INTRODUCTION
Influenza is a highly infectious respiratory viral illness that is transmitted through respiratory droplets propelled by coughing and sneezing or through contact with contaminated surfaces. The contagious period is from one day before onset of symptoms till 5–7 days after onset. Common symptoms include fever, headache, chills, cough, sore throat, muscle aches and generalised malaise and fatigue. Influenza is common in Singapore, with between 1,500 and 3,500 people experiencing influenza-like illness weekly. Certain populations such as pregnant women are more susceptible to developing complications such as severe illness, hospitalisation, admission to an intensive care unit and death. There have also been reports of influenza infection in pregnancy being associated with an increased risk of obstetric complications such as spontaneous abortion, preterm delivery, low birth weight and fetal death. Antenatal influenza vaccination therefore helps to reduce the risk of serious maternal medical complications while providing passive protection to the neonate via transplacental transmission of antibodies, especially in the initial few months of life. Various international guidelines such as those from Public Health England,(1) the American College of Obstetricians and Gynecologists (ACOG),(2) the Royal Australian and New Zealand College of Obstetricians and Gynaecologists(3) and the Society of Obstetricians and Gynaecologists of Canada (SOGC)(4) recommend that inactivated influenza vaccine be offered to pregnant women at any stage of pregnancy. Current local guidelines such as Singapore’s Clinical Practice Guidelines on Adult Vaccination (April 2016)(5) as well as the Ministry of Health’s National Adult Immunisation Schedule (NAIS)(6) also recommend routine influenza vaccination in pregnancy.
Pertussis, commonly known as whooping cough, is a highly contagious respiratory disease caused by the bacterium Bordetella pertussis. It is transmitted via coughing or sneezing or via close contact in an enclosed environment. Symptoms usually develop within 5–10 days after exposure, but the incubation period may last as long as three weeks. Pertussis has an insidious onset, with catarrhal symptoms that are indistinguishable from those of minor respiratory tract infections. The cough, which is initially intermittent, becomes paroxysmal, and typically persists for 1–6 weeks or more. There has been an increase in the number of reported cases of pertussis since the 1980s. Factors contributing to this include an increased awareness of pertussis among healthcare practitioners, greater access to and use of laboratory diagnostics, increased surveillance and reporting of pertussis infections to public health departments, and waning immunity from vaccines. A recent publication modelling pertussis cases and deaths estimated that in 2014, there were 24.1 million pertussis cases and 160,700 deaths in children younger than five years worldwide.(7) Locally, the number of whooping cough cases has more than doubled since 2013, with the number of laboratory-confirmed cases of pertussis increasing from 17 in 2013,(8) to 57 in 2015(9) and to 86 in 2016.(10) More than half of the cases reported in 2015 and 2016 occurred in infants aged less than six months.
Neonates and infants are at particularly high risk for developing serious pertussis infection, as they remain vulnerable until they can be vaccinated at two months of age. Unvaccinated or incompletely vaccinated infants have the highest risk of severe illness including hospitalisation and death. In this particular group, about half require inpatient therapy, most commonly in infants less than six months of age. Of those infants with pertussis requiring inpatient therapy, approximately 61% will have apnoea, 23% pneumonia, 1.1% seizures, 1% death and 0.3% encephalopathy as a result of hypoxia from coughing or toxins.(11) Experience with vaccination of pregnant women in the United Kingdom indicates the great impact of vaccination in reducing infant pertussis-related mortality,(12) which is likely due to the direct protection conferred by the transfer of maternal antibodies. Various international guidelines such as those from Public Health England,(13) ACOG(2) and the SOGC(4) recommend tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccination during each pregnancy to provide maximal protection to every infant, as vaccine-induced pertussis antibodies wane over time and the protective antibody level required in newborn infants remains unknown.
Recognising the clinical benefits and impact of antenatal vaccination, the Ministry of Health, Singapore, recently extended the use of Medisave for vaccines under the NAIS. From 1 November 2017, Singaporeans have been able to use their Medisave funds, which are funds set aside specifically for healthcare expenses under Singapore’s compulsory Central Provident Fund savings scheme, for NAIS vaccinations at Medisave-accredited healthcare institutions, such as hospitals, polyclinics and Community Health Assist Scheme general practitioner clinics. These include both the influenza vaccine and the Tdap vaccine.
