Abstract
INTRODUCTION
Perinatal transmission remains one of the important causes of transmission of the human immunodeficiency virus (HIV). Over the years, with better knowledge and awareness of HIV infection, the perinatal transmission rate has been significantly reduced. We previously reported on the pregnancy outcomes of HIV-positive mothers from 1997 to 2007 in our institution. This article aimed to review the standards of care of HIV-positive pregnant women since then.
METHODS
A retrospective study reviewed 84 HIV-positive women who delivered in a tertiary centre from January 2008 to December 2015. Patient demographics and antenatal, intrapartum, postnatal and immediate neonatal data were analysed.
RESULTS
A total of 97 deliveries with 98 neonates were recorded; 12 women delivered more than once, and there was one set of twins. The mean maternal age at diagnosis of HIV infection was 27.8 years. Of the study population, 63.1% of women were non-Singaporeans. 56 women were known to have HIV infection on presentation and 90.7% were on antiretroviral therapy during pregnancy. 88.7% of the women received intrapartum intravenous zidovudine, and 93.1% of women with detectable and 58.7% with undetectable viral load underwent Caesarean sections. All neonates were HIV-negative.
CONCLUSION
The high standards of care for HIV-positive women have successfully reduced our perinatal transmission rate to zero.
INTRODUCTION
Singapore has seen a steady increase in the number of human immunodeficiency virus (HIV)-positive patients since the diagnosis of its first case on 16 May 1985.(1) An average of 450 new cases have been reported every year since 2008. In 2015, 455 new cases of HIV were reported among Singapore residents, increasing the total number of HIV-infected Singapore residents to 7,140. Of these 455 patients, 7% were female, with the most common mode of transmission being sexual intercourse with an infected individual.(2)
Perinatal transmission remains an important cause of HIV spread.(3) Over the years, improvements in knowledge about HIV and public awareness, routine antenatal HIV testing, access to anti-retroviral agents for both mother and neonate, delivery via Caesarean section (CS) when appropriate and avoidance of breastfeeding have successfully reduced the vertical transmission rate to less than 2%(4) when compared with transmission rates of 25%–30% with no interventions.(5)
Globally, the number of new infections diagnosed per year among children has decreased by 56% since 2010 and by 70% since 2000.(3) An estimated 1.6 million new HIV infections among children have been averted since 1995 owing to the provision of antiretroviral medicines to women with HIV infection during pregnancy and breastfeeding, with the majority of reductions (1.3 million) occurring between 2010 and 2015. Still, over 300,000 women did not receive antiretroviral medicines to prevent mother-to-child transmission in 2015.(3)
In Singapore, 31 cases of perinatal HIV transmission were reported from 1985 to 2014, of which there were 29 cases from 1985 to 2007 and only two cases being reported between 2008 and 2014.(6) Following on a previous study that reported the pregnancy outcomes of HIV-positive mothers from 1997 to 2007,(1) this study aimed to review the epidemiology and management of HIV-positive pregnant women and the vertical transmission rates in our centre from 2008 to 2015.
METHODS
This was a retrospective study involving all HIV-positive women who delivered at KK Women’s and Children’s Hospital, Singapore, over an eight-year period from January 2008 to December 2015. KK Women’s and Children’s Hospital is a tertiary referral centre that provides care for over 14,000 women and their babies every year, which accounts for about one-third of the total number of babies born in Singapore.
As part of their routine antenatal blood tests, screening for HIV infection, hepatitis B and syphilis is offered to all expectant mothers in Singapore on an opt-out basis. All women who are HIV positive are promptly referred to an infectious disease (ID) physician upon diagnosis and commenced on antiretroviral therapy (ART) in the early second trimester, unless they were already on ART prior to the pregnancy. In keeping with the local protocol, all HIV-positive pregnant women are also offered screening for other sexually transmitted diseases such as hepatitis C, gonorrhoea and chlamydia.
A viral load (VL) test for HIV is routinely performed in the third trimester and is used as a preferred investigation over cluster of differentiation 4 (CD4) levels for planning the mode of delivery. A normal vaginal delivery (NVD) is encouraged for VL < 1,000 copies/mL, while women with VL > 1,000 copies/mL would be offered an elective or planned CS to minimise the chances of vertical transmission. Zidovudine infusion (2 mg/kg over one hour followed by 1 mg/kg/h) is routinely started four hours before a planned CS or at the onset of labour for those undergoing NVD and continued until the umbilical cord is clamped. All women are advised against breastfeeding, and postpartum contraception options are discussed. All patients are referred to ID physicians postnatally, and postnatal ART regimes and follow-up are arranged prior to discharge.
