Mr Tan, a 39-year-old banker, visited your clinic complaining of difficulties in falling asleep. This started six months ago after he underwent an acrimonious divorce, and he was desperate for a permanent solution to his insomnia. He admitted to drinking half to one bottle of red wine every night with his dinner to help him relax after a long and stressful day at work. He also enjoyed drinking ‘a few’ nips of whiskey when socialising with his friends, about two to three times a month. Recently, he missed a day of work after having had a drinking session the night before and his boss had given him a stern warning. He denied having any low mood or anhedonia. He went to see you to take medical leave, as he felt too tired to concentrate on his work that day.
WHAT IS UNHEALTHY ALCOHOL USE?
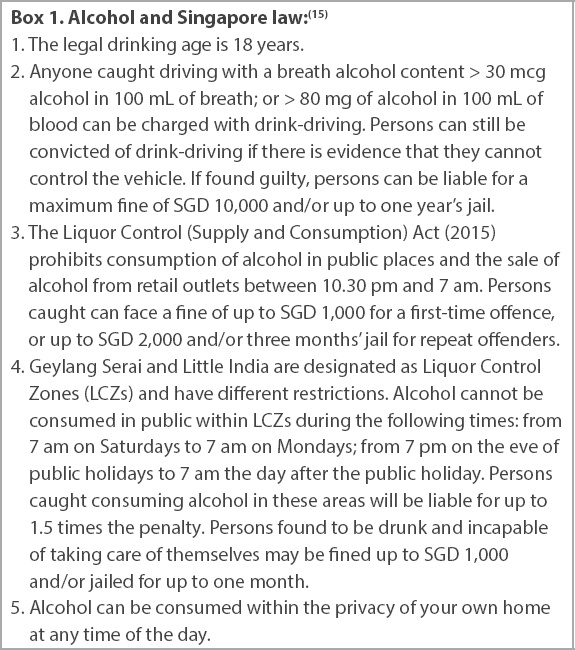
Unhealthy alcohol use is an umbrella term that encompasses a spectrum of behaviours, ranging from risky drinking to alcohol use disorder.(1) Risky alcohol use is defined as: binge drinking, heavy drinking, or any alcohol use by pregnant women or those under 21 years of age.(2) Alcohol use disorder is categorised by severity according to the number of criteria present (
Fig. 1
Flowchart shows the definition of unhealthy alcohol use.(3) DSM: Diagnostic and Statistical Manual of Mental Disorders
Local recommendations
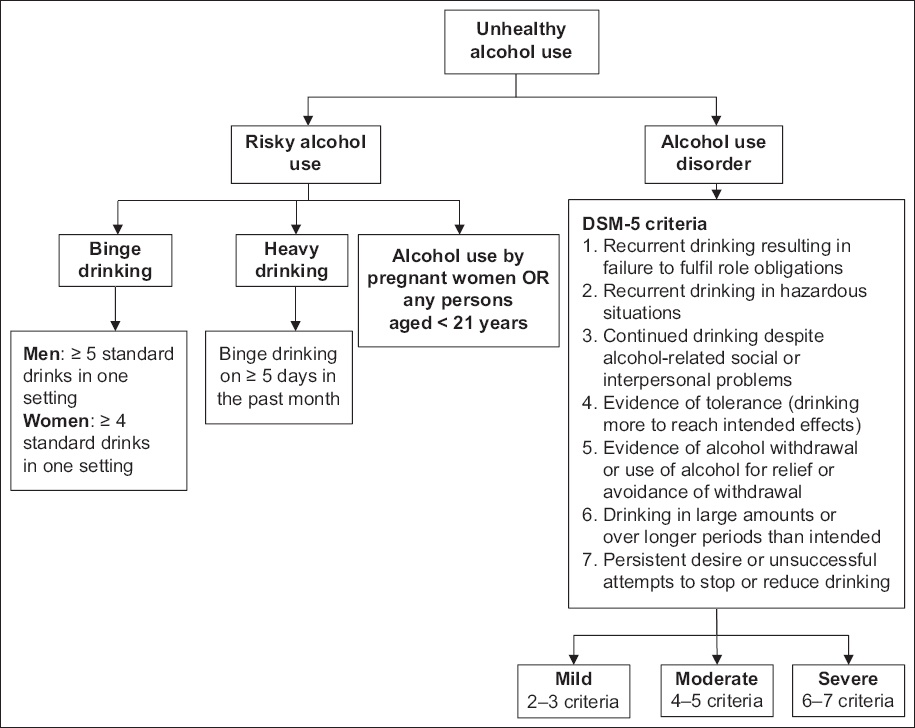
In Singapore, the maximum recommended alcohol intake is two standard drinks per day for men and one standard drink per day for women.(4) Definitions of a standard drink vary internationally. In Singapore, one standard drink is equivalent to 10 g of pure alcohol (
Fig. 2
Graphic shows examples of one standard drink in Singapore (10 g pure alcohol)
Another useful way of calculating alcohol intake is by using the following formula:(6) number of standard drinks = amount of drink (in litres) × alcohol by volume (%) × 0.789 (density of ethanol at room temperature). For example, for a 500-mL bottle of beer that is 5% alcohol by volume, the number of standard drinks it contains is: 0.5 × 5 × 0.789 = 1.97 standard drinks.
