Abstract
INTRODUCTION
Healthcare professionals (HCPs) working in critical care areas play an important role in the organ donation (OD) process. We studied HCPs’ own willingness to be organ donors and its association with sociodemographic factors as well as their knowledge and attitudes about OD and transplantation.
METHODS
A cross-sectional survey of HCPs working in four critical care units in a major transplant centre in Malaysia was undertaken using a validated structured questionnaire. Responses were analysed using multivariable analysis with willingness to donate as the dependent variable.
RESULTS
Of the 412 respondents (response rate 98.1%), the majority were nurses (60.4%), Malay (71.1%) and female (77.2%). Overall, 68.0% were willing to donate. The independent predictors of willingness to donate were profession (p < 0.001) and the Hindu religion (p = 0.001). Ethnicity (p = 0.003), religious belief (p < 0.001), knowledge (p = 0.016), belief in brain death (p = 0.018) and confidence in transplantation (p < 0.001) also independently correlated with willingness to donate, while attitudes to OD did not. Of those willing to donate, only 37.3% were carrying a donor card and only 63.1% had informed their family of their intention to donate.
CONCLUSION
Although willingness to donate was higher in critical care HCPs than HCPs in general, significant knowledge gaps as well as certain beliefs and perceptions that could pose a barrier to OD were identified in this group. Measures to improve OD rates in Malaysia should include targeted educational programmes for HCPs working in critical care areas.
INTRODUCTION
The concept of brain death (BD) was officially recognised in Malaysia by the Malaysian Medical Council in 1993 with the publication of the Consensus Statement on BD.(1) However, organ donation (OD) was sporadic until the first heart transplant in 1997, when interest in BD and deceased OD revived.(2) In an effort to improve OD rates, tissue organ procurement teams were established in hospitals throughout Malaysia.(2-4) Hospital staff specifically identified for this purpose included doctors (responsible for donor detection, diagnosis of BD, referral and consent), nurses (to reinforce the aforementioned functions and support the family) and other staff responsible for the transport of organs and speedy return of the donor’s remains to the next of kin.(3,4)
In spite of these efforts, Malaysia’s deceased OD rate in 2015 was only one per million population (pmp), among the lowest in the world, although there were 21,513 patients on the waiting list.(5,6) Developed countries such as Spain (40.15 pmp), the United States (28.21 pmp) and the United Kingdom (20.26 pmp) have achieved substantially better deceased OD rates.(7) Other Muslim countries such as Turkey and Iran have recorded deceased OD rates of 6.00 pmp and 10.21 pmp, respectively, while neighbouring countries such as Singapore and Thailand attained 3.93 pmp and 3.03 pmp, respectively.(7)
The low donation rate in Malaysia is concerning and has been highlighted in previous studies.(2,8,9) Malaysia’s multiracial and religious society consists of three major ethnicities, Malay (68.6%), Chinese (23.4%) and Indian (7.0%).(10) Awareness of deceased OD has been found to be low, with less than half (34.9%–44.3%) of the general population being reported to be willing to donate.(8,11,12) Lack of trust in the medical system, cultural-religious attitudes, a desire to be buried whole, and insufficient information on OD were common reasons cited for unwillingness to donate.(8) Loch et al and Wong reported a difference in acceptance of OD among different ethnic groups: Malays, who make up the largest proportion of the population, were less willing to donate.(8,11) Another study stated that only 34.8% of the Muslim population were willing to donate.(13) However, other researchers suggested that religious and cultural factors may not influence the decision to donate.(12,13) Instead, possible reasons were lack of access to information on OD and not being convinced of the benefits of OD.(12,13)
Another factor that could contribute to low OD rates is the failure of healthcare professionals (HCPs) to identify donors, obtain their consent and procure organs.(9) This has been the subject of several studies around the world.(14-21) An American study showed that HCPs’ attitudes played a major role in approaching families for donation and that their medical knowledge did not affect the OD process.(21) Studies in Spain and Nigeria have shown that the medical profession and knowledge of BD were strongly correlated with HCPs’ willingness to donate.(14,15,17) In the Islamic world, 90% of HCPs in Turkey were willing to donate their own organs and 83% of HCPs from Qatar supported OD.(18,20) Abidin et al and Rozaidi et al concluded that general HCPs in Malaysia had low levels of agreement to OD, as only 47.8% and 49.5% of them, respectively, were willing to donate their own organs, consistent with that of the general population.(2,9) HCPs’ acceptance and declaration of BD, passivity in approaching family, and cultural and religious differences may affect the OD process.(9)
A review of 45 studies published by Walters in 2009 showed that the responsibility for OD may be best placed within the domain of specialist personnel working in critical care areas.(22) These professionals are directly involved in recognising and diagnosing BD; they establish a relationship with the family early on and may advocate OD once the diagnosis of BD has been confirmed.(23) They are also responsible for contacting transplant coordinators and initiating the OD process.(9,23,24) These HCPs also play a vital role in nursing the potential multiorgan donor.(24) In Malaysia, the OD process has been outlined by the National Transplant Resource Centre.(25) HCPs working in this domain must therefore have adequate experience, knowledge, skills and positive attitudes, as they have the ability to influence OD rates. Longer waiting lists and low OD rates may be a reflection of their reticence, leading to lack of transplantable organs.
