Abstract
Major depression is common in the primary care setting. In the final article of this series, we illustrate the approach to the management of depression in primary care. Psychotherapy has been shown to be as effective as antidepressants for mild to moderate major depression. The common myth that antidepressants are addictive should be addressed. Antidepressants should be started at a subtherapeutic dose to assess tolerability, then gradually increased until a minimally effective dose is achieved. Apart from pharmacotherapy and psychotherapy, management of depression should include managing stressors, engaging social and community support, dealing with stigma and discrimination, and managing concomitant comorbidities. A strong therapeutic relationship and empathic listening are important between the primary care physician and patient.
Joseph, a 45-year-old shipping clerk, visited your clinic. Upon reviewing his notes and laboratory results, you noted that he had missed his appointment by two months. His blood pressure and glycaemic control were poor. Joseph was in a crumpled shirt and avoided eye contact, and was not forthcoming at the start of the consultation. You astutely asked about his mood and identified anhedonia, disturbed sleep, poor appetite, poor energy levels and difficulty concentrating at work. You noted that he had problems at work and was also stressed out at home, as he was the main carer for his mother who had dementia. Screening for suicide risk, you assessed that he had no active suicidal ideation, although he did wonder at times if life was worth living. You made the diagnosis of moderate depression, with caregiving and work stress as his contributing factors.
WHAT IS MAJOR DEPRESSION?
Major depression is a mood disorder that presents with either a persistent feeling of sadness or loss of pleasure, or both.(1) In this article, we describe the management of depression in primary care. This follows earlier articles that discussed the diagnosis of major depression and the important differentials to consider when a patient presents with low mood,(2) and the assessment of suicide risk.(3)
HOW RELEVANT IS THIS TO MY PRACTICE?
By applying the criteria described in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), as well as using screening tools in at-risk patients,(1) the primary care physician can establish the diagnosis of major depression. Despite this, it has been shown that more than two-thirds of persons with mental health disorders do not seek help.(4) Barriers to obtaining care include lack of financial means (e.g. having no Medisave accounts), stigma and lack of primary care involvement in the care of persons with mental disorders.(5) As primary care practitioners are accessible and can provide continuity of care and foster long-term relationships with the patient, they are in a unique position to manage depression and should be familiar with the principles and modalities of treatment.
WHAT CAN I DO IN MY PRACTICE?
Be familiar with the principles and modalities of depression management
Management aims to achieve and maintain remission of symptoms as well as full functional recovery.(6) Treatment should be holistic, based on the biopsychosocial and lifestyle model;(7) this can include medication, psychological treatment (e.g. legitimising the illness and facilitating acceptance of the diagnosis), social treatment (e.g. helping the patient to deal with issues of stigma and discrimination, harnessing resources such as support groups and family members) and lifestyle changes (e.g. identifying and managing stressors, managing comorbidities such as substance misuse), as well as managing concomitant medical illnesses such as diabetes and hypertension.