However, in spite of the recommendations from local and international bodies, vaccination uptake rates in general remain inadequate. For example, even when free flu vaccines were offered to all pregnant women under the British National Health Service, the uptake among pregnant mothers was low and trending downward, with only 42% of pregnant women in England getting vaccinated in the winter of 2015/16, down from 44% the winter before.(14) Locally, the Singapore National Health Surveillance Survey in 2013 found that only 15.2% had received seasonal influenza vaccination in the past year.(15)
Attitudes and beliefs held by obstetricians is an important factor that may impact the successful implementation of universal vaccination during pregnancy. A key underlying factor is obstetricians’ knowledge about vaccination in pregnancy in terms of its safety, effectiveness, benefits and recommendations in guidelines. Our study aimed to assess the knowledge, attitudes and current practices of obstetricians in Singapore regarding the delivery of antenatal Tdap and influenza vaccines, as well as to elicit their perceived barriers to maternal immunisation.
METHODS AND RESULTS
This cross-sectional study was conducted in July 2017. A questionnaire assessing the knowledge, attitudes and current practices of obstetricians regarding maternal immunisation, and exploring their perceived barriers to maternal immunisation was sent to target participants by email. Participants were obstetricians from public institutions (KK Women’s and Children’s Hospital, Singapore General Hospital and National University Hospital) as well as the private sector in Singapore, and included full-fledged specialists and residents at various levels of training. The questionnaire is shown in the Appendix.
Study population
A total of 76 obstetricians participated in the study. Survey participants comprised 25 (33%) consultant level obstetricians (i.e. associate consultants, consultants and senior consultants) and 51 (67%) non-consultant level obstetricians (i.e. medical officers, residents and registrars). The majority (82%, n = 62) of the participants were from the public sector, with the remaining 14 (18%) participants from the private sector.
Knowledge and practices
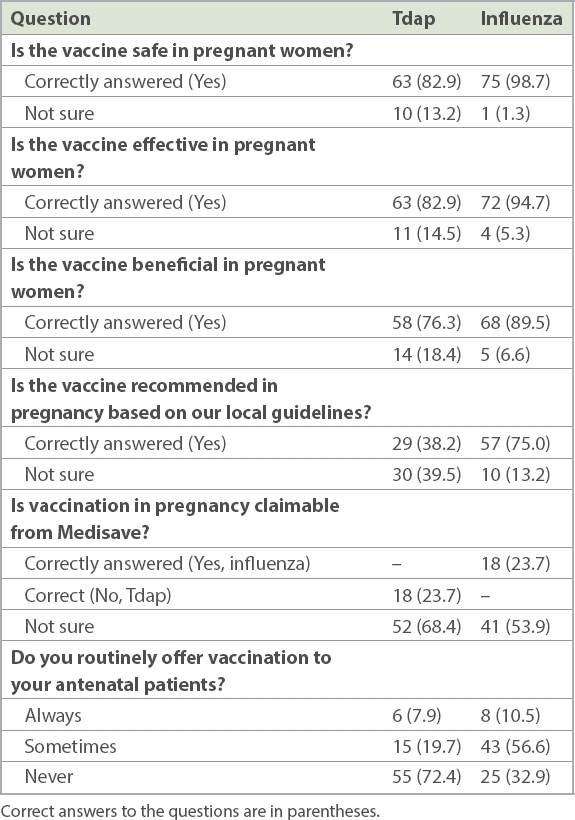
Obstetricians were assessed on their knowledge of recommendations and self-reported immunisation practices (
Table I
Obstetricians’ knowledge of recommendations on Tdap and influenza vaccination for pregnant women and self-reported immunisation practices (n = 76).
Barriers to vaccination
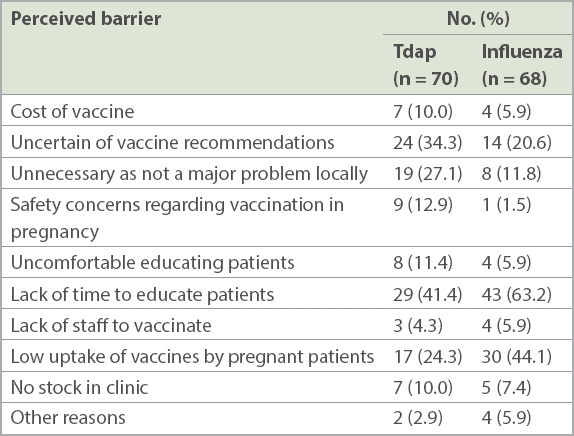
Table II
Perceived barriers to Tdap and influenza vaccination among obstetricians.
