprising psychiatrists and therapists (clinical psychologists and counsellors). It provides community-based specialised psychotherapy services to patients with mild to moderate mental health conditions who are managed by PCPs in the eastern region of Singapore. The HWP employs a shared care model that is characterised by close collaboration between members of the team and PCPs. The PCPs receive specialist psychiatric liaison support for patients whom they refer to the programme for psychotherapy. The therapists in the HWP, in discussion with psychiatrists at weekly case conferences, provide regular feedback to the referring PCPs regarding the progress of patients in therapy. PCPs may, in turn, flag patients who are unstable or unresponsive to first-line treatments to attend consultations with the programme’s psychiatrists. These patients may be given an early appointment to see a psychiatrist at the specialist outpatient clinic in Changi General Hospital for timely escalation of care.
This stepped care model provides patients in primary care with timely access to specialised psychotherapy interventions within the community, allowing for more effective integration of mental health services within primary care. By empowering and supporting PCPs in managing mental health conditions in the community, our integrated care programme helps to address two key barriers and challenges to mental healthcare in Singapore, namely the stigma associated with seeking tertiary psychiatric treatment and suboptimal accessibility (in terms of cost, scheduling and transport) of mental health services.(7)
The primary aim of this study was to examine the impact of the HWP on mental health-related patient-reported outcomes (PROs) for patients enrolled within the programme. The secondary aim was to describe the demographic and clinical profiles of the study participants.
METHODS
This prospective study involved patients who were referred by PCPs to the HWP for psychotherapy and were successfully enrolled in the programme from August 2013 to March 2015. Written informed consent was obtained from all patients. Patients who were included were (a) aged ≥ 21 years; (b) able to provide informed consent; and (c) had a mild to moderate mental health condition, as defined by a Global Assessment of Functioning (GAF) score of 51–90. Patients with an unstable mental state, delirium or dementia; psychiatric emergencies; suicidal, violent or aggressive behaviours; illicit drug use; personality disorders; and those with a GAF score ≤ 50 were excluded, as they would be more appropriately managed in specialist settings. This study was exempted from review by the institutional review board, as it was designed to examine the impact of a healthcare service programme.
The participating PCPs referred patients under their care for mental health diagnoses if they met the inclusion criteria of the programme. Thereafter, HWP therapists performed intake assessments to determine the patients’ suitability for enrolment into the programme. Subsequently, accepted participants underwent psychotherapy sessions, as indicated. The therapists had the flexibility to choose suitable psychotherapy approaches in collaboration with the patients. The number of treatment sessions was decided based on the therapists’ judgement of the patients’ clinical needs and agreed goals of treatment. Examples of psychotherapy approaches employed were supportive therapy, psychoeducation, problem-solving therapy, cognitive behavioural therapy, and acceptance and commitment therapy.
Throughout the enrolment process, therapists monitored the progress of the participants and liaised with the referring PCPs in a collaborative approach. Psychiatrists provided management recommendations at weekly case conferences with the therapists. The PCPs could also contact the psychiatrists to discuss cases when required, and escalate cases of patients who were more severely unwell to the specialist clinic at Changi General Hospital, Singapore, within seven working days.
Baseline GAF scores and clinical and demographic data were collected by the therapists during intake assessments. The mental health issues of the patients were categorised according to the records of the referring PCPs. Baseline measures were obtained on three patient-reported outcome measures: the EQ-visual analogue scale (EQ-VAS) of the EQ-5D-3L, Patient Health Questionnaire-9 (PHQ-9) and Sheehan Disability Scale (SDS). The EQ-5D-3L is the three-level version of the EQ-5D, a family of instruments measuring self-ratings of general health, and consists of two sections: the EQ-5D three-level descriptive system and the EQ-VAS. Only the EQ-VAS was used in the present study. The EQ-VAS records the respondent’s self-rated generic health status, with an endpoint score of 100 indicating the best health an individual can imagine and 0 indicating the worst.(19) The PHQ-9 is a nine-question instrument used to screen for the presence and severity of depression in the primary care setting. It measures depressive symptoms by scoring each of the nine DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) criteria for depression on a scale of 0 (not at all) to 3 (nearly every day).(20) The SDS is a self-report tool for assessment of functional impairment. This single-dimensional measure of global functional impairment ranges from 0 (unimpaired) to 30 (highly impaired).(21)
HWP therapists re-administered these three outcome measures to patients every five sessions and at the completion of therapy. Scores at the initial assessment session were considered as pre-intervention scores, and scores from the most recent re-administration before the end of the study period were considered as post-intervention scores.
Descriptive statistical analysis was performed for the demographic and clinical data of all study participants. Continuous variables were presented as mean ± standard deviation, and categorical variables were presented as frequency and percentage. EQ-VAS, PHQ-9 and SDS scores were compared before and after the intervention using paired t-tests. Improvements in mean scores and 95% confidence intervals were presented. Statistical significance was set at p < 0.05. Statistical analysis was performed using SAS software version 9.4 for Windows (SAS Institute Inc, Cary, NC, USA).