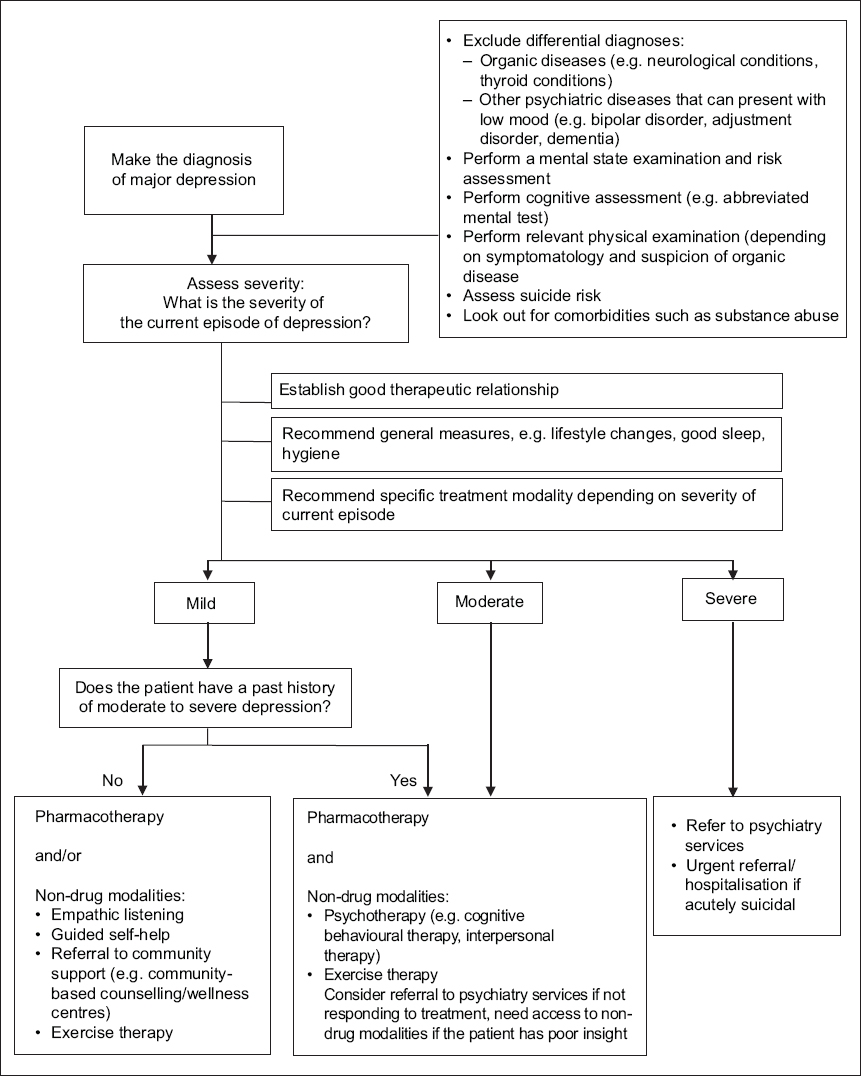
Various clinical guidelines are available to aid the primary care physician in managing patients with depression.(7-9) However, the primary care physician should also bear in mind that clinical guidelines serve as a guide and should not replace their own clinical judgment, and treatment should be individualised as much as possible to cater to the patient’s best interest. The algorithm in
Fig. 1
Flowchart shows approach to the treatment of depression in primary care.
Establish a therapeutic relationship with the patient
Regardless of the type of treatment modality chosen, the most central component is the quality of the therapeutic relationship between the primary care physician and the patient. A strong therapeutic relationship, along with empathic listening, has been shown to improve outcomes.(10,11) A therapeutic relationship starts from the first encounter with the patient, and should be patient-centred, open and non-judgemental, and involve active building of mutual respect and trust.(12) This is where the longitudinal relationship that family physicians often foster with their patients, even before their life events, creates an advantage. The respect and trust in the existing relationship aids in therapeutic recovery, while prior knowledge helps the physician to elicit the patient’s social background more easily.
Practical tips to foster good therapeutic relationships include the following:
-
Addressing the patient by their name, ensuring that the consultation setting is private and confidentiality is assured (within the limits of safety).
-
Addressing treatment expectations and concerns (especially with regards to medication safety, duration, side-effects and perceived risks of addiction) via psychoeducation in a validating, non-judgemental manner.
-
Addressing issues and myths regarding stigma and discrimination, especially in relation to the patient’s cultural beliefs. Some may be reluctant to accept the diagnosis or be on medication as they view depression to be a sign of weakness. In addition, legitimising depression as a chronic illness has been shown to increase the patient’s willingness to receive help.(13)
-
Exploring to locate possible interpersonal or psychosocial stressors. The consultation should not be rushed and the physician should not appear to dismiss the patient with quick solutions.
-
Seeking permission to involve family members or significant others in psychoeducation and treatment.
-
Being mindful of one’s own attitudes and beliefs that may influence the therapeutic alliance (countertransference).
