Abstract
INTRODUCTION
The uncinate process (UP) has an important role because of its relationship with the vertebral artery and spinal roots. Degenerative diseases cause osteophyte formation on the UP, leading to radiculopathy, myelopathy and vertebral vascular insufficiency, which may require surgical management. This study aimed to evaluate the morphometry of this region to shed light on the anatomy of the UP.
METHODS
Morphometric data was obtained from 13 male formaldehyde-fixed cadavers. Direct measurements were obtained using a metal caliper. Computed tomography (CT) morphometry was performed with the cadavers in the supine position.
RESULTS
Direct cadaveric measurements showed that the height of the UP increased from C3 (5.8 ± 1.0 mm) to C7 (6.6 ± 0.5 mm). On CT, the corresponding measurements were 5.9 ± 1.2 mm at C3 and 6.9 ± 0.6 mm at C7. The distance between the left and right apex of the UP from C3 to C7 also increased on both direct cadaveric and CT measurements (C3: 20.8 ± 1.0 mm and C7: 28.1 ± 2.4 mm vs. C3: 23.7 ± 3.4 mm and C7: 29.0 ± 3.0 mm, respectively). On CT, the distance between the UP and superior articular process at the C3 to C7 levels were 9.8 ± 1.7 mm, 7.9 ± 1.8 mm, 7.9 ± 1.6 mm, 7.8 ± 1.3 mm and 8.2 ± 1.7 mm, respectively.
CONCLUSION
Direct cadaveric and CT measurements of the UP are useful for preoperative evaluation of the cervical spine and may lead to better surgical outcomes.
INTRODUCTION
The uncinate process (UP) is located on the superior surfaces of the third to seventh cervical vertebral bodies (i.e. C3–C7) and the first thoracic vertebra. According to Pait et al,(1) the UP was first identified in 1858 by Luschka, who named it ‘eminentia costaria’ because it resembles the head of a rudimentary rib; Trolard introduced the current, widely used term, ‘processus uncinatus’ (Latin for uncinate process) in 1893. The function of the UP is said to be protective, as it restricts lateral flexion.(1)
The UP is located close to the vertebral artery, radicular artery and spinal nerve roots. The development of osteophytes on the UP, which may be due to some degenerative diseases, could result in increased pressure on neurovascular structures that are in close proximity to the UP. For instance, osteophytes arising from the UP vertebra may interfere with the transverse foramen, leading to compression of the vertebral artery.(2) Pathologies such as radiculopathy, myelopathy and vertebral vascular insufficiency may occur due to the formation of UP osteophytes.(2-4) To treat these conditions, uncoforaminectomy and corpectomy via the anterolateral or anteromedial approach may be necessary.(4-6) As the UP is a very important area in osteophyte resection, corpectomy and cervical surgery for decompression, knowledge of its morphometry is crucial to surgeons.
Although several studies have been conducted on the UP based on the analysis of dry bone materials,(7-9) to the best of our knowledge, none used direct cadaveric measurements to evaluate the UP. The present study aimed to assess the anatomy of the UP and vertebral body via direct measurement of cadavers and angiographic computed tomography (CT). Using the aforementioned methods, the unity of vertebrae is not destroyed, thus ensuring that the bone materials measured are from the same cadaver.
METHODS
A total of 13 adult, male formaldehyde-fixed cadavers were obtained from the Department of Anatomy, School of Medicine, Dokuz Eylül University, Turkey. The vertebral arteries of the cadavers were washed with water and filled with barium and coloured silicone mixture. Angiographic CT of the vertebral arteries was conducted at the institution’s angiography unit in the Department of Radiodiagnostics.