RESULTS
A total of 232 patients were referred to the programme and assessed. 229 patients were deemed suitable for enrolment, and 228 of them consented to participate in the programme and data collection.
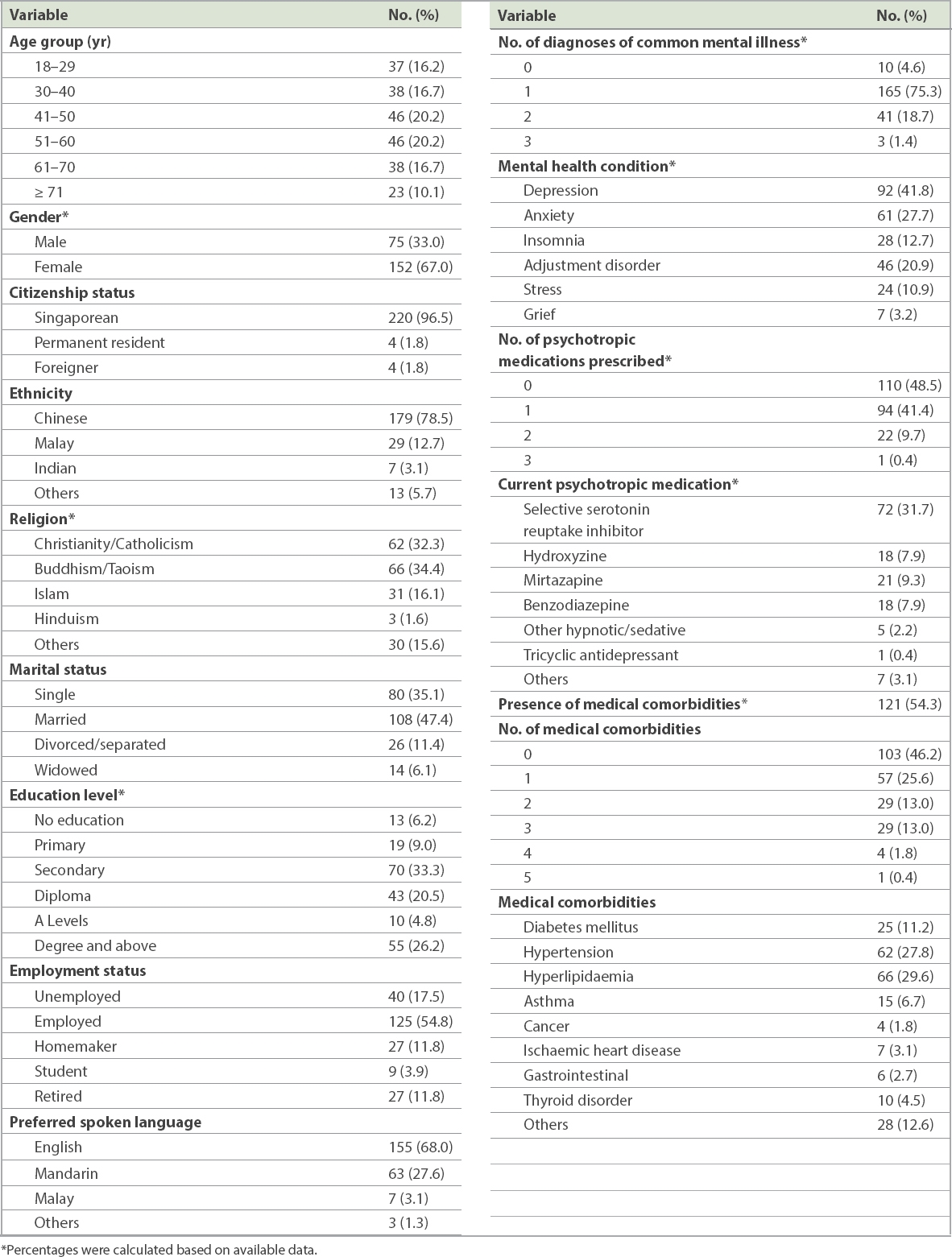
The demographic features of the participants, including age group, gender and clinical characteristics such as number of diagnoses of common mental health conditions, are summarised in
Table I
Demographic and clinical characteristics of study participants (n = 228).
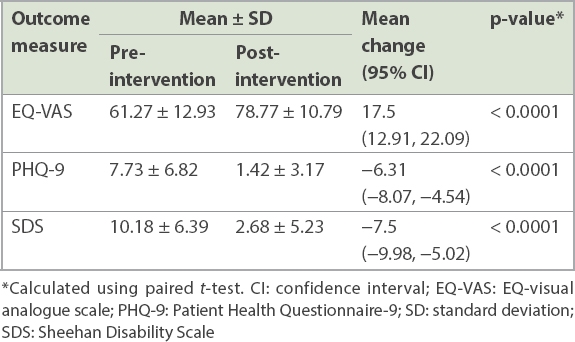
All three PROs (EQ-VAS, PHQ-9, SDS) showed significant improvement after intervention, as shown in
Table II
Changes in patient-reported outcomes after intervention.