At our institution, all neonates are administered zidovudine at birth, with additional lamivudine and nevirapine therapy if their mothers are unbooked or if ART is started less than two months prior to the delivery. HIV proviral DNA polymerase chain reaction is performed at one and four months of age, while the HIV confirmatory antibody test is performed at 15–18 months of age. Uninfected babies are defined as those who show negative results in all three tests. A positive test is confirmed by a repeat test immediately, with the baby being defined as HIV positive if the confirmatory test is positive.
For this study, a list of HIV-positive mothers was generated from the database of babies who were delivered by HIV-positive women in our hospital from our ID service. Patient demographics; antenatal data (i.e. details on HIV diagnosis, ART use and follow-up, VL and CD4 counts, mode of delivery); and intrapartum, postnatal care and immediate neonatal outcomes were collected. Women who were lost to follow-up and did not deliver in our institution were excluded. Data was analysed using IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA). All results were reported as mean (range), unless otherwise stated.
Ethics approval for this study was sought from the SingHealth Centralised Institutional Review Board. Waiver of consent was deemed appropriate, as this was a review of case records only.
RESULTS
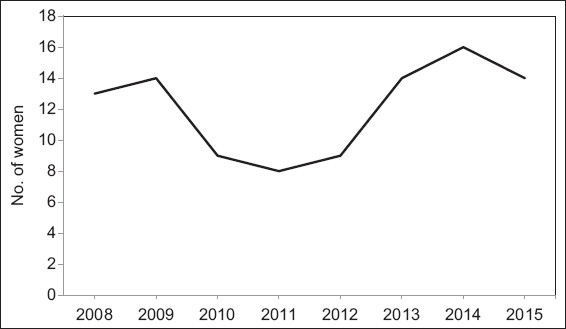
Between January 2008 and December 2015, a total of 97 pregnancies in 84 HIV-positive women were recorded at KK Women’s and Children’s Hospital. 11 women had two pregnancies and one woman had three pregnancies. This resulted in 98 neonates in total, including a set of twins. During study period, a decline in the number of HIV-positive women was observed, from 13 cases in 2008 and 14 cases in 2009 to less than ten cases in 2010–2012, followed by an increase thereafter (
Fig. 1
Chart shows the trend in the number of HIV-positive pregnant women at KK Women’s and Children’s Hospital during the study period.
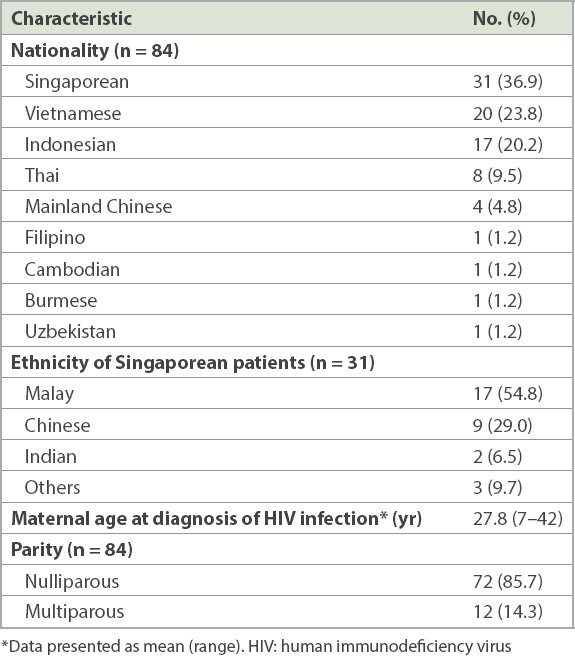
The demographic details of the patients (n = 84) are shown in
Table I
Patient demographics.
The antenatal characteristics of the study population are shown in
Table II
Antenatal characteristics of the pregnancies (n = 97).