A multislice CT scanner (Mx8000 Multislice System; Philips, Amsterdam, Netherland) was used. The cadavers were placed in the supine position and imaging was performed in the transverse plane. The following parameters were used during imaging: 1.3 mm slice thickness; 0.6 mm increment; 1.250 pitch; 0.75 s rotating time; 120 kV power; 240 mAs/slice; 180° scanning angle; and 512 acquisition matrix. The scanning area was between the upper level of the C2 vertebra and the lower level of the C7 vertebra. The mean scan time was 40 seconds. On completion, the imaging data was transferred to a picture archiving and communication system (PACS). Both the sagittal and coronal reformatted images (
Fig. 1
(a) CT angiography image (reconstructed coronal slice view) shows the anterior view of the cervical spine and the vertebral artery. (b) Photograph shows the decapitated prevertebral and paravertebral tissues of a dissected cadaver, as well as the coloured silicon injected into the vertebral arteries. IVD: intervertebral disc; UP: uncinate process; VA: V2 segment of the vertebral artery; VB: vertebral body
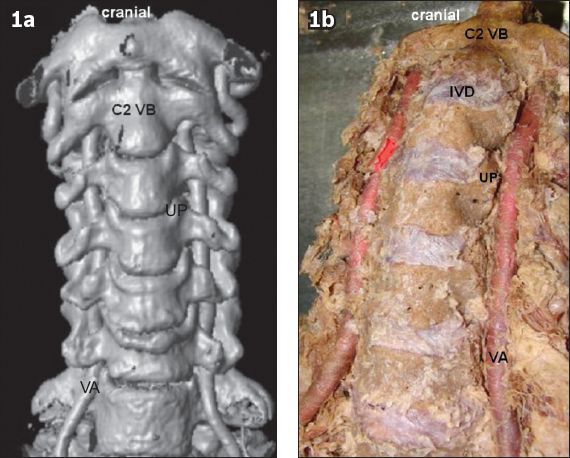
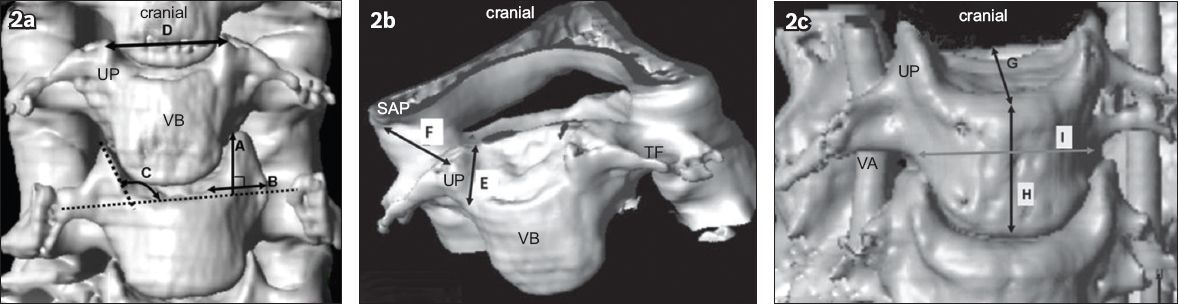
Fig. 2
(a–c) CT angiography images (reconstructed coronal slice view) show the parameters measured in the present study. A: uncinate process (UP) height, i.e. distance on the vertebra anterior between the endplate and the apex of the UP; B: width of the UP; C: angle between the UP and vertebral body (VB) endplate (the angle on the anterior vertebra between the endplate and medial side of the UP); D: anterior distance between the right and left apex of the UP; E: length of the medial border of the UP on the VB; F: distance between the UP apex and lateral side of the superior articular process (SAP); G: anteroposterior diameter of the VB (the distance between the front and back points in the middle of the superior VB); H: anterior height of the VB (the vertical distance between the midpoint of the VB on the superior and inferior side); I: width of the VB (the horizontal distance between the right and left attachment points of the transverse processes on the VB); TF: transverse foramen; VA: vertebral artery
RESULTS
We observed that the height of the UP increased from the C3 to C7 level in both direct cadaveric and CT measurements (
Table I
Measurements made at the uncovertebral region of 13 cadavers.