HOW COMMON IS THIS IN MY PRACTICE?
According to the Singapore Mental Health Study 2016, 4.1% and 0.5% of the population suffer from alcohol abuse and alcohol dependence, respectively, at some point in their lifetime. Those who were more likely to have alcohol use disorders were male, aged 18–34 years, of lower education attainment and employed. Among all people with a mental disorder who sought help, 20% presented to a general practitioner.(7)
The prevalence of binge drinking, in particular, is a rapidly growing problem, with a prevalence of 13.7% in 2016. Male and younger individuals (aged 18–34 years) were more likely to binge drink.(8) Underage drinking is also a problem, with a World Health Organization study from 2004 demonstrating that 73.5% of males and 64.5% of females aged 15–19 years drank alcohol.(9)
HOW RELEVANT IS THIS TO MY PRACTICE?
Alcohol use disorders are some of the most stigmatised mental health disorders in Singapore and, as such, patients rarely seek help for their condition.(10) Results from the Singapore Mental Health Study demonstrated that only 18.9% of people with alcohol use disorder had sought help in their lifetime.(11) Another study demonstrated that persons with alcohol use disorder, in particular alcohol dependence, had the highest 12-month treatment gap of all mental health disorders, at 97.1%. This is largely due to the individual’s failure to perceive the need for treatment.(10)
This highlights the important role that primary care physicians have to play in identifying vulnerable persons at risk for alcohol use disorder. Epidemiological studies have demonstrated a strong association between unhealthy alcohol use and certain physical and medical conditions, such as hypertension, heartburn, gastric ulcers, anaemia, abnormal liver enzyme levels and chronic pain syndromes, as well as major depressive disorder, insomnia, and problems in social life or at work.(1,11) Screening for alcohol use disorders in these groups of patients will aid detection and earlier treatment initiation at the primary care level.
WHAT CAN I DO IN MY PRACTICE?
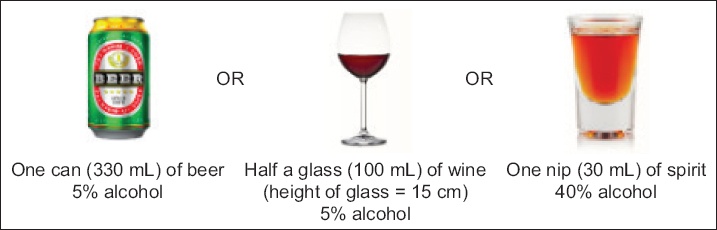
Screening
Table I
Screening tools that can be used in primary care.
