Abstract
INTRODUCTION
A pseudoaneurysm (or false aneurysm) is a haematoma that communicates with an artery through a disruption in the arterial wall. The femoral artery is the most common injection site among drug users, and infected femoral pseudoaneurysms are the most common vascular complications.
METHODS
A retrospective review of medical records of intravenous drug abusers (IVDAs) who presented with infected femoral pseudoaneurysms from January 2006 to December 2016 was carried out. Patients who had pseudoaneurysms due to other aetiologies or trauma were excluded.
RESULTS
A total of 27 patients with infected femoral pseudoaneurysms were identified. The majority were male (92.6%) and of Malay ethnicity (55.6%). Median age was 50 (range 31–62) years. Commonly abused drugs were buprenorphine (or Subutex; 59.3%) and midazolam (or Dormicum; 51.9%). Groin pain and swelling (100.0%), fever (66.7%) and presence of a pulsatile mass (51.9%) were the most common presenting symptoms. Diagnosis was confirmed via computed tomography angiography in all patients. 25 patients underwent upfront arterial ligation with debridement, among whom three patients required concurrent surgical revascularisation. Only two patients underwent ultrasonography-guided thrombin injection – one eventually required surgery and the other was lost to follow-up. Postoperative complications included wound infection (42.3%), bleeding (11.5%) and necrotising fasciitis eventually resulting in limb loss (3.8%). There were no associated mortalities.
CONCLUSION
Infected pseudoaneurysms in IVDAs pose a unique challenge to vascular surgeons. We found that simple ligation and debridement was a safe and effective option for such patients.
INTRODUCTION
A pseudoaneurysm (also known as false aneurysm) is a haematoma that communicates with an artery through a disruption in the arterial wall. Its outer wall usually lacks a true epithelial lining and is made up of a layer of compressed surrounding tissue.
Complications arising as a result of intravenous drug abuse have traditionally posed a unique challenge to vascular surgeons. Due to its easy accessibility, the femoral artery is the most commonly abused injection site for drug users.(1,2) Accordingly, infected femoral pseudoaneurysms are the most common vascular complications in this select group of patients. Other common causes of infected femoral pseudoaneurysms include iatrogenic complications secondary to percutaneous access procedures (e.g. cardiac catheterisation) and synthetic bypass graft infections. These patients can present with severe sepsis and/or haemodynamic instability due to septicaemia. If left untreated, femoral pseudoaneurysms can be rapidly fatal secondary to septicaemia and exsanguination.
Locally, there has been a brief increase in the number of intravenous drug abusers (IVDAs) since 2002. This spike coincided with the introduction of buprenorphine (also known as Subutex) into the local market. It had initially been introduced as an opiate substitute for heroin abusers to wean themselves off their dependency but was instead abused by many drug users due to its lower cost and relatively easy accessibility. Within the first four years of its introduction, there were at least 3,800 known Subutex abusers in Singapore.(3) Subutex abusers then accounted for the majority of IVDA patients locally. However, following a review by Singapore’s Ministry of Home Affairs and Ministry of Health in 2006, more stringent measures were imposed to curb the abuse of this drug, and the number of Subutex abusers has correspondingly dropped.(3)
This study aimed to evaluate a single institution’s experience with infected femoral pseudoaneurysms in IVDAs over a decade, with a particular focus on the range of presentations and management outcomes in this select group.
METHODS
A retrospective review was performed of all IVDA patients who presented with infected femoral pseudoaneurysms to our institution’s vascular unit from January 2006 to December 2016. Patients who had pseudoaneurysms due to other aetiologies, such as cardiac catheterisations or trauma, were excluded.
Basic demographic data and the type of drug abused, presenting signs/symptoms, investigations performed, clinical management (including operative details), postoperative complications and long-term outcomes to date were extracted from the patients’ electronic medical records and case notes.
Data was analysed using IBM SPSS Statistics for Windows version 20.0 (IBM Corp, Armonk, NY, USA). The study protocol was approved by our institutional review board.
RESULTS
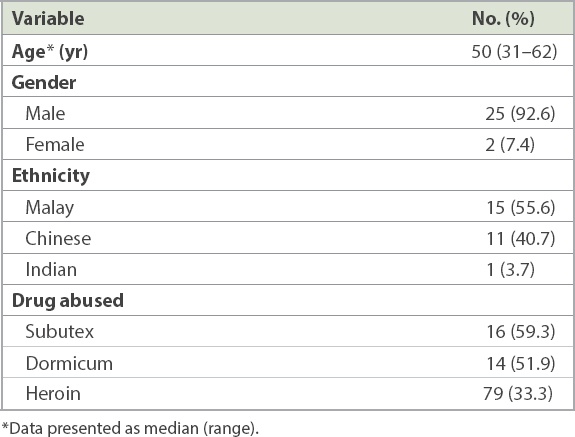
A total of 27 IVDA patients presented with infected femoral pseudoaneurysms during the study period. The majority were male (92.6%) and of Malay ethnicity (55.6%) (
Table I
Demographics and patient characteristics (n = 27).