Local and worldwide studies showed that HCPs were more likely to request donations from families if they were personally willing to donate.(9,21) This is especially relevant for HCPs working in critical care areas, as they are directly involved in the OD process. In a large-scale international study surveying such professionals from 11 developed countries, an average of 79.3% were willing to donate their own organs.(26) Willingness to donate in this group of professionals has not been studied in the Malaysian context and hence merits scrutiny. We hypothesised that the knowledge and attitudes of HCPs working in critical care areas would correlate positively with the HCPs’ personal willingness to donate organs. We also believed that religion and religious beliefs may correlate with their willingness to donate.
This study examined the association between HCPs’ knowledge of BD, OD and organ transplantation and their willingness to donate. In addition, we examined associations among specific attitudes towards BD and OD, confidence in transplantation and religious beliefs, and the HCPs’ willingness to donate.
METHODS
A cross-sectional survey was carried out in July 2015 in Hospital Kuala Lumpur, a major transplant centre in Kuala Lumpur, Malaysia. The study population consisted of doctors and nurses (medical officers, specialists, consultants, registered nurses, sisters and matrons) working in the following critical care areas: General Medical Intensive Care Unit (ICU); Neurosurgery ICU; Neurology; and Emergency and Trauma. The target population size was 565, which was the total number of HCPs working in the above areas. The study was conducted and reported according to recommendations from the STROBE (Strengthening the Reporting of Observational Studies) Statement.(27) It was registered under the National Medical Research Register (NMRR) with ID number NMRR-14-1790-23450 S5 R0. Ethical approval was given by Malaysia’s Medical Research and Ethics Committee and the Perdana University Internal Review Board (PUIRB-HR0090).
A questionnaire was constructed based on existing literature and clinical experience.(1,18,28-32) It contained 51 items and included ten demographic features, 25 knowledge questions and 16 attitude questions. Collected sociodemographic data included profession, position, gender, age, religion and ethnicity. The questionnaire was divided into two sections, the first on BD and the second on OD and transplantation. Each knowledge and attitude question was assessed using a five-point Likert scale with the responses ‘Definitely not’, ‘Probably not’, ‘Unsure’, ‘Probably yes’ and ‘Definitely yes’. The sum of the overall knowledge scores was calculated out of 25 questions: the maximum total OD and transplantation knowledge score was 10, while the total BD knowledge score was 15. Five questions specifically concerned knowledge on BD tests. Respondents’ attitudes were grouped according to theme: religious attitudes, attitudes towards BD, confidence towards transplantation and attitudes towards OD.
We assessed the questionnaire qualitatively by face and content validation. For this, ten experts in the fields of medicine, surgery, psychology and transplantation examined early versions of the questionnaire. The final version incorporated the experts’ comments. The questionnaire, participant information sheet (PIS) and consent form were constructed in English and translated into Malay. An independent back translation was performed to check for validity. An option of either language was offered to our study population.
Participants from the above critical care areas were verbally briefed and handed a copy of the PIS. After obtaining written consent, the questionnaire was distributed to the respondents individually. Completed questionnaires were separated from the PIS and consent forms so that anonymity was maintained. Responses were coded into IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA) for statistical analysis.