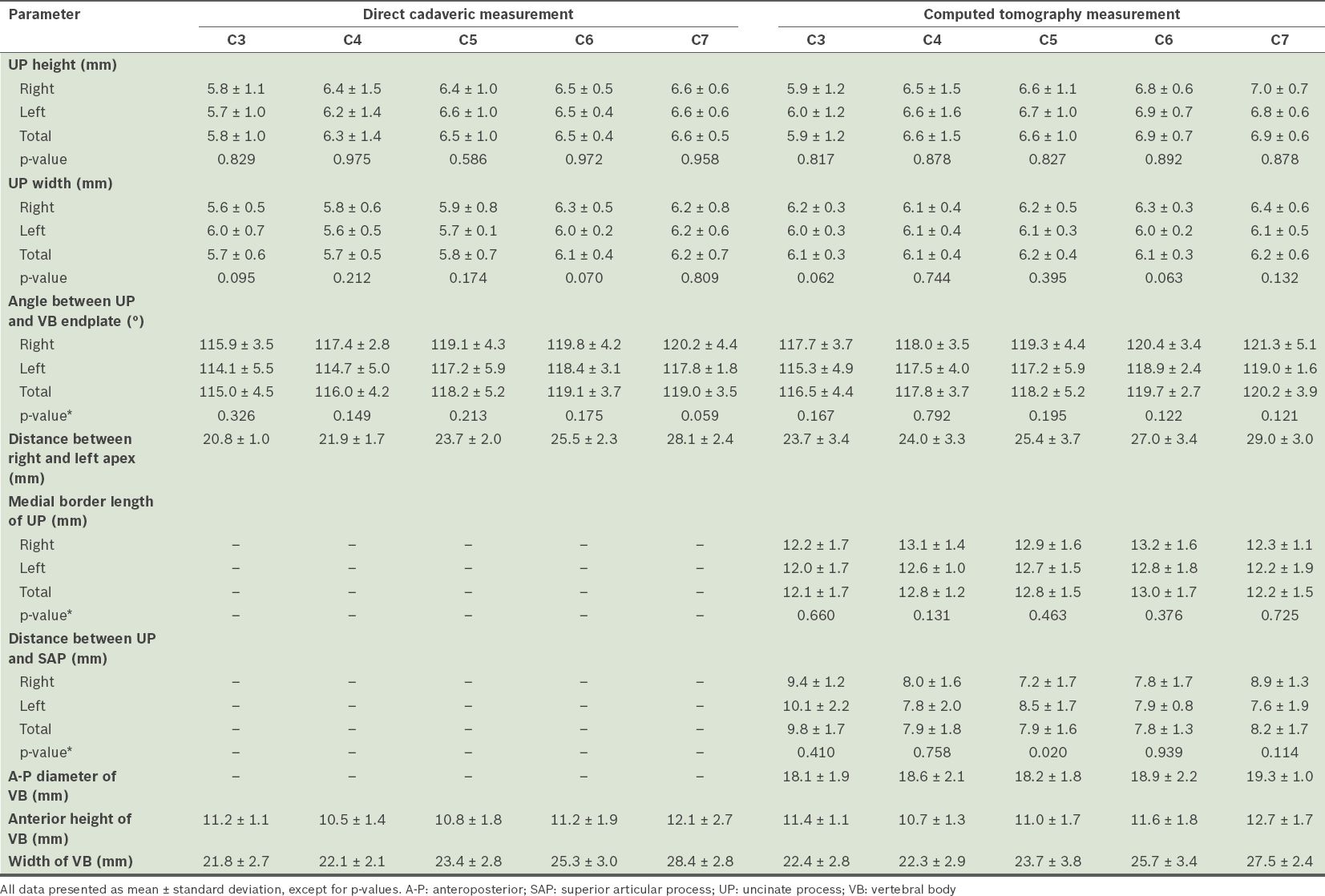
The angle between the UP and vertebral body endplate also increased from C3 to C7 on both direct cadaveric and CT measurements (C3: 115.0° ± 4.5° and C7: 119.0° ± 3.5° vs. C3: 116.5° ± 4.4° and C7: 120.2° ± 3.9°, respectively). The distance between the right and left apex of the UP using direct cadaveric measurements at C3 and C7 was 20.8 ± 1.0 mm and 28.1 ± 2.4 mm, respectively, while the corresponding measurements using CT were 23.7 ± 3.4 mm and 29.0 ± 3.0 mm, respectively. Again, the measurements showed an increase from the C3 to C7 level.