DISCUSSION
This survey revealed important points about maternal immunisation within Singapore. Firstly, a substantial number of obstetricians displayed knowledge regarding safety and effectiveness of influenza and Tdap vaccines in pregnancy. However, in spite of this knowledge, the rate of obstetricians offering antenatal vaccination is comparatively low, particularly for pertussis. This could be partly due to uncertainty regarding vaccine recommendations, with 24 (34.3%) obstetricians citing this as a reason to not routinely offer Tdap vaccination in their practice. At the time of the survey in July 2017, maternal immunisation against pertussis was already recommended in international guidelines.(4,13) The Ministry of Health, Singapore, later released guidelines in September 2017 recommending Tdap vaccination between 16 and 32 weeks’ gestation during each pregnancy, regardless of the interval from a previous Tdap vaccination.(6) The launch of these local guidelines will likely help to encourage obstetricians to actively promote antenatal Tdap vaccination for the benefit and promotion of neonatal and infant well-being.
One major barrier to Tdap vaccination was the lack of recognition that pertussis was a major problem locally. There is certainly a need for greater knowledge and awareness of pertussis infection as a contemporary local and global health burden. Only then can obstetricians themselves feel compelled to include these antenatal vaccinations in the routine antenatal care they provide. This is a critical component of success in any vaccination programme, as studies have shown that women are more likely to receive vaccinations in pregnancy if recommended to do so by a healthcare provider.(16-19) The active promotion of antenatal vaccination by obstetricians and primary health physicians would help to increase patients’ confidence in the effectiveness and safety of the influenza and Tdap vaccines, thereby improving their uptake.
Another two major and recurring obstacles we identified were the limited consultation time for patient education as well as perceived vaccine hesitancy and rejection by pregnant women. To combat these barriers, patient education and exposure could be reinforced via educational materials such as patient leaflets and pregnancy apps. Empowering nurses to promote, counsel and administer antenatal vaccines could also help to reduce clinic consultation times while still ensuring that every woman is appropriately counselled on Tdap and influenza vaccination in pregnancy and routinely offered these vaccines.
Lastly, cost was one of the barriers identified that potentially deterred pregnant women from vaccination. Many obstetricians were unaware that patients could use Medisave to offset the cost of the influenza vaccine. As of 1 November 2017, the Tdap vaccine is also a Medisave-claimable vaccine. Making this information known to patients at the time of counselling for maternal immunisation could help to remove the cost barrier, especially for families struggling to cope with the cost of antenatal care.
Our study was not without limitations. Firstly, the small sample size of 76 respondents was a contrast to the 326 obstetricians registered in Singapore, according to the 2017 Singapore Medical Council Annual Report, limiting the generalisability of the study findings. Secondly, although our study endeavoured to be as inclusive as possible by surveying obstetricians from both the public and private sectors, private sector obstetricians, who account for approximately two-thirds of all obstetric specialists in Singapore, were under-represented in this study. It is therefore possible that our findings may not be representative of the general trend of obstetric practice in Singapore. Lastly, although we attempted to maximise participation through ensuring the anonymity of survey respondents, as their participation was completely voluntary, one potential limitation encountered was that of a non-response bias. As non-respondents may have different perceptions, knowledge and immunisation practices compared to respondents, their non-participation in the survey may potentially skew the study findings. Future studies with a larger sample size could be conducted to improve the overall representativeness of the findings. Studies assessing patients’ knowledge and perception of antenatal vaccination would also be useful to explore potential barriers from the perspective of the patient.
CONCLUSION
Maternal immunisation against influenza and pertussis infection is safe, effective and beneficial. In recent years, there has been an increasing awareness of the importance of maternal immunisation in improving maternal outcomes in pregnancy as well as neonatal outcomes in the first few months of life. Obstetricians who are primarily responsible for the care and health of pregnant women and their unborn children need to view influenza and Tdap vaccination as an integral component of antenatal care, and take on an active role in educating and supporting women to make the best decision for their babies and themselves.
SUPPLEMENTARY MATERIAL
The Appendix is available online at https://doi.org/10.11622/smedj.2019170.