Data was analysed using IBM SPSS Statistics and Stata version 14 (StataCorp, College Station, TX, USA). Questionnaires that were less than 80% complete were excluded entirely to avoid any analysis being unjustly skewed. For questionnaires that were more than 80% complete, only missing data for particular items were excluded. These exclusion criteria were determined during the study design phase to eliminate the possibility of post-entry exclusion bias. For knowledge questions, the Likert scale responses were collapsed into a right or wrong answer, with every right answer being given a score of 1. Questions pertaining to attitudes were analysed quantitatively. ‘Definitely yes’ and ‘Probably yes’ were grouped together as ‘Yes’, while ‘Unsure’, ‘Definitely not’ and ‘Probably not’ were grouped as ‘No/unsure’, as the absolute numbers for some Likert scale responses were too few to allow for appropriate statistical analysis. ‘Unsure’ was taken as a negative response for all questions, because being unsure showed a tendency to support a negative attitude as compared to a positive one.
Descriptive statistics including percentage, mean and standard deviation were used to summarise the variables, as appropriate. Demographics and attitudes were cross-tabulated with willingness to donate as the dependent variable, and Pearson’s chi-square test was used to examine for statistical significance. Univariable logistic regression analysis was used to identify associations between demographics, knowledge scores and attitudes, with willingness to donate as the dependent variable. Multivariable logistic regression analysis was also used to adjust the odds for each significant independent variable. Kendall’s tau-b correlation coefficient and Spearman’s rank correlation coefficient were used to check for correlation prior to input into the model. Results of the univariable and multivariable analyses were displayed as odds ratios and 95% confidence intervals (CI). For categorical variables, the odds ratios were relative to the reference population. Statistical tests used were two-tailed and p-values < 0.05 were considered significant.
RESULTS
Of the 565 HCPs employed in the critical care areas listed, 420 were available for the study. However, seven declined to participate. Data from another respondent was excluded due to non-completion of over 80% of the questionnaire, leaving a total of 412 respondents. Missing data was less than 6% for all variables. The contacted population response rate was 98.1%, while the total eligible population response rate was 72.9%. The mean age of the respondents was 29.37 ± 6.08 years. The majority were nurses (60.4%), female (77.2%) and Malay (71.1%).
Table I
Association of sociodemographic data with willingness to donate (n = 412).
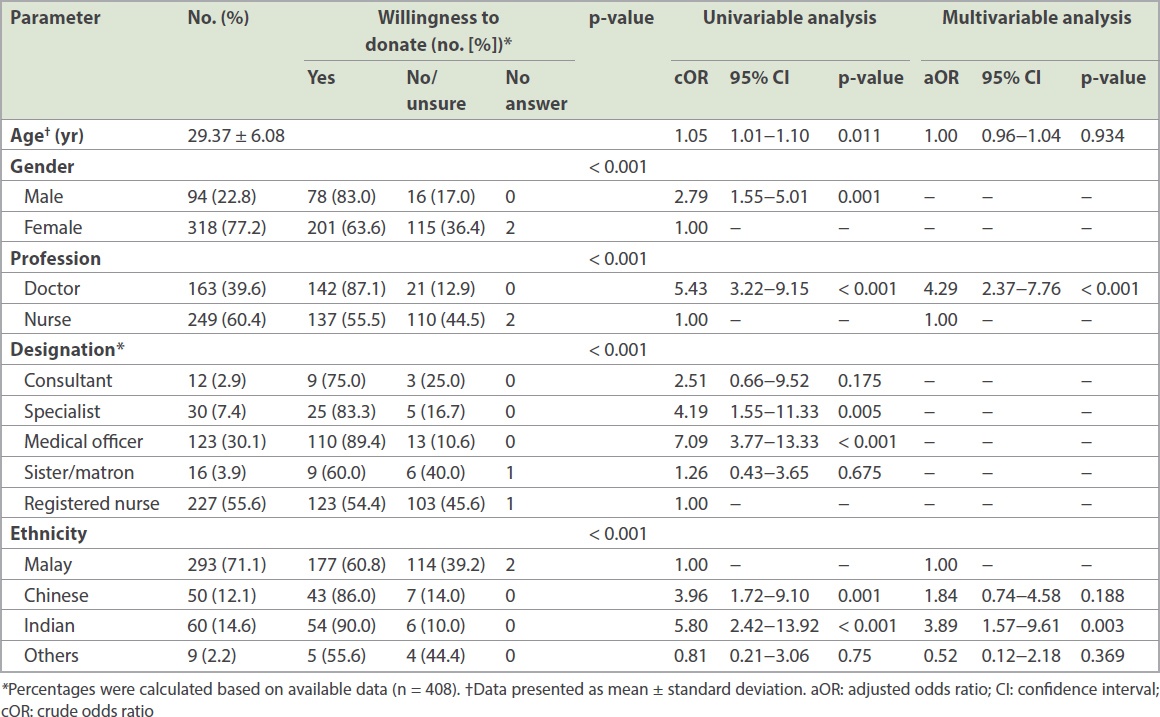
Table II
Association of religion and religious belief with willingness to donate (n = 412).