The length of the medial border of the UP, and the distance between the UP and the superior articular process were measured using CT only. The maximum measurement for the length of the medial border of the UP was obtained at C6 and the minimum at C3 (C3: 12.1 ± 1.7 mm; C4: 12.8 ± 1.2 mm; C5: 12.8 ± 1.5 mm; C6: 13.0 ± 1.7 mm; and C7: 12.2 ± 1.5 mm), with no significant differences between the measurements on the right and left sides (p > 0.05). For the distance between the UP and superior articular process, the maximum distance was measured at C3 (9.8 ± 1.7 mm), while the minimum was measured at C6 (7.8 ± 1.3 mm).
On CT, the anteroposterior diameter of the vertebral body was at its minimum at C3 (18.1 ± 1.9 mm) and maximum at C7 (19.3 ± 1.0 mm). The anterior height of the vertebral body was at its minimum at C4 and maximum at C7 on both direct cadaveric and CT measurements (C4: 10.5 ± 1.4 mm and C7: 12.1 ± 2.7 mm vs. C4: 10.7 ± 1.3 mm and C7: 12.7 ± 1.7 mm, respectively). Similarly, the width of the vertebral body increased from C3 to C7 on direct cadaveric and CT measurements (C3: 21.8 ± 2.7 mm and C7: 28.4 ± 2.8 mm vs. C3: 22.4 ± 2.8 mm and C7: 27.5 ± 2.4 mm, respectively).
There were no significant differences between all measurements related to the UP from C3 to C7 on the right and left sides, for both direct cadaveric and CT measurements (p > 0.05;
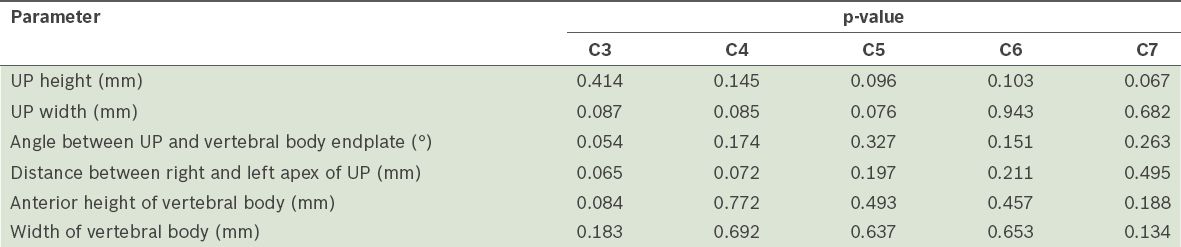
Table II
Results of paired samples t-test comparing the measurements of the uncinate process (UP) using the direct cadaveric method and computed tomography.