Clinical history and physical examination
Following a positive screening test, it is important to quantify alcohol use (
Fig. 3
Flowchart shows the approach to unhealthy alcohol use. AUDIT-C: Alcohol Use Disorders Identification Test-Concise; SASQ: Single Alcohol Screening Question
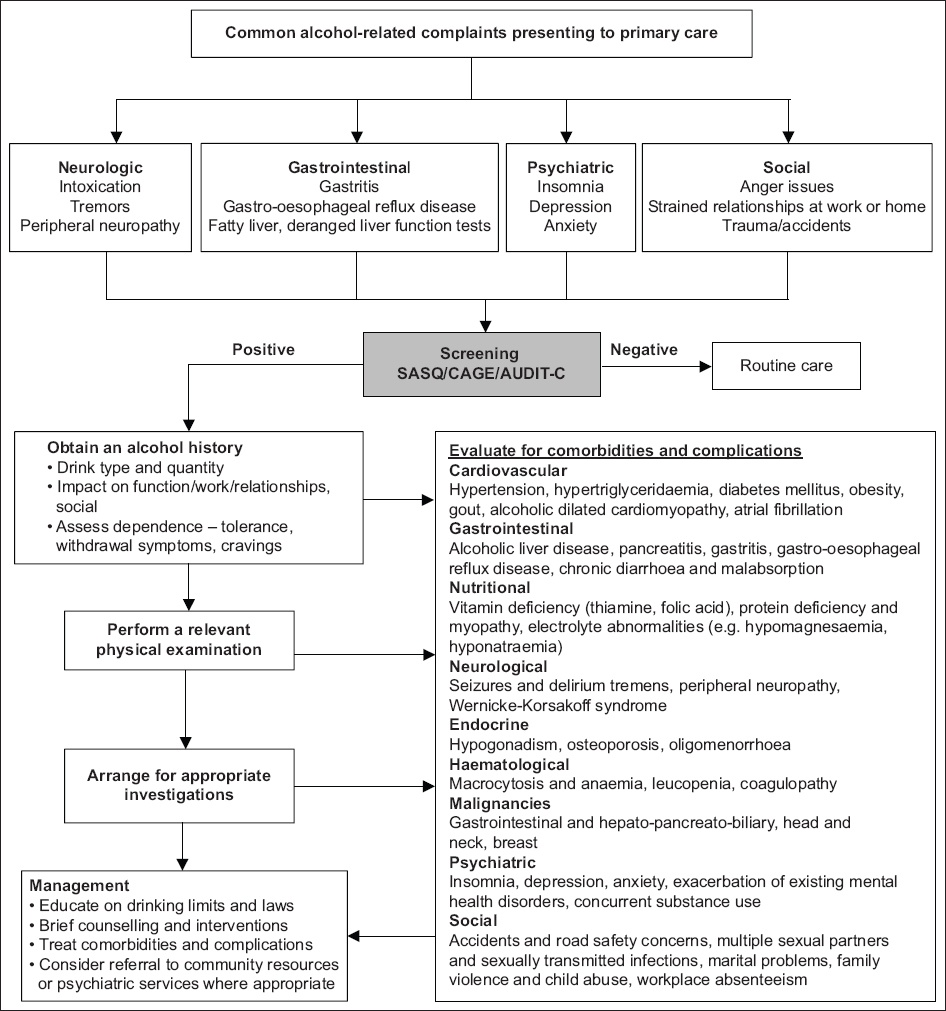
It is important to acknowledge the significant impact of physicians’ attitudes, knowledge and perception in eliciting this information. Open and non-judgemental attitudes are vital in encouraging patient disclosure.
A review of the patient’s past medical history, along with a targeted systems review should be done to evaluate for physical and mental health complications of alcohol use disorder. Concurrent substance use, such as cigarettes and recreational drugs, should be screened for.
Clinicians should be mindful of alcohol withdrawal in higher-risk patients, which usually occurs after a drastic reduction in chronic alcohol drinking and within 6–24 hours of the last drink. Symptoms include anxiety, agitation, restlessness, tremors, insomnia, diaphoresis, palpitations, headache and alcohol craving. Patients may also experience nausea, vomiting and loss of appetite. Manifestations of severe withdrawal are hallucinations, seizures and delirium tremens.(14) A thorough physical examination, mental state examination and risk assessment should be performed. If deemed necessary, a suicide risk assessment should be performed in those with severe psychiatric comorbidities.
Special populations
As there is no known safe level of alcohol consumption during pregnancy, alcohol should not be consumed in any quantity by pregnant women or women who are trying to get pregnant. Alcohol is teratogenic and also increases the risk of pregnancy loss.(1) It is important to screen all pregnant women for alcohol consumption and counsel them appropriately.