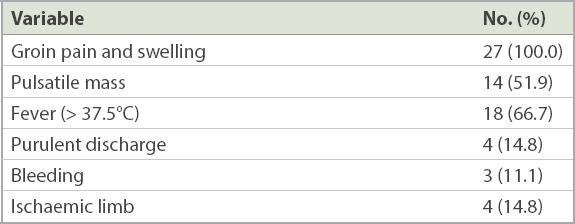
Groin pain and swelling (100.0%), fever (66.7%) and the presence of a pulsatile mass (51.9%) were the most common presenting symptoms (
Table II
Presenting signs and symptoms (n = 27).
Computed tomography (CT) angiography was performed for all patients to confirm the diagnosis and preoperative evaluation. The mean diameter of the pseudoaneurysms was 4.2 (range 1.1–10.0) cm.
Microbiological analysis via blood culture and intraoperative tissue culture predominantly grew Staphylococcus aureus (90.0%). Other organisms that were cultured included Pseudomonas aeruginosa, Streptococcus milleri and Klebsiella. All patients were empirically started on intravenous cloxacillin on admission, and this was subsequently modified according to culture sensitivities.
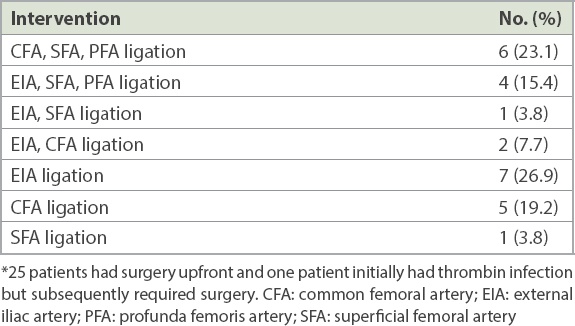
Among 27 patients, 25 underwent arterial ligation with debridement. Of these 25, three patients required concurrent surgical revascularisation – two required an external iliac to popliteal artery bypass and one required thrombectomy of the superficial femoral artery (
Table III
Surgical interventions (n = 26).*
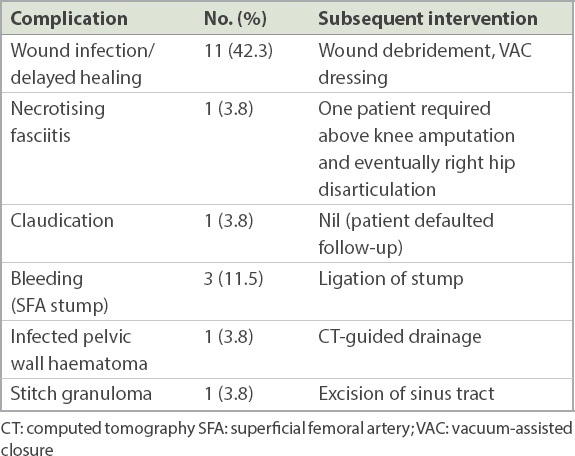
Postoperative complications included wound infection (42.3%), bleeding (11.5%) and necrotising fasciitis eventually resulting in limb loss (3.8%) (
Table IV
Postoperative complications in patients who needed surgery (n = 26).
DISCUSSION
The femoral artery is the most common site for an infected pseudoaneurysm in IVDAs due to its easily accessible location. Pseudoaneurysms occur in this group due to the inadvertent arterial injection of illicit drugs, resulting in periarterial extravasation and haematoma formation. Subsequent contamination of this haematoma can cause erosion and eventual rupture of the vessel wall, and pseudoaneurysm formation. If left untreated, potential sequelae include sepsis, haemorrhage, digital embolisation, limb loss and even death due to exsanguination or septicaemia.(4)
Groin pain and swelling in an IVDA should prompt a high index of suspicion for the presence of a pseudoaneurysm. It is of paramount importance to be able to clinically differentiate a femoral pseudoaneurysm from a groin abscess. Previous studies have shown that an erroneous diagnosis can lead to massive haemorrhage, especially if surgical drainage is attempted for a presumed groin abscess.(5) For this reason, thorough history-taking and physical examination are essential for any patient presenting with groin swelling, especially with previous history of intravenous drug abuse. It is pertinent to note that even though the patients are ill, not all will look toxic at presentation and with a classical pulsatile groin mass. This was demonstrated in our case series, where only 51.9% of patients presented with a pulsatile groin mass and only 66.7% of patients had fever on admission. When faced with an uncertain diagnosis, further investigation with appropriate imaging is warranted.
The two most commonly used investigations are CT angiography and duplex ultrasonography. Each has its own advantages and disadvantages. Duplex ultrasonography is the diagnostic modality of choice at many centres overseas.(6,7) Its advantages include the provision of a dynamic view, with the ability to visualise bidirectional blood flow in the aneurysmal sac, reliably distinguishing between a groin abscess and a pseudoaneurysm. It can also help screen for associated deep vein thrombosis. The main drawbacks of duplex ultrasonography are that it is often unable to detect the full extent of the aneurysm or visualise the inflow anatomy.