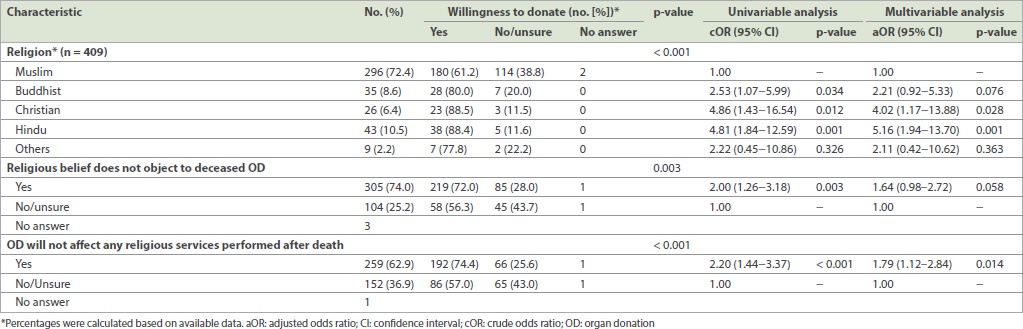
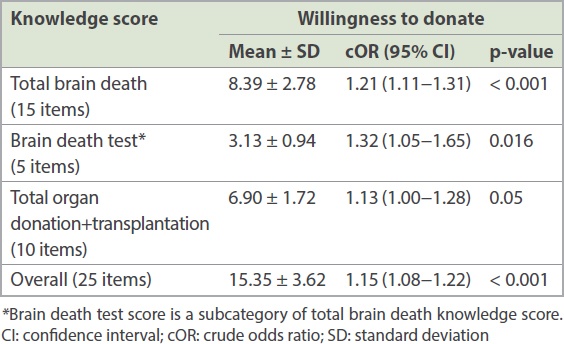
Table III
Association of knowledge with willingness to donate.
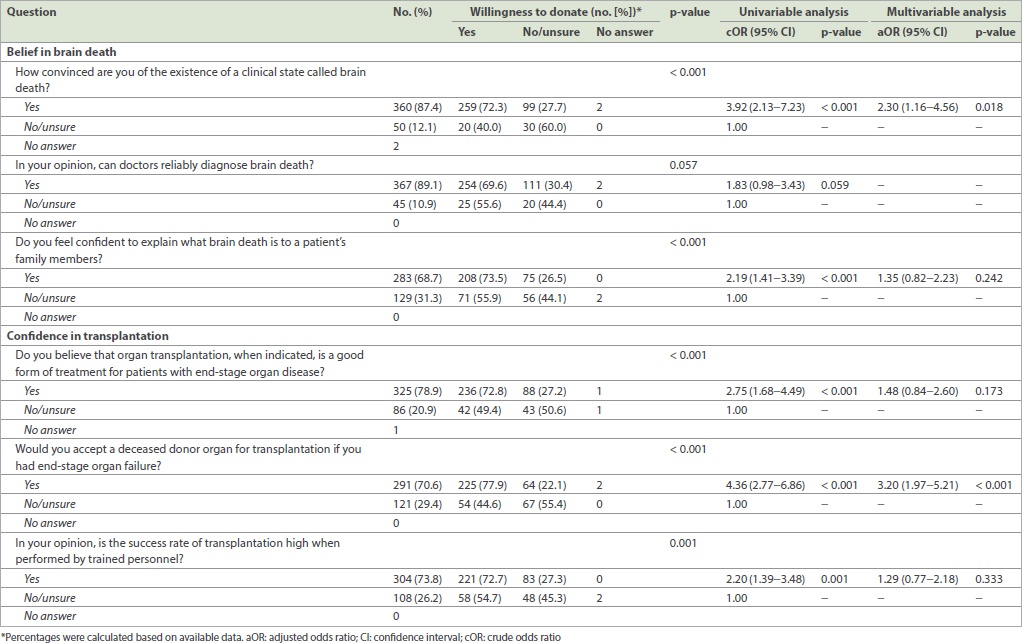
The odds of HCPs’ willingness to donate increased to 3.92 (95% CI 2.13–7.23, p < 0.001) when they were convinced of the existence of BD, by 1.83 (95% CI 0.98–3.43, p = 0.059) when they believed that doctors could reliably diagnose BD, and by 2.19 (95% CI 1.41–3.39, p < 0.001) when they felt confident to explain BD to a patient’s family member (
Table IV
Association of attitudes towards brain death and organ transplantation with willingness to donate.