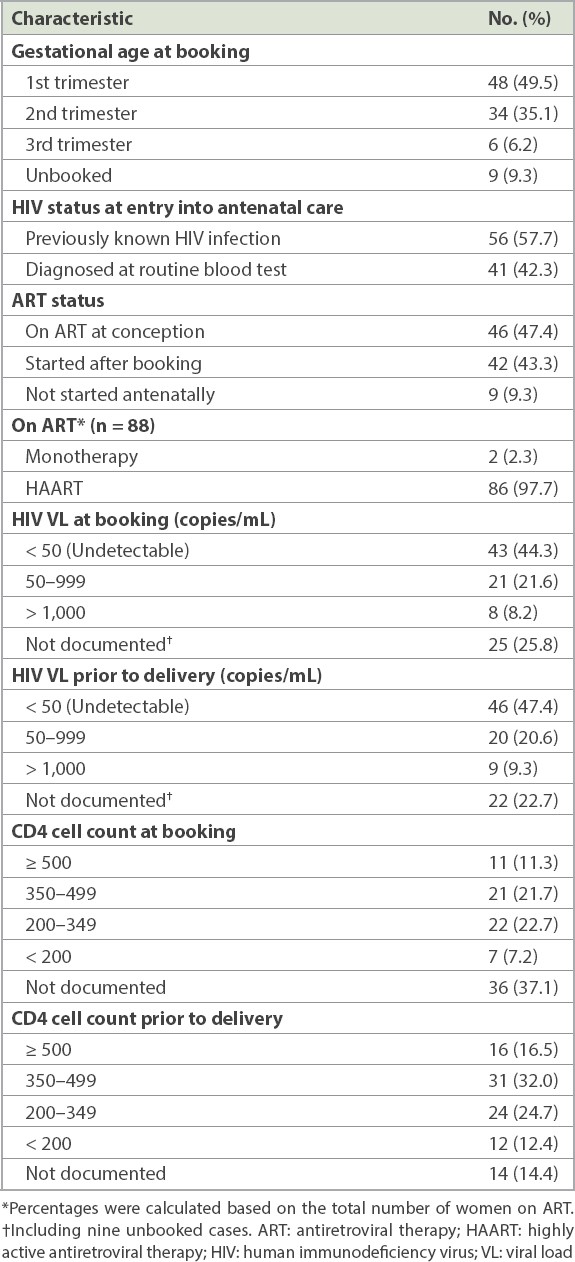
At the booking visit, 56 (57.7%) women were known to be HIV positive, while the remaining 41 (42.3%) were diagnosed using RBT in the current pregnancy. Of these 41 pregnancies, 16 (39.0%), 15 (36.6%) and 4 (9.8%) were booked in the first, second and third trimesters, respectively, and 6 (14.6%) were unbooked at delivery. The HIV status of the spouse was documented in case files for only 23.1% of the pregnancies. Of these, 57.0% of the spouses were HIV negative at the time of documentation.
Overall, 46 (47.4%) pregnancies were conceived while on ART, and the majority continued their original regime. Changes to established ART regimes were made in eight pregnancies to control their persistently high VL. ART was started in 42 (43.3%) pregnancies in the second trimester. 9 (9.3%) women did not receive any antenatal treatment: six women had not sought any antenatal care during the pregnancy, and three women had sought antenatal care but defaulted subsequent consultations and had an unknown HIV status at the time of delivery. Overall, 88 (90.7%) of pregnancies were on ART. Of these, the majority (97.7%) were on highly active antiretroviral therapy (HAART) and 2.3% were on oral zidovudine monotherapy.
In our study, concomitant hepatitis B infection occurred in 5 (5.2%) pregnancies and syphilis in 4 (4.1%) pregnancies. There were no pregnancies with concomitant hepatitis C infection. Results for chlamydia and gonorrhoea infections were available for only 14 pregnancies, which included one chlamydia infection. Four women in the study population had a history of treated opportunistic infections, including pneumocystis pneumonia in one and pulmonary tuberculosis in three women.
At booking, VL was undetectable in 43 (44.3%) pregnancies and detectable in 29 (29.9%) pregnancies, of which 8 (8.2%) had a VL of more than 1,000 copies/mL. VL was not documented for 25 (25.8%) women. Results of VL tests repeated prior to delivery were largely unchanged, with the number of pregnancies with undetectable VL increasing from 43 (44.3%) to 46 (47.4%). Detectable VL remained unchanged in 29 (29.9%) pregnancies. Of these, interestingly, 9 (9.3%) had a VL of more than 1,000 copies/mL. VL prior to delivery was not documented in 22 (22.7%) pregnancies. The CD4 count was more than 350 cells/mL in 47 (48.5%) women prior to delivery, in contrast to 32 (33.0%) women at booking.
Table III
Intrapartum and perinatal characteristics of the pregnancies (n = 97).