General measures
Before considering more specific treatment modalities such as psychotherapy or medication, the primary care physician should advise on general measures such as lifestyle changes (healthy eating and exercise) and sleep hygiene.(14) Sleep hygiene is essentially establishing good sleep habits to promote good nighttime sleep and daytime alertness. Issues related to possible substance use disorders, such as smoking and alcohol use, should also be addressed. Exercise therapy, which can be done individually or in a group, has been shown to improve depression.(15) Exercise has additional health benefits beyond improving depressive symptoms.(16) Moderate-intensity exercise for a duration of at least 150 minutes per week is beneficial, and administering an exercise prescription is one way to encourage this.(17,18)
Psychotherapy options in primary care
Most patients with depression prefer non-pharmacological means of treatment instead of antidepressants, due to stigma, cost and the perceived risk of addiction and dependence.(19) In primary care, psychotherapy (also known as ‘talk therapy’) can be administered as first-line treatment or as an adjunct to antidepressants.(20) It has been proven to be as effective as antidepressants for patients with mild to moderate major depression;(20-22) however, many primary care physicians have minimal training in psychotherapy.(23) Patient selection is also important, as not all patients are suitable for psychotherapy. Suitable candidates are those who are able to assess and identify their own feelings, are motivated to change and improve, and can control their impulses.(24,25)
Psychotherapies that have been recommended for the treatment of depression include cognitive behavioural therapy (CBT),(21) interpersonal psychotherapy,(26) and problem-solving therapy.(27) Among these, CBT is considered as the first-line and most evidence-based psychological therapy for depression.(21) CBT works by identifying any dysfunctional thoughts and replacing them with more helpful ones, with the intent of modifying negative behaviours and emotions that perpetuate the depression.(28) For example, a person who is depressed might think: ‘She did not respond to me when I greeted her. It’s probably because she doesn’t like me.’ This negative thought would likely result in feelings of sadness, worry or rejection. As a result, the patient might start avoiding that friend in the future. CBT encourages the patient to think of alternative explanations (e.g. ‘She did not notice me, perhaps she is distracted or troubled. I should give her a call and find out how she is’) and partake in positive activities, such as meeting up with friends, which would lead to more positive outcomes. As CBT is not readily available in the primary care setting in Singapore, any patient who may benefit from it would need a referral to a clinical psychologist or tertiary setting where CBT is available. Understanding the importance of patient selection helps the primary care physician to make appropriate referrals.