DISCUSSION
Knowledge of the boundaries of the UP is important for good surgical outcomes. Patients with cervical radiculopathy require anterior or anterolateral decompression via the removal of the uncovertebral joints and bone spur. Researchers have shown that excessive decompression of the UP increases the risk of cervical instability.(8) Thus, in order for the surgery to be minimally invasive and to achieve sufficient decompression, surgeons should be aware of the morphology and morphometry of the UP;(9,10) it borders the lateral line of the intervertebral disc. Tubbs et al(3) did not regard uncovertebral joints as synovial joints; the UP was regarded as a product of the formation of fibrocartilage and new bone due to reactive osteogenesis and degeneration, i.e. new bone formation was seen as a response to ageing.(3)
Compression of the posterolateral disc or UP is the most common cause of spinal nerve root compression.(7) Osteophytes can result in radiculopathy, myelopathy and vertebral vascular insufficiency due to their anatomical relationship with the spinal nerve roots, vertebral artery and spinal cord.(2,5) To treat these pathologies, uncoforaminectomy, decompressive surgery or osteophyte resection may be necessary.(2,6,8) However, foraminotomy and uncovertebral joint resection procedures may also cause vertebral artery injury,(11-16) possibly leading to ischaemic neurological pathologies.(17,18) Vertebral artery injury usually occurs following the use of a high-speed drill for lateral decompression, aggressive discectomy or decompression of bony tissues. Infection or tumour invasion of the lateral part of the spinal canal may also cause vertebral artery injury during surgery.
Although there is a very short distance between the UP and the medial border of the vertebral artery, the medial borders of the UP and the uncovertebral joints are referred to as safety zones for surgical procedures.(11,15) The vertebral artery and nerve roots are surrounded by a fibroligamentous band in the intertransverse area. The fibroligamentous tissue, which is laterally attached to the anterior border of both the vertebral artery and spinal nerve root, may stick to the high-speed drill and cause vertebral artery laceration. For this reason, this tissue must be dissected completely before resection.(11,16,19,20) Cervical spondylosis also narrows the foramen, making surgery more challenging in patients with this pathology.(11,19,21)
Some authors refer to the line between the UP and the medial border of the uncovertebral joint as a safety line, although the short distance between the UP and vertebral artery reduces the safety of surgery.(1,22) Once an uncovertebral joint is encountered, there is less than 6 mm to the medial margin of the transverse foramen.(23) It is important to take note of this distance when drilling the UP, so as to prevent vertebral artery injury. The vertebral artery or spinal nerve root injury is a very serious complication of surgeries performed with an anterior cervical approach.(5,8,23) For patients who have spondylolisthesis, the distance between the UP and the medial border of the transverse foramen is narrower than that of a healthy person.(2,23)
In a study conducted by Russo et al,(24) the distances between the medial border of the vertebral artery and the UP were as follows: C2–3 level left: 3.2 ± 1.0 mm, right: 3.5 ± 0.6 mm; C3–4 level left: 1.3 ± 0.6 mm, right: 1.1 ± 0.4 mm; C4–5 level left: 1.7 ± 0.9 mm, right: 1.6 ± 1.0 mm; C5–6 level left: 1.2 ± 0.8 mm, right: 1.1 ± 1.2 mm).(24) In our previous study, which was conducted on angiographic images of cadavers, the corresponding distances were as follows: C3: 1.8 ± 1.3 mm; C4: 2.4 ± 1.0 mm; C5: 2.5 ± 1.0 mm; and C6: 2.1 ± 1.2 mm.(12) In another study, we repeated the process using direct cadaveric and CT measurements, and found that the distance between the medial and lateral margin of the UP gradually increased from C3 to C7 (direct C3: 1.6 ± 0.2 mm, C4: 1.7 ± 0.2 mm, C5: 1.6 ± 0.4 mm, C6: 1.6 ± 0.4 mm vs. CT C3: 1.7 ± 0.3 mm, C4: 1.8 ± 0.3 mm, C5: 1.6 ± 0.4 mm, C6: 1.6 ± 0.5 mm),(13) as was found in the present study.