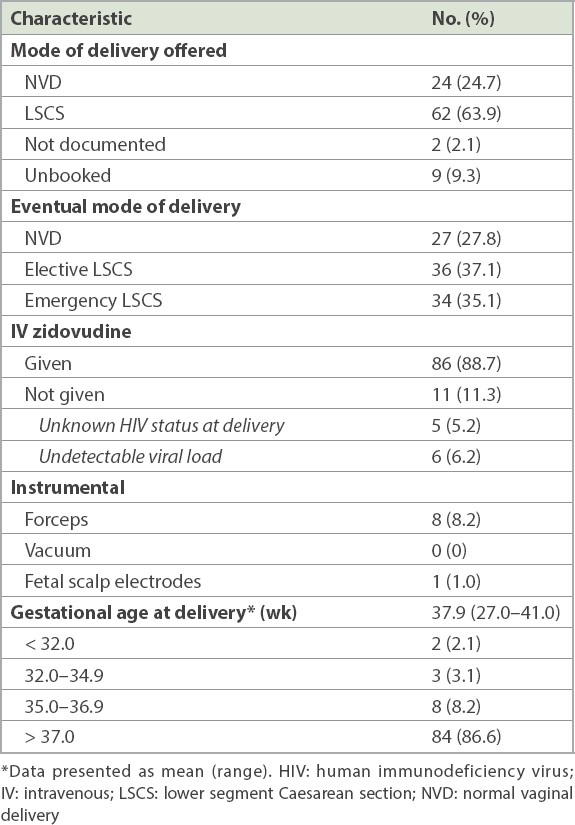
The majority (88.7%, n = 86) of the 97 women in our study received intrapartum intravenous (IV) zidovudine as per the standard of care. Of those who did not receive IV zidovudine (11.3%, n = 11), 6.2% (n = 6) did not require it, as their maternal VL was undetectable.(7) The remaining 5.2% (n = 5) delivered soon after presentation, prior to the availability of their HIV infection status.
Forceps were used to deliver 8 (8.2%) neonates, and the positive HIV status of their mothers was known for all of them. Of these, seven women had an undetectable VL. In five cases, forceps were used during CS delivery, including the woman who had a detectable VL. Fetal scalp electrode was used for fetal monitoring in one woman, as she was unbooked and had an unknown HIV status at presentation during labour. She did not receive IV zidovudine.
Among the 27 women who had NVD, 19 had undetectable VL and two had detectable VL. Out of the 70 women who underwent CS, 27 had undetectable VL and 27 had detectable VL. The majority (93.1%, n = 27) of the 29 women with a detectable VL underwent an uneventful CS. 2 (6.9%) women underwent an unplanned NVD as they presented when in advanced labour, although one of them had a VL of 4,608 copies/mL. In comparison, 58.7% (n = 27) of the 46 women with an undetectable VL underwent CS. The indications for CS were maternal request (55.6%), previous CS (22.2%), failed induction of labour (7.4%), breech presentation (7.4%) and severe preeclampsia (7.4%). The VL was unknown in the remaining 22 women, of whom 6 (27.3%) had NVD and 16 (72.7%) underwent CS.
A total of 98 live births were recorded in our study population. The mean gestational age at delivery was 37.9 (27–41) weeks, and 86.6% of deliveries occurred at term. The mean birth weight was 2,791 (1,294–3,738) g. 91 (92.9%) neonates had an Apgar score of 9 at both one and five minutes of life. There was 1 (1.0%) neonatal death in an unbooked multiparous woman with unknown HIV status at delivery. She was found to be HIV- and hepatitis B-positive after delivery. She presented in advanced labour with pyrexia and ruptured membranes of almost 17 hours’ duration. The baby was estimated to be at about 27 weeks of gestation and weighed 1,000 g at birth. The neonate was born with Apgar scores of 1 and 2 at one and five minutes of life, respectively, and died at 10.5 hours of life owing to refractory septic shock secondary to maternal chorioamnionitis and severe prematurity. The remaining 6 (6.1%) neonates had an Apgar score of 5–8 at one minute and 9 at five minutes of life.
All except one baby, who returned overseas, received further treatment in our institution. Of the remaining 96 live births who were subsequently evaluated and followed up at our centre, none were found to be infected with HIV.
DISCUSSION
Between 2018 and 2019, no cases of HIV mother-to-child transmission were observed in our hospital. Available data from a study by Chin et al(1) from 1997 to 2007 in Singapore provides interesting comparisons. In their study, 58% of HIV-positive women were foreigners, which was similar to the corresponding value of 63.1% in our study. However, the majority (70%) of women in their study were 20–29 years of age, while in our population, the mean maternal age at booking was 30.1 years. In their study population, only 21% of women booked for pregnancy care in the first trimester, compared to nearly half (49.5%) of the women in our study. This could be attributed to improved patient awareness of their disease and implications for the pregnancy, as well as better collaboration with ID physicians over the years.
The vertical transmission rate in our study population was 0%, in contrast to a previous study conducted in Singapore(1) that showed a vertical transmission rate of 5.3%. A likely explanation for this reduction could be that the majority of our study population booked in the first trimester, in contrast to the previous study, and were managed in a well-established multidisciplinary setting throughout the pregnancy.