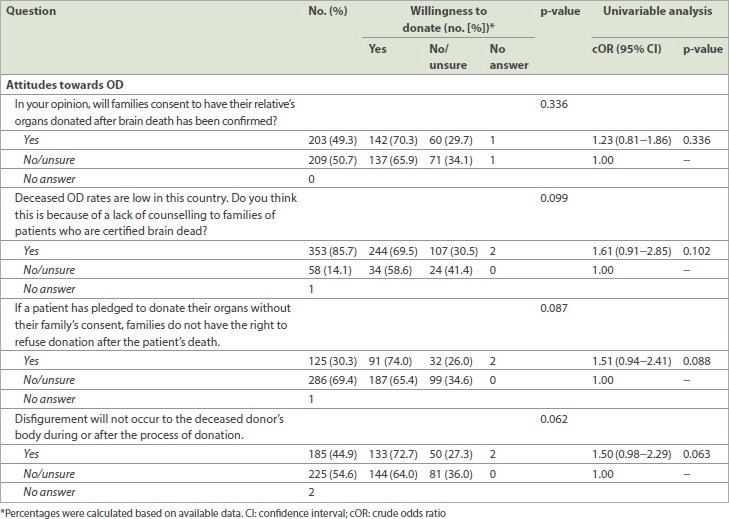
There was no statistically significant association between willingness to donate and HCPs’ beliefs regarding families’ consent to OD (cOR 1.23, 95% CI 0.81–1.86, p = 0.336). Lack of family counselling (p = 0.102), the right to refuse OD (p = 0.088) and disfigurement after OD (p = 0.063) were also not significantly associated with the willingness to donate (
Table V
Association of attitudes towards organ donation (OD) with willingness to donate.
Out of the 410 HCPs who responded, 279 (68.0%) expressed their willingness to donate organs, but only 267 answered the question on informing their family about their wish to donate; 176 (63.1%) responded that they had informed their family. Of the 279 HCPs who were willing to donate, only 104 (37.3%) were carrying a donor card at the time of this study. Interestingly, six HCPs who answered ‘No’ or ‘Unsure’ regarding their willingness to donate also reported that they were carrying a donor card.
DISCUSSION
In contrast to previous studies in Malaysia, this study focused on HCPs caring for critically ill patients who may become eligible organ donors. We found that sociodemographic factors such as profession, religion and ethnicity were associated with HCPs’ willingness to donate their own organs. Religious belief, belief in BD and confidence in transplantation were also associated with their willingness to donate. In Malaysia, willingness towards OD among HCPs in general was less than 50%, as shown by Rozaidi et al and Abidin et al.(2,9) In our study population, 68.0% were willing to donate. This difference may be due to the nature of the selected study population, which directly deals with OD. The majority of our HCP population from the critical care areas studied were nurses, who were significantly less willing to donate compared to doctors. Other studies have reported similar observations.(9,26,33)
Malays of Muslim faith were the largest ethnic group in our study population, consistent with that of the general population in Malaysia. They were found to be significantly less willing to donate compared to other religions and ethnicities. Malays were observed to comprise only 6% of all donors although they form 68.6% of the population(34) and have the potential to be the largest donor pool in Malaysia if their willingness to donate can be improved.
It has been shown that people are more willing to donate if they anticipate the support of a religious leader and the religious community.(35) In one study, Islamic views supporting concepts of transplantation showed the strongest positive influence for OD both during life and at death.(36) National and state fatwas (decrees) on OD have been issued in Malaysia, stating that OD was not forbidden in Islam.(37) In one study, Malays who were aware of the correct Islamic fatwa on OD were shown to be more willing to donate.(8) One factor for the lower willingness to donate found in this study may be the inaccurate perception of OD among the Muslim community.(37) In another local study, less than half of the Malays interviewed were aware that a fatwa on OD even existed, and one-third of those who were aware of its existence thought that the fatwa was against OD.(8) Our results were similar to those of another study demonstrating that people who believed their religion did not allow OD showed no motivation to donate in the future.(35) Therefore, clearing up the religious misconceptions of HCPs would improve their willingness to donate.