DISCUSSION
To the best of our knowledge, the present study is the first to examine the impact of an integrated community mental health programme on mental health-related PROs for patients with mild to moderate mental health conditions managed in the primary care setting in Singapore. Our findings suggest that the HWP, a pilot integrated primary care mental health programme, is a feasible intervention that improved mental health-related PROs of patients with mild to moderate mental health conditions managed by PCPs. While the results of the present pilot study are preliminary, they bear important implications for the future planning of community mental health services in Singapore.
It has been well established that the traditional hospital-centric model of specialist care is insufficient to overcome barriers to care, especially for patients with longer-term disabilities.(22-24) Over the past two decades, several models of a collaborative approach between mental health and primary care providers, commonly termed as integrated care, have been proposed and implemented.(25) Previous studies have demonstrated that integration of mental health services in primary care brings about significant clinical and functional improvements for patients with mental disorders.(25-27) To date, community mental health programmes in Singapore have focused on supporting deinstitutionalisation and step-down care from the hospital to the community, neglecting the treatment of mental health conditions by PCPs in the community from initial detection.(28,29)
Our integrated care programme bridges the aforementioned gaps by providing access to timely and affordable specialised psychotherapy services in the community. Patients who are accepted into our programme bypass the need to be referred by their PCP to a psychiatrist in a restructured hospital or a private psychotherapist to access specialised psychotherapy services. This circumvents important barriers to help-seeking for mental disorders, such as stigma in seeing a psychiatrist, scheduling difficulties and cost. Furthermore, the collaborative consultation-liaison approach of our programme supports the right-siting of care of mild to moderate mental health conditions in the community from the initial diagnosis, through supporting PCPs with specialist consultation, as required, and timely escalation to specialist care for severely ill patients. These features of our programme may have contributed to the improvements in our patients’ PROs.
The clinical characteristics of our sample broadly mirror data from the 2010 Singapore Mental Health Study, which showed that 50.6% of participants had a comorbid medical illness.(30) In our sample, 54.3% of the participants had a comorbid medical illness. In Singapore, the majority of patients with chronic medical illnesses are followed up in primary care. As such, our integrated care programme may help to fill an important service gap for patients with comorbid physical and mental illnesses by bringing specialised mental healthcare to the primary care setting to support PCPs in their management efforts.
SSRIs are recommended as the first-line treatment for patients with moderate to severe depressive and anxiety disorders. The prevalence of SSRI use was 31.7% in our study sample. This suggests that the PCPs participating in our programme were confident in initiating evidence-based pharmacotherapy for depressive and anxiety disorders, which affected two-thirds of our participants. Consultation-liaison support provided by psychiatrists for patients enrolled in our programme and access to community-based specialised psychotherapy services to complement pharmacotherapy may account for the sizeable proportion of patients who were prescribed SSRIs by our partner PCPs. While our sample may not be representative of primary care practice in entire Singapore, the improvements in PROs suggest that this model of care could be feasible for wider implementation.
An important limitation of the present study is the lack of a control group. This means that we could not draw definitive conclusions about the impact of the HWP on mental health PROs in primary care. As this was a programme evaluation health service research study, we also could not determine which specific interventions in our programme contributed to the improvement in PROs. The improvements in EQ-VAS, PHQ-9 and SDS scores could be attributed to co-intervention with psychotropic medications. Future studies employing more sophisticated methodology such as waitlist control or cluster randomisation would generate a higher level of evidence. Another limitation of our study is the relatively short follow-up period, making it unclear whether the positive impact of the HWP is sustainable in the longer term. Nevertheless, our pilot data and results provide preliminary evidence that larger studies with a longer follow-up period can build on. Another limitation of our study is that it did not measure outcomes at the health system level, such as healthcare costs. Integrated care programmes are intrinsically resource intense and should demonstrate cost effectiveness before they are implemented on a large scale. They should lead not only to better clinical outcomes but also health system-level and society-level benefits such as reduced overall healthcare costs.(31) Future research can track patient movement between primary and tertiary care over a period to examine whether the implementation of the HWP is associated with lower healthcare costs.
Future research should also include external validation of similar integrated care programmes in another healthcare cluster at a larger scale. Although our study, along with many other studies, employed protocolised interventions that intend to facilitate the replication or adaptation of similar programmes in other healthcare clusters,(32-36) exact implementation strategies and outcomes in another healthcare cluster will likely depend on the clinical profiles of the local patients, capacity of the healthcare professionals, organisational setup and policy support. Health service research studies employing qualitative and mixed methods approaches are required to determine whether a similar integrated care programme can be adopted in another local healthcare cluster.(37)
In conclusion, the results of this pilot study provide preliminary evidence that the HWP, an integrated primary care mental health service, improved PROs for patients with mild to moderate mental health conditions who were managed by PCPs in Singapore.