The height and width of the UP may be considered as the entrance to the spinal nerve and vertebral artery for decompression of the intervertebral foramen anterolaterally.(2,25) The UP is an important bone landmark that becomes larger and flatter as individuals get older, losing its sharp and bony characteristics.(8) In the present study, we found that in both direct cadaveric and CT measurements, the height of the UP increased from C3 to C7 (i.e. C3: 5.8 ± 1.0 mm, C7: 6.6 ± 0.5 mm vs. C3: 5.9 ± 1.2 mm, C7: 6.9 ± 0.6 mm). There were no significant differences between the measurements made via the two methods (p > 0.05;
Pait et al(1) and Bozbuğa et al(7) found that the height of the UP increased from C3 to C7, with the greatest height noted at the C6 level (
Table III
Results of studies conducted on the anatomy of the uncinate process (UP).
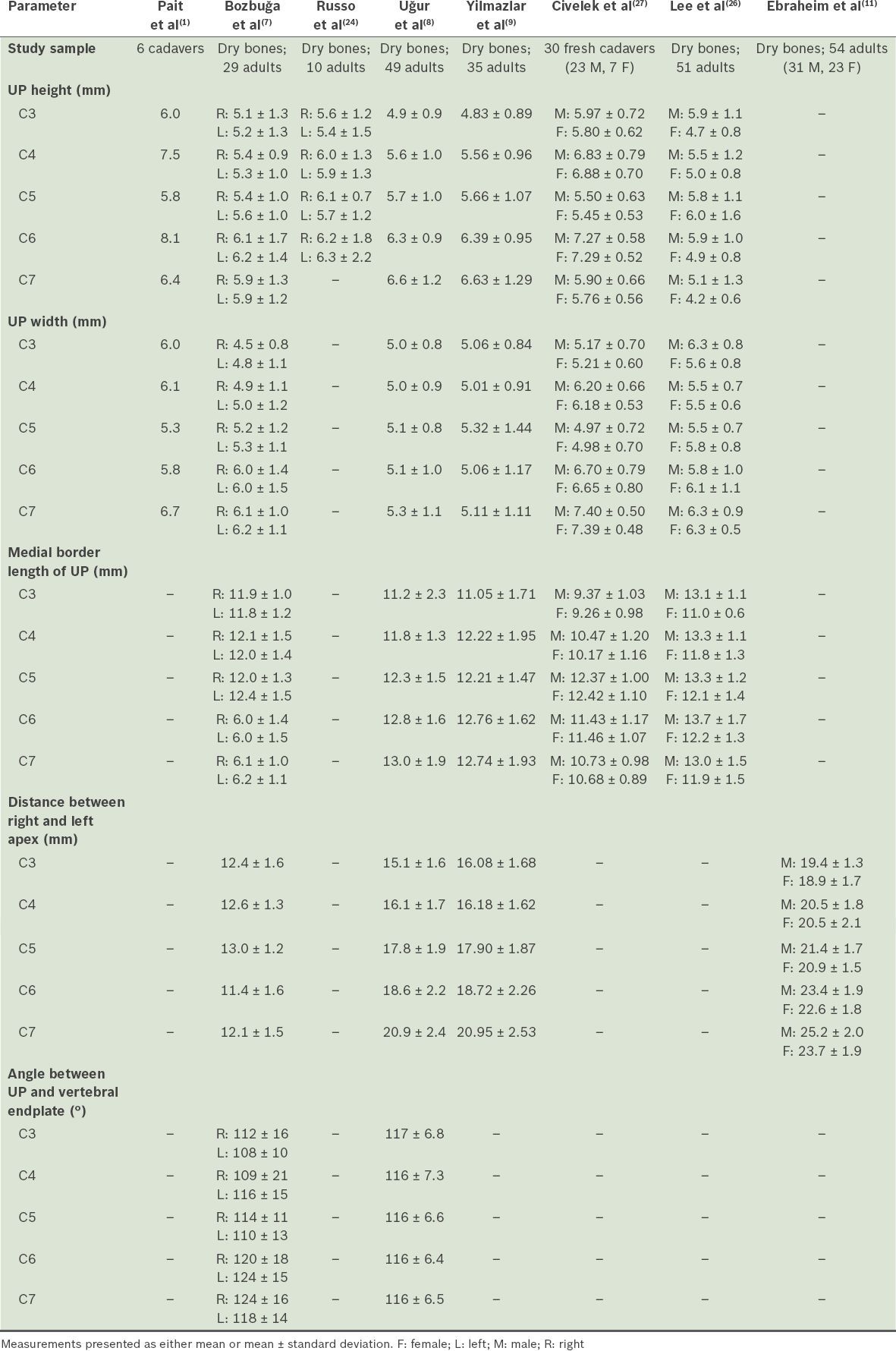
Knowledge of the width of the UP is also important when decompressing nerve roots posterolaterally. Lee et al found that the mean values for the width of the UP in men ranged from 5.5 mm (at C4 and C5) to 6.3 mm (at C3 and C7), and in women, from 5.8 mm (at C5) to 6.3 mm (at C7); the width of the UP was widest at C7 and narrowest at C5.(26) In the study by Civelek et al,(27) the measured width of the UP was 5.17 ± 0.70 mm at C3, 6.20 ± 0.66 mm at C4, 4.97 ± 0.72 mm at C5, 6.70 ± 0.79 mm at C6, and 7.40 ± 0.50 mm at C7 (
The UP lies posterolaterally at C6 and C7 and laterally at C3 and C5. It has a course from lateral to medial obliquely and front to back anatomically.(7) The distance between the right and left apex of the UP increases from C3 to C7. At different cervical levels, the surgical method may be changed.