We found that the better the knowledge of HCPs, the more willing they were to donate, with BD test scores having the strongest correlation. This is consistent with international studies suggesting that HCPs who understand the concept of BD have more positive attitudes towards OD.(14,15,17) It has been suggested that critical care nurses have inadequate knowledge of BD, OD and organ transplantation and that this may explain why they are less willing to donate.(20,24,38) In a study by Loch et al, some HCPs did not adequately understand the concept despite having tertiary education.(8) Thus, educational programmes to improve understanding of BD and bedside tests for BD are urgently needed in the critical care setting.
Our study showed that HCPs with positive attitudes towards BD and confidence in transplantation were more willing to donate. HCPs were also more willing to donate if they were convinced of the existence of BD, which is consistent with previous studies.(17) Non-recognition of BD and misconceptions about BD were said to be factors that contributed to a shortage of organs from deceased donors.(9) Misconceptions about BD may lead to aversion towards OD, which could affect HCPs’ own willingness to donate.(39)
The majority of the HCPs had confidence in transplantation and believed that it was a good form of treatment for end-stage organ disease and were confident of the outcome of the procedure. However, in the multivariable logistic regression analysis shown in
HCPs who believed there could be disfigurement after donation were as willing to donate as their counterparts. This is in contrast with other studies showing that only HCPs who were unconcerned about disfigurement were more inclined to donate.(14,15,40) Even HCPs who thought that families had the right to refuse OD or that there was lack of counselling were willing to donate as compared to their counterparts. Overall, HCPs personal attitudes towards OD did not appear to influence their own willingness to donate.
Possession of an organ donor card has been studied as an indicator of HCPs’ willingness to donate.(16,21) Our study revealed that only 28.4% of HCPs possessed an organ donor card although most were willing to donate. This is in line with other studies that showed that possession of an organ donor card did not accurately reflect the actual number of HCPs willing to donate.(20,24,38,41) Non-cognitive reasoning may have led to the belief that a donor card or discussion about OD carried bad luck (‘jinx’ factor) and was disgusting (‘ick’ factor).(42) Moreover, medical distrust, desecration of bodily integrity and anticipated regret strengthen these potential barriers.(39,42)
As in other countries, families’ consent is required in Malaysia for deceased OD. However, in our study, one-third of the HCPs who were willing to donate had not informed their family of their intention. Families who are unaware of the deceased person’s wishes may refuse consent and potential donors can be lost.
Our study had a few limitations. It was conducted in Hospital Kuala Lumpur, which is the largest transplant centre in Malaysia. Although our high response rate and a good proportionate representation from different ethnicities added to the strength of the study, this was a single-centre study, and hence the data may not be representative of HCPs in the rest of Malaysia. Furthermore, knowledge and attitudes of family members of potential donors in critical care areas were not explored as part of this study. An understanding of these would shed light on factors such as their expectations, concerns and decision-making process in giving consent for their relatives’ organs to be donated.
In conclusion, critical care HCPs can contribute to OD in various ways, including advocating for it. They should possess an adequate understanding of OD and the issues surrounding it, including BD as well as ethical, legal and religious issues. In our study, the willingness to donate of HCPs working in critical care areas was found to be higher than that of HCPs in general. However, significant knowledge gaps as well as certain beliefs and perceptions that could pose a barrier to OD were identified in this group. Although the majority of the HCPs were willing to donate their organs, one-third of them had not informed their families and nearly two-thirds did not possess an organ donor card. In future studies, targeted efforts to improve critical care HCPs’ knowledge, attitudes and beliefs towards OD are needed to increase their willingness for OD. This is likely to influence their advocacy for OD and their approach to the families of potential OD patients in critical care units.
ACKNOWLEDGEMENTS
The authors would also like to thank Datin Dr Fadhilah Zowyah Lela Yasmin Mansor (National Transplant Resource Centre, Kuala Lumpur, Malaysia), Prof Karen Morgan and Assoc Prof Dr Manoj Valappil (Perdana University-Royal College of Surgeons in Ireland) for expert advice, Dr Yuzana Yusop (National Transplant Resource Centre, Kuala Lumpur, Malaysia) for forward translation to Malay, Dr Anne Jamaludin (Perdana University Royal College of Surgeons in Ireland) for back translation, Datuk Dr Noor Hisham Abdullah (Director General of Health, Ministry of Health, Malaysia) for allowing us to conduct this study, and the staff of Hospital Kuala Lumpur, Malaysia, for participating in this study.