The other important risk factor for vertical transmission is believed to be advanced maternal disease with a high VL.(8) Hence, women with HIV VL above 1,000 copies/mL near delivery should deliver by CS to minimise the risks of vertical transmission. In our study, the majority (93.1%) of women with detectable VL underwent CS, and only 2 (6.9%) women who presented in very advanced labour delivered vaginally. These two neonates were not breastfed and received ART as per protocol, and remained HIV negative at 18 months of age. Further, avoidance of breastfeeding constitutes an important risk reduction(4) strategy for reducing perinatal transmission of HIV. In our study population, none of the women breastfed their infants, as they had all been advised against breastfeeding postnatally. All neonates in our study were administered zidovudine at birth, with additional lamivudine and nevirapine therapy if their mothers were unbooked or ART was started less than two months prior to the delivery. This successfully reduced the vertical transmission rate in our study to 0%.
In women with low VL (< 1,000 copies/mL), the surgical risks from CS outweigh the benefits of reduction of vertical transmission from a low VL (< 2%).(9) However, in our study, over half (58.7%) of the women with undetectable VL underwent CS, with the main indication being maternal request. We feel that this could be attributable to the traditional belief that all HIV-positive mothers must undergo CS to prevent vertical transmission among patients and caregivers. This emphasises the importance of continual education of patients and caregivers on the surgical risks and implications of CS in future pregnancies to avoid unnecessary CS.
Previously identified risk factors such as prolonged duration of membrane rupture (i.e. of more than four hours)(10,11) and mode of delivery (i.e. vaginal)(12) were shown to have minimal effect on vertical transmission in women who have achieved viral suppression on HAART. Our study concurs with these findings, as detectable VL was present in five women and unknown in one woman among the 29 women with ruptured membranes in our study population. They were all on HAART and delivered via CS. None of these neonates were infected with HIV.
The field of ART has changed. Monotherapy with antenatal and intrapartum zidovudine for the mother, and for the newborn for six weeks, was the initial mainstay of treatment when it was first reported in the PACTG 076 study(4) in 1994, resulting in a 67% relative reduction in the risk of HIV transmission from 25.5% to 8.3%. Over the years, this has been replaced by combination ART or HAART, which was shown to be more effective in reducing mother-to-child transmission to less than 2% of deliveries in HIV-positive women,(4) making HAART the standard of care. The majority (97.7%) of the women in our study received HAART. Of note, two women in our study population were on monotherapy – one woman was on oral zidovudine and was unbooked at presentation, while the other booked in the second trimester and had a booking CD4 count > 350 cells/mL.
Screening for other sexually transmitted diseases is also vital in HIV-positive pregnancies. In our study, five women were hepatitis B positive, of which four women received the recommended treatment of tenofovir, together with lamivudine or emtricitabine, in addition to a third ART agent such as a protease inhibitor or non-nucleoside reverse transcriptase inhibitor.(13) The remaining hepatitis B-positive woman was unbooked with unknown HIV and hepatitis B status at delivery. Syphilis screening is crucial to prevent not only congenital syphilis but also HIV, as syphilis has been associated with an increased risk of vertical transmission of HIV.(14) Syphilis screening is part of routine antenatal blood tests in Singapore. All four women who had antenatal syphilis in our study population were treated.
Our study was conducted in the largest obstetric tertiary centre where the majority of high-risk pregnancies in Singapore are referred. This forms the major strength of our article, as the data is robust and likely includes the majority of HIV-positive women seeking antenatal care. As it was a follow-up of a previous study conducted in the same centre, we were able to compare our outcomes with those of the previous study including the reduced vertical transmission rate, which can be attributed to better management strategies adopted over the years.
However, our study has a few limitations. There is a lack of long-term data about the impact of the use of ART during pregnancy and the early neonatal period on the subsequent development of these children and on screening for opportunistic infections(15) such as Pneumocystis jiroveci pneumonia, Mycobacterium tuberculosis, Mycobacterium avium complex infection and Cytomegalovirus retinitis. Data regarding maternal vaccination for our study population was also lacking.
In conclusion, the importance of early diagnosis, established protocols, multidisciplinary team care and continual patient education cannot be overemphasised. This is evident in our population, whose perinatal transmission rate was successfully reduced to zero. However, there was a low vaginal delivery rate in HIV-positive mothers who were on HAART and had undetectable VL prior to delivery, as well as a significant proportion of women who defaulted their postnatal follow-up. Innovative interventions are required to improve long-term adherence to ART among HIV-positive mothers.