Pharmacotherapy
For mild depression, psychotherapy and a review in two weeks’ time may be an option. However, antidepressants should be prescribed if there is no improvement following psychotherapy, the patient is unsuitable for psychotherapy, or the patient meets the criteria for moderate to severe depression. Features that support starting the patient on an antidepressant include more severe symptoms or a longer duration of symptoms.(6)
Table I
Side-effect profile and potential for drug interactions in commonly used antidepressants.(30,31,37-39)
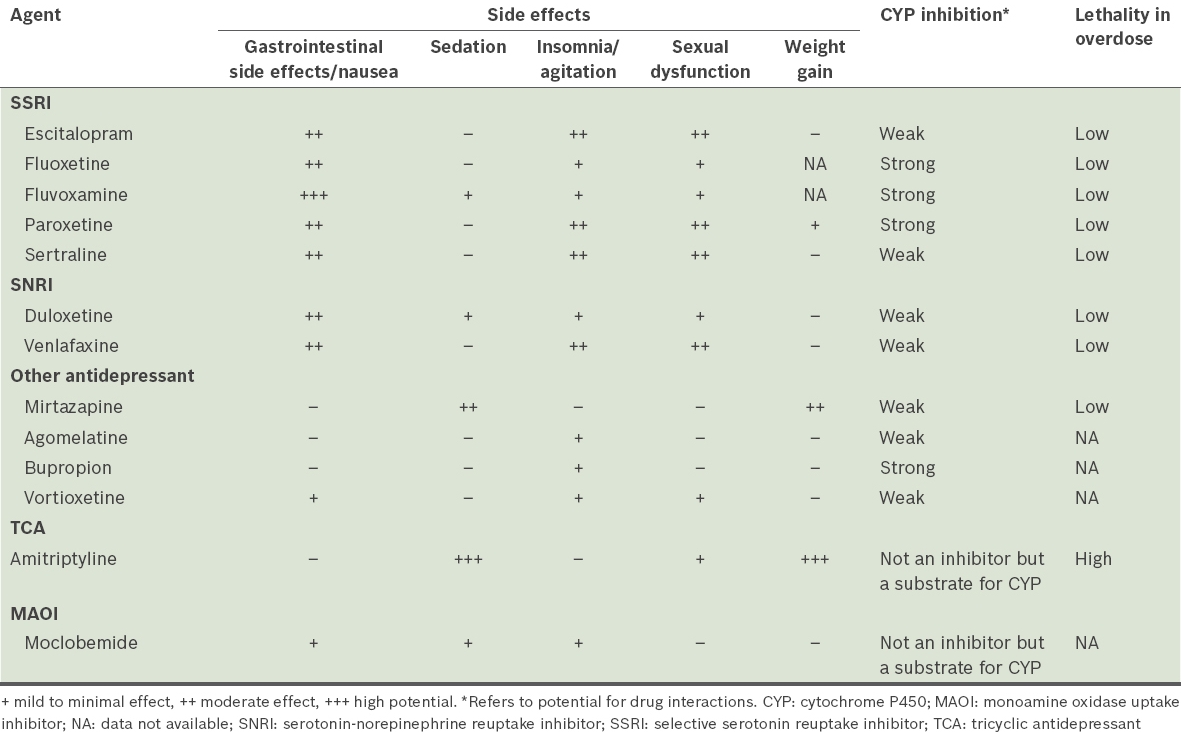
While there is little difference in terms of efficacy between the various classes of antidepressants, they differ in terms of potential for drug interaction as well as side effects such as sexual dysfunction, sedation or weight gain. Therefore, in choosing an antidepressant, the primary care physician should consider the side-effect profile of the medication, cost, the patient’s age, the presence of comorbid medical conditions, preference, past history or response/non-response to the antidepressant, current medications and potential drug-drug interactions, and the risk of lethality in overdose. In sum, the choice of antidepressant treatment should be individualised according to the patient’s needs.
First-line antidepressants include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, mirtazapine, bupropion, agomelatine and vortioxetine.(7,8,15) Other antidepressants such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are regarded as second-line and third-line, respectively, due to their tolerability and safety profile.(6) TCAs can cause anticholinergic effects (dry eyes, constipation and urinary hesitancy) and may be lethal if overdosed. MAOIs can lead to a hypertensive crisis if combined with tyramine-rich foods such as cheese and many medications, including common primary care drugs such as decongestants and cough syrups. Such drugs with high lethality in overdose should be avoided in persons with high suicide risk.(29)
SSRIs are commonly prescribed in primary care settings, as they are generally well tolerated and safe. Examples of SSRIs include sertraline, fluvoxamine, paroxetine, escitalopram and fluoxetine. The primary care physician should advise patients that SSRIs are commonly associated with nausea, vomiting and a potential worsening of anxiety, especially during the first week, which should resolve over time as the body adjusts to the medication. Short-term adjunctive benzodiazepines may be helpful during the initial week, but should be tapered off as soon as possible. Apart from their common gastrointestinal side effects, primary care physicians should also be aware that SSRIs may be associated with hyponatraemia and sexual dysfunction.
