Dear Sir,
A previously healthy 52-year-old Sikh woman presented with painful calf swelling of two weeks’ duration. Palpation revealed tender indurated non-ulcerated nodules located bilaterally over the calves without lymphadenopathy. The patient had no fever, night sweats, weight loss or any preceding symptoms of an upper respiratory tract infection. She underwent a punch biopsy of a left calf nodule. Histology demonstrated non-specific changes of subcutaneous fat degeneration and fibrosis with a mild foam cell infiltrate. Evaluation for autoimmune and infective aetiologies was unremarkable. The patient was treated with a course of oral prednisolone for panniculitis of unclear aetiology but demonstrated only mild clinical improvement. In view of persistent disease and a lack of conclusive aetiology, a repeat punch biopsy of a separate nodule over the right calf was sought. Histology revealed mild lobular and septal inflammatory infiltrate; no acid-fast bacilli, granulomas or malignant cells were seen. She was continued on steroids and monitored clinically.
Six months later, the patient developed subacute onset of bilateral lower limb weakness and numbness. Neurological examination revealed signs consistent with a conus medullaris lesion. Magnetic resonance (MR) imaging of the whole spine demonstrated mild spinal cord expansion at the T12-L1 level with T2 hyperintensity and contrast enhancement. MR imaging of the brain showed two tiny enhancing lesions at the right frontal subcortical region. Cerebrospinal fluid analysis revealed lymphocytic pleocytosis, but infective markers, cytology and flow cytometry were negative. During the same period, the patient was noted to have mild thrombocytopenia, elevated serum lactate dehydrogenase (LDH) levels (1,957 U/L) and elevated β2-microglobulin levels (2,643 µg/L). A whole-body positron emission tomography/computed tomography did not reveal any systemic organ abnormality or lymphadenopathy. A bone marrow trephine was also performed and excluded malignant marrow infiltration.
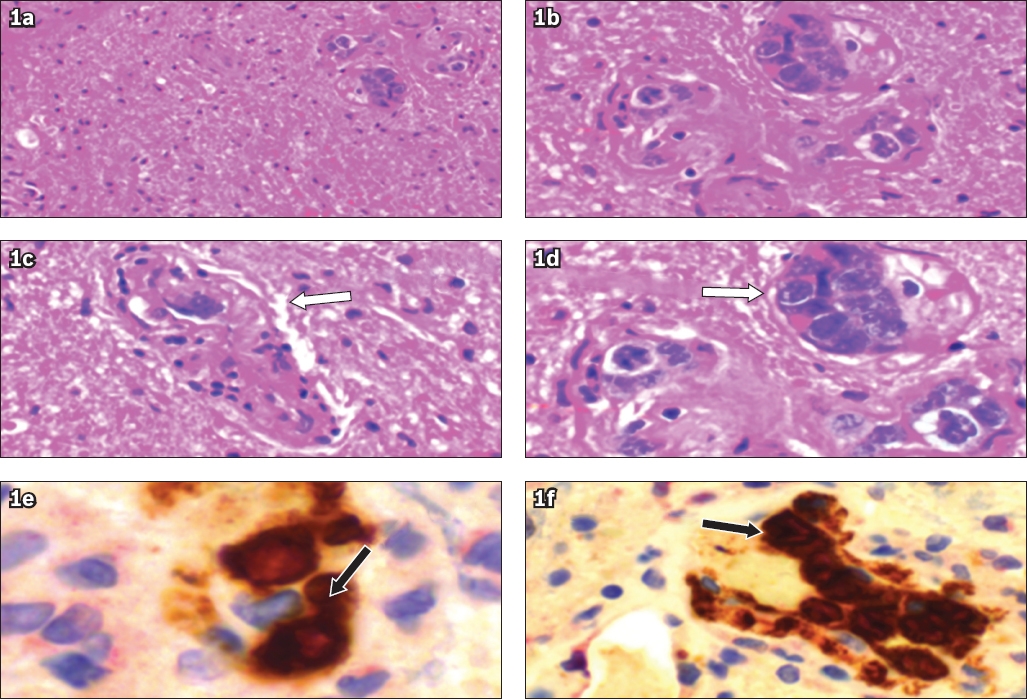
The patient eventually underwent a biopsy of the conus medullaris lesion. Histology showed spinal cord necrosis and focal segmental vessel occlusion by a few atypical lymphoid cells that stained doubly positive for CD79a and Ki-67 on immunohistochemistry (
Fig. 1
(a-f) Immunohistochemistry images of the conus biopsy specimen show focal segmental vessel occlusion (white arrows) by atypical lymphoid cells (black arrows) that stained strongly positive for CD79a and Ki-67.
Intravascular lymphoma (IVL) is a rare disease that frequently involves the skin.(1) Cutaneous manifestations can be remarkably protean, ranging from maculopapular eruptions to palpable purpura and ulcers.(1,2) There have been a few sporadic case reports of IVL presenting as panniculitis since 2000.(3,4) To aid in the diagnosis of IVL, repeat and even random skin biopsies of clinically uninvolved skin have been advocated, especially in the setting of pyrexia of unknown origin.(5) Other clinical manifestations include central nervous system involvement, haemophagocytic syndrome with hepatosplenomegaly, cytopenia and elevated LDH. The cutaneous variant of IVL, good ECOG (Eastern Cooperative Oncology Group) performance status, limited Stage 1 disease and early institution of combination chemotherapy are independently associated with improved survival,(1) highlighting the importance of early diagnosis of IVL. In our case, the patient initially presented with skin lesions, followed by myelopathy and thrombocytopenia more than six months later. Early diagnosis was unfortunately limited by non-specific cutaneous signs and histological features.
In summary, this case highlights the importance of a high index of suspicion for IVL among clinicians and pathologists in the aetiological diagnosis of panniculitis, especially when the location is atypical, the patient does not respond to conventional therapy, and in the presence of central nervous system and/or systemic involvement. Early diagnosis of IVL, particularly when it is limited to cutaneous involvement, coupled with timely institution of combination chemotherapy, can dramatically improve the overall prognosis of the condition.
Yours sincerely,