(20) As the UP forms the lateral border of a corpectomy, knowledge of the distance between the right and left apex of the UP is important, so as to determine the width of the UP during corpectomy. The distance between the right and left apex of the UP decreases gradually from C6 to C3.(7,8,12,14,20) The width of the vertebral body is smaller in the vertebral endplate than the distance between the right and left apex of the UP at the same level, and accordingly, the angle between the UP medial side and vertebral body upper side is an obtuse angle. The distance between the right and left apex of the UP, vertebral body width and angle between the UP medial side and vertebral body upper side increases from C3 to C7. The results of the present study are supported by those of other studies found in the literature (
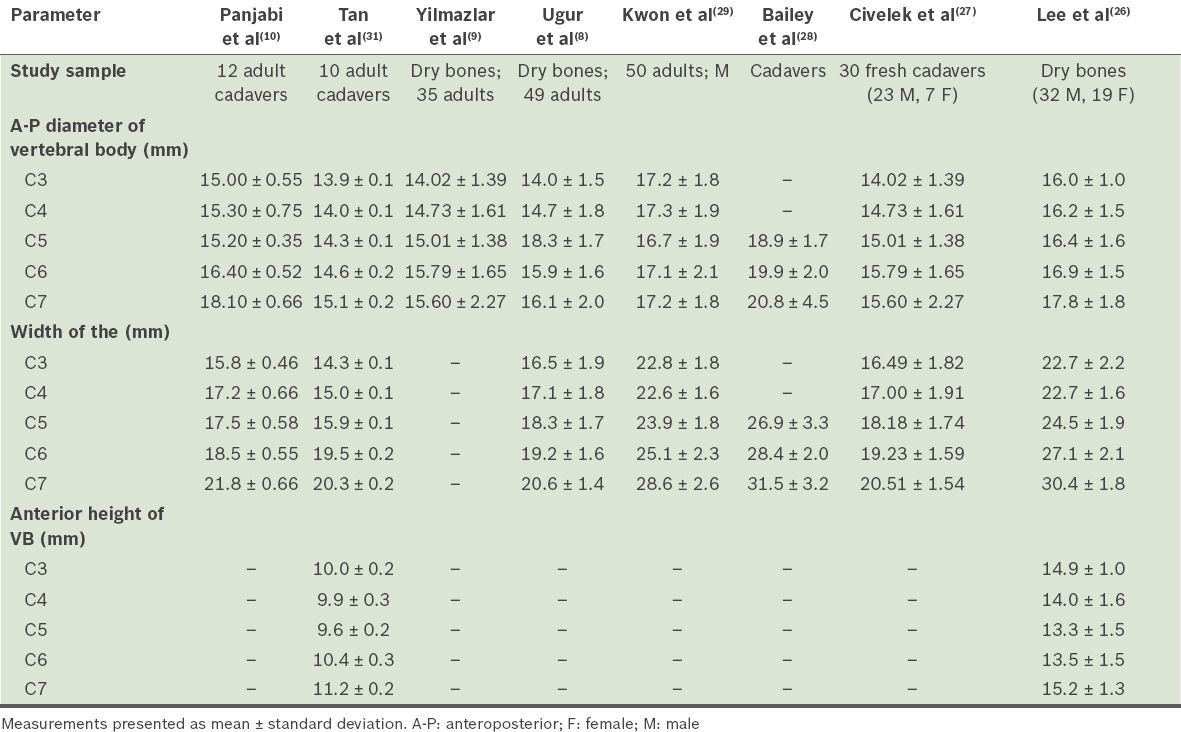
In the present study, the anteroposterior diameter of the vertebral body gradually increases from C3 to C7. It is approximately 6 mm longer than the medial border length of the UP at the same level. While the anteroposterior diameters of the vertebral body measured on dry bone vertebrae in the studies by Uğur et al(8) and Yilmazlar et al(9) were smaller than those in the present study, the corresponding diameters on CT measurement in studies by Bailey et al(28) and Kwon et al(29) were similar to the values found in the present study (
Table IV
Results of studies conducted on the vertebral body (VB).