The potential for drug interaction is based on the inherent ability of the drug to inhibit cytochrome P450 (CYP) enzymes.(30,31) SSRIs such as fluoxetine, fluvoxamine and paroxetine have strong potential to inhibit CYP, which can lead to clinically significant interactions with other drugs. In contrast, escitalopram, sertraline and mirtazapine have little inhibitory effect on CYP,(31,32) and therefore can be considered in a patient who is on multiple other drugs. SSRIs are also associated with gastrointestinal bleeding.(33) As such, caution should be exercised when considering it in patients who are already on aspirin or warfarin therapy.(29)
In special populations, antidepressant therapy, if indicated, should be tailored according to individual requirements. Elderly patients should be prescribed antidepressants at much lower doses. As pregnancy is not an absolute contraindication for antidepressant therapy, it should be considered in pregnant patients, especially if the benefits far outweigh the risks. In such cases, recommended first-line antidepressants include escitalopram and sertraline, in view of their efficacy and safety profile.(8,15) For children and adolescents, the United States Food and Drug Administration requires a ‘black box’ warning (i.e. most serious type of warning) about the suicide risk associated with the use of antidepressants, but the benefits of antidepressants, when indicated, far outweigh the potential harm associated with treatment in children and adolescents.(34,35) In view of the many challenges related to the management of depression in these special groups, pregnant women and patients aged 18 years and below should be referred to tertiary services for further management.
The physician should inform the patient that while the adverse effects of antidepressants may manifest earlier, their onset of action is at least 2–4 weeks. Patients should also be informed that sudden cessation of antidepressant medication may result in discontinuation symptoms; these may manifest as flu-like symptoms, insomnia, nausea and hyperarousal,(36) and are not a sign of addiction. This is important to improve understanding and adherence to medication. Finally, before ending the consultation, the primary care physician should again assess the patient’s understanding of their condition; their antidepressant treatment in terms of its indication, expected duration, course of treatment, side-effect profile and dosing; and the importance of adherence to medication, as well as conducting a suicide risk assessment. Patients should be advised to make an earlier appointment if they are unable to tolerate their medication or their symptoms worsen.
Resources in the community
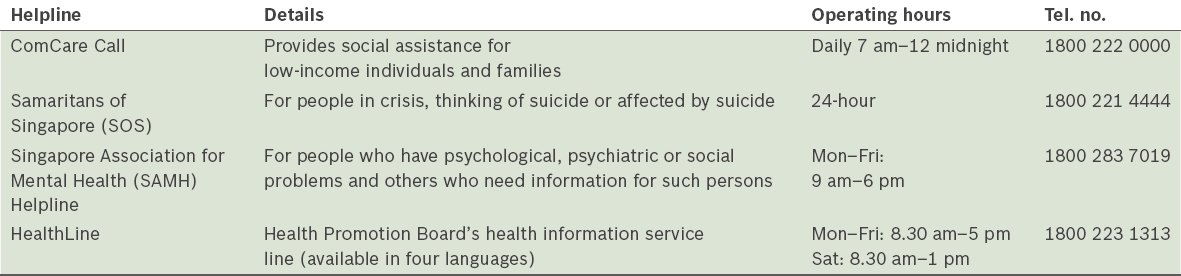
For holistic patient management, physicians can also tap on resources in the community to help support patients with depression and their caregivers. Presently, there are local peer support groups conducted by the Singapore Association for Mental Health and Institute for Mental Health (IMH). The group at IMH is a psychoeducation group in which patients can also learn about the depressive illness and methods of coping. Some helplines that can provide support for patients or caregivers are listed in
Table II
Helplines for patients in need.