CT angiography, on the other hand, can allow precise definition of the pseudoaneurysm anatomy as well as that of its surroundings. It is important for the surgeon to be able to visualise the anatomy of the surrounding structures as well as the arterial supply to the distal limb, especially if more complex surgical reconstruction is planned. Additionally, CT imaging will allow the surgeon to identify any potential indwelling sharp objects in the surgical field, such as broken needle tips. Remnant foreign objects left in situ could not only be a nidus for recurrent infection but also pose a risk for healthcare workers performing a change of wound dressings for these patients. The main drawback of CT angiography is the risk of contrast-induced nephropathy in patients with pre-existing renal impairment. CT angiography was the imaging modality of choice in our series for both logistic and technical reasons – it was readily available at our institution at all hours of the day and a preoperative definition of the vascular anatomy was preferred by the vascular surgeons on call.
Once the diagnosis of an infected femoral pseudoaneurysm has been established, antibiotic coverage should immediately be commenced. Barring any contraindications, the empirical antibiotic of choice at our institution is intravenous cloxacillin. This would be appropriate for a majority of patients in our local setting, as 90.0% of patients in our series grew methicillin-sensitive Staphylococcus aureus from their microbiological cultures. This finding was confirmed in other series,(8) although atypical organisms, such as Salmonella, have been also reported.(9)
Over the years, various treatment approaches have been suggested, with varying degrees of success. A non-surgical approach involves the injection of thrombin into the sac of the pseudoaneurysm to promote thrombosis. Surgical options include arterial ligation with wound debridement (without revascularisation), primary repair with local debridement, limb amputation, and arterial ligation and wound debridement (with immediate/delayed reconstruction). Although there are no published guidelines on the recommended management for this group of patients, most vascular units regard arterial ligation with wound debridement as the first-line surgical treatment.(10-12) The principles of surgery, for these patients, are adequate debridement of necrotic tissue, control of haemorrhage and preservation of distal circulation, when possible.
The main point of contention in recent years has been the role of surgical revascularisation after arterial ligation. Proponents for revascularisation have raised concerns regarding the incidence of severe claudication and disability in these patients. As mentioned previously, various revascularisation options have been described, including bypass with autologous conduit (e.g. superficial femoral vein),(13) extra-anatomical bypass with synthetic material (e.g. obturator bypass) (14) and arterial reconstruction with the internal iliac artery.(15) However, the risk of graft sepsis (eventually necessitating graft removal) is considerable, occurring in more than 80% of patients in one previous case series.(16) Arguments against immediate revascularisation include the lack of suitable superficial veins in these patients (due to chronic venous cannulation), the high risk of graft infection and anastamotic breakdown, and the possibility of recalcitrant addicts using the graft as a route of injection.
While arterial ligation without immediate revascularisation can potentially result in limb loss or disabling claudication, it should be remembered that the primary objective is to first save life before limb. Our series showed a limb loss rate of 3.8% (n = 1), which ultimately resulted from necrotising fasciitis rather than postoperative ischaemic limb. In our cohort of patients, these results suggest pre-existing, well-developed collaterals supplying their extremities, likely due to chronic arterial thrombosis from repeated injections. Based on the above results of our case series, revascularisation at the time of the initial operation is not recommended. Delayed revascularisation in patients with disabling claudication can be considered once the infection has settled and appropriate treatment for the patient’s drug addiction has been administered.
Ultrasonography-guided thrombin injection into the pseudoaneurysm sac has been proposed as a non-surgical alternative. However, it is more commonly used for small, non-infected pseudoaneurysms (i.e. occurring as a result of interventional procedures, such as cardiac catheterisation). An Irish study in 2009 included four IVDAs who received thrombin injections for their infected femoral pseudoaneurysms.(17) The patients in the study were thought to be suitable, as they presented early and had small-diameter pseudoaneurysm necks. However, the end result was 75% failure and eventual surgical intervention. This largely corroborates with the data in our case series, which showed a 100% treatment failure rate, as one patient who received thrombin injection required subsequent surgery, and the other patient absconded and was lost to follow-up. As such, thrombin injection should not be recommended as treatment for infected pseudoaneurysms in IVDAs.
A few studies have suggested endovascular treatment of mycotic pseudoaneurysms, where a stent-graft is initially used as a bridge to a definitive revascularisation procedure.(18-20) One such case report described a patient who remained well and symptom-free over a year following such a bridging procedure, and thus a bypass was not performed. He was treated with prolonged intravenous antibiotic therapy for four weeks after the stenting procedure.(18) Even though technically feasible, these novel methods are still not standard treatment for infected pseudoaneurysms. Such an endovascular approach may have potential for use in the emergency setting to stabilise patients until a time when they become suitable for a more definitive extra-anatomical bypass procedure.
In conclusion, infected pseudoaneurysms in IVDAs pose a unique challenge to vascular surgeons. In addition to the controversies regarding their optimal treatment, management of this group of patients is often complicated by compliance issues and recalcitrant drug use. We found that simple ligation and debridement without revascularisation was a safe and effective treatment for such patients. Interval revascularisation can be discussed with patients if postoperative recovery is complicated by disabling claudication or tissue loss secondary to ischaemia. Special attention should be directed during follow-up to rehabilitation from intravenous drug abuse.