Laboratory investigations
Investigations are useful to detect complications of alcohol use disorder. These include:
- Full blood count (to look for macrocytosis)
- Liver function tests (aspartate aminotransferase:alanine aminotransferase ratio of 2:1 suggests alcoholic liver disease)
- Gamma-glutamyl transferase (elevated in one-third of heavy drinkers)
- Electrocardiography
Carbohydrate-deficient transferrin is a more specific marker of chronic excessive alcohol use, although it is only available in specialist settings. In the inpatient setting, serum electrolytes (including sodium, potassium, magnesium and phosphate) should be checked, along with amylase, lipase and urine drug testing.
Management: brief counselling and interventions
We should educate all patients on their alcohol limits and advocate having at least 2–3 drink-free days per week. If any patient is contemplating reduction of his alcohol intake, motivational interviewing techniques can be used for brief intervention. For example:
- “Would you like to hear more about what drinking does to you, and how to cut back?”
- “What have you tried before?”
- “What do you think are the good and not so good things about stopping drinking?”
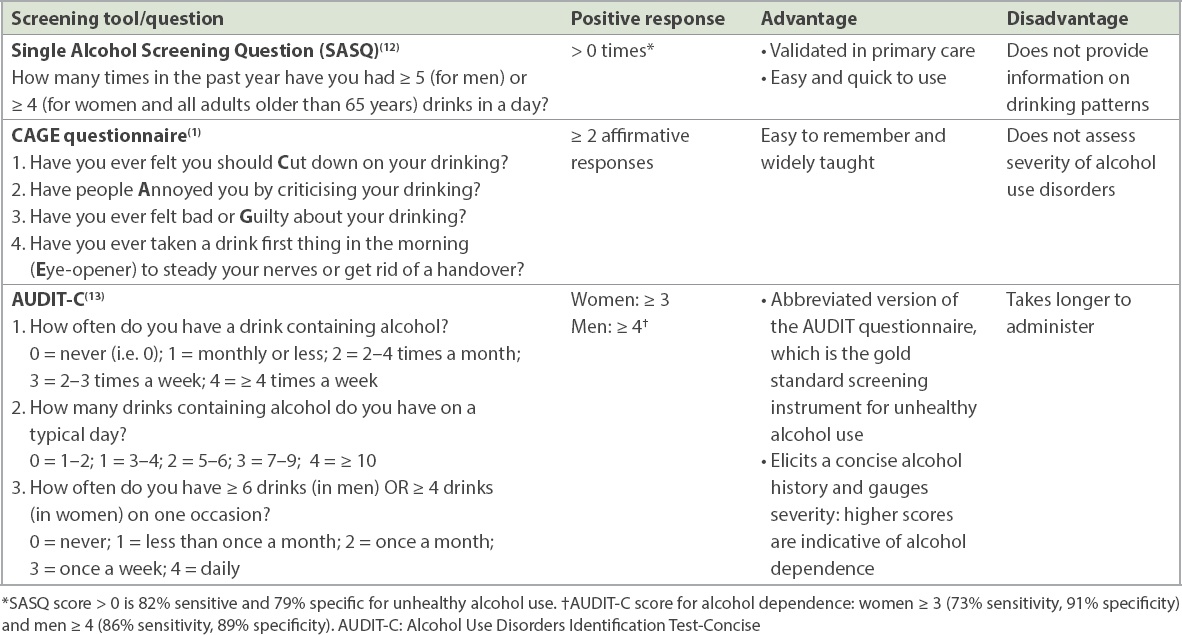
To maintain rapport, efforts should be made to ensure continuity of care, with the same physician seeing the patient at all subsequent visits. Doctors should also keep up to date on the relevant laws related to alcohol use in Singapore (
WHEN SHOULD I REFER TO A SPECIALIST?
Patients with mild alcohol use disorder can be safely managed in the community. Brief counselling and interventions, with close follow-up, may be sufficient for most of these patients. There are various resources that can provide further support for motivated individuals or those whose drinking is starting to affect their work or social lives (
Table II
Community resources and helplines.