Follow-up visits
Once an antidepressant has been selected, it may be started initially at a subtherapeutic dose to assess tolerability, after which the dose should be gradually increased until a minimally effective dose is achieved. The patient should be reviewed at two weeks after commencement of antidepressant medication,(29) or earlier if there is any concern of self-harm. During follow-up visits, the patient should be asked about drug tolerability and side effects, with dose adjustment if necessary. Progress should be assessed using measurement-based assessment tools, preferably those that are easy and inexpensive to use, such as the Patient Health Questionnaire-9, or PHQ-9.(40) The same tool should be used throughout the treatment duration to facilitate monitoring of progress.(6) Aspects to be monitored include adherence to medications, mood, vegetative symptoms and suicide risk. Accurate assessment of response to therapy is important because the dose of antidepressant should be increased if there is inadequate improvement, provided the drug is tolerable. In general, response to treatment is defined as a 50% decrease in scores on depression scales, while a non-response refers to a less than 25% decrease from baseline severity. A partial response would be somewhere in between. The patient is said to be in remission if signs and symptoms are absent in the current episode of depression and function is restored.(41) If the side effects are intolerable, the decision may be made to switch to a different antidepressant. The clinicians should wait approximately 2–4 weeks to assess symptomatic improvement and tolerability before deciding on a change of dose or switching to another agent.(6)
Upon achieving symptom remission, the dose of antidepressants should be maintained for at least 6–9 months for any patient with a first episode of depression. Hence, a typical treatment course would be approximately a year.(42) The patient should be advised that antidepressants are not addictive and that ‘the dose which gets you well, keeps you well’.(29,43) The likelihood of recurrence increases with the number of depressive episodes, with a recurrence rate of 50% after one episode(44) and 90% after three episodes.(45) A person who has a second episode of depression would require maintenance treatment at full therapeutic doses for 1–2 years, while anyone who has more than two episodes of depression would require lifelong or at least two years of maintenance therapy.(43) Apart from the number of depressive episodes, other factors associated with increased risk of relapse include the presence of comorbid conditions (psychiatric or chronic), having residual symptoms between episodes, and the presence of severe symptoms during episodes, such as suicidality, psychosis and severe functional impairment.(46)
WHEN SHOULD I REFER TO A SPECIALIST?
Patients should be referred to a psychiatrist for further management if the following conditions are present:(15,43,47)
-
Diagnostic difficulty
-
No improvement seen after one or two trials of medication, and augmentation/combination therapy or specialised treatment (such as electroconvulsive therapy) is indicated
-
Comorbid medical conditions giving rise to potential drug-drug interactions for which expertise is needed
-
Comorbid substance abuse
-
Psychotic symptoms
-
Risk of suicide
-
Pregnancy
-
Age < 18 years
TAKE HOME MESSAGES
-
Apart from using the specific treatment modalities of pharmacotherapy and psychotherapy, management of depression should be holistic and include managing stressors, putting the patient in touch with the community and other resources, dealing with stigma and discrimination, and managing concomitant comorbidities.
-
A strong therapeutic relationship between the primary care physician and the patient, along with empathic listening, has been shown to improve outcomes.
-
Psychotherapy or ‘talk therapy’ has been shown to be as effective as antidepressants for patients with mild to moderate major depression, but patient selection is important, as not all patients are suitable for this treatment modality.
-
CBT works by identifying any current dysfunctional thoughts and replacing them with more helpful ones, with the intent of modifying behaviour and emotion.
-
When selecting an initial antidepressant, the primary care physician should take into consideration the side-effect profile, the presence of comorbid conditions, concurrent medications and lethality in overdose.
-
Antidepressants should be started initially at a subtherapeutic dose to assess tolerability, after which the dose can be gradually increased until a minimally effective dose is achieved.
-
Accurate assessment of response to therapy is important because the dose of antidepressants should be increased if there is inadequate improvement, provided the drug is tolerable.
-
Upon achieving symptom remission, the dose of antidepressants should be maintained for a period to prevent relapse; the duration of maintenance therapy depends on the number of depressive episodes, the severity of the episodes and other factors.
-
The patient should be advised that antidepressants are not addictive and that ‘the dose which gets you well, keeps you well’.
-
The primary care physician should be cognisant of factors suggesting that a patient is unsuitable for management by primary care and needs to be referred to a psychiatrist.
Joseph accepted your assessment and was agreeable to being started on escitalopram for his depression. As he was also keen to explore psychotherapy as a treatment option, you referred him to the behavioural medicine department of a tertiary hospital. You also arranged for his mother to attend dementia daycare services. At his review two weeks later, you found out that Joseph was tolerating the medication well. A month later, he reported that his mood was better and that he had started psychotherapy sessions at the behavioural medicine department.
SMJ-58-466.pdf