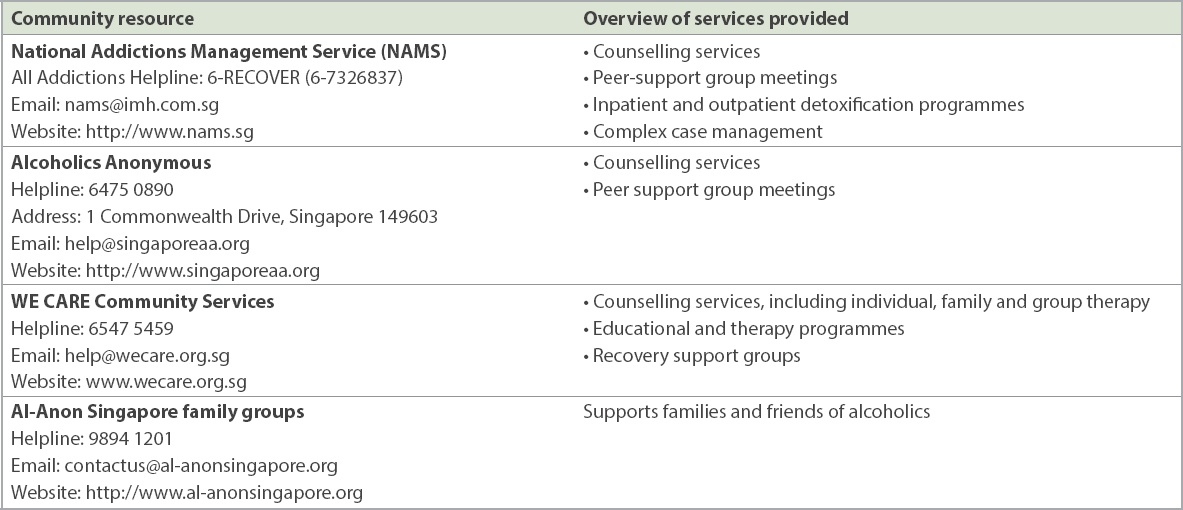
Patients with moderate to severe alcohol use disorder can be referred to specialist psychiatric clinics for consideration of medication-assisted detoxification therapy. Patients with concurrent psychiatric comorbidities and those with a history of recurrent failed detoxification attempts or delirium tremens should also be referred to specialist clinics. These are primarily based at the National Addictions Management Service (NAMS) within the Institute for Mental Health. NAMS also runs satellite Community Wellness Clinics at Geylang and Queenstown Polyclinics. There are also psychiatrists who run alcohol cessation services within National University Hospital and Changi General Hospital.
Patients with severe physical or psychiatric complications from alcohol use disorder should be referred to the emergency department for stabilisation. Those at high risk of harm to self or others and those with a lack of social support should also be referred for their safety.
TAKE HOME MESSAGES
-
Unhealthy alcohol use is a growing problem in Singapore, with the prevalence of alcohol use disorder and binge drinking steadily increasing in the last decade.
-
The recommended maximum alcohol intake is two standard drinks per day for men and one standard drink per day for women.
-
All at-risk adults should be screened for unhealthy alcohol use, using simple screening tools such as the Single Alcohol Screening Question, CAGE questionnaire or AUDIT-C.
-
Those who screen positive should undergo further assessment for alcohol use disorder, other substance abuse, and medical/psychiatric comorbidities and complications.
-
Laboratory investigations may be helpful as an adjunct to determine the severity of alcohol use disorder.
-
Primary care physicians have an important role in assessing risk and can also provide counselling and intervention. A therapeutic doctor-patient relationship can be fostered if efforts are made to ensure continuity of care.
-
Motivated individuals with alcohol use disorder can be referred to several community resources for more comprehensive management. Those assessed to be at higher risk for alcohol withdrawal syndromes should be referred to specialist psychiatric services for medication-assisted treatment.
You quickly found that Mr Tan screened positive on the Single Alcohol Screening Question. After further history-taking, you diagnosed him with mild alcohol use disorder. He had been using alcohol to cope with stress from work and his ongoing divorce proceedings. He had not realised that he had been drinking excessively until he met you and was open to accepting help. Apart from a borderline high blood pressure of 146/94 mmHg, his physical examination was unremarkable. There were no features of alcohol withdrawal. He agreed to do basic laboratory investigations (full blood count, liver function tests and gamma-glutamyl transferase) and to return to see you next week to review his blood test results. In the meantime, he decided to sign up for the next Alcoholics Anonymous meeting to help him address his drinking problem.
SMJ-62-74.pdf