The vertebral artery travels closer to the UP at the mid-cervical region than at the lower cervical regions.(20) Vertebral artery compression due to osteophytes may occur anteriorly from the UP or posteriorly from the superior or inferior articular facet. In most cases, compression is likely to occur from the UP rather than the articular facets, as osteophytes are present in 48% of UPs and only 30% of articular facets.(30) In the present study, the distance between the UP and the lateral side of the superior articular process on CT measurements was the greatest at C3 (9.8 ± 1.7 mm) and the smallest at C6 (7.8 ± 1.3 mm). The distance between the lateral side of the superior articular process and the UP apex in the posterior and lateral aspects is important for orientation, in terms of defining the region where the vertebral artery and spinal nerve root exists. One study suggested the removal of the medial side of the superior articular process during UP localised osteophyte resection, especially at the C5, C6 and C7 levels.(8)
Panjabi et al(10) made measurements directly on 12 adult cadavers and found the posterior height of the vertebral body to be 11.6 ± 0.35 mm at C3, 11.4 ± 0.43 mm at C4, 11.4 ± 0.32 mm at C5, 10.9 ± 0.26 mm at C6 and 12.8 ± 0.46 mm at C7. In the study by Tan et al(31) conducted on ten cadavers of Singapore Chinese origin, the posterior height of the vertebral body was 11.2 ± 0.1 mm at C3, 11.3 ± 0.2 mm at C4, 11.3 ± 0.1 mm at C5, 11.3 ± 0.2 mm at C6 and 11.8 ± 0.3 mm at C7. The anterior height of the vertebral body was 10.0 ± 0.2 mm at C3, 9.9 ± 0.3 mm at C4, 9.6 ± 0.2 mm at C5, 10.4 ± 0.3 mm at C6 and 11.2 ± 0.2 mm at C7. In the study by Lee et al(26) on the dry bones of Korean origin, the anterior height of the vertebral body was 14.9 ± 1.0 mm at C3, 14.0 ± 1.6 mm at C4, 13.3 ± 1.5 mm at C5, 13.5 ± 1.5 mm at C6 and 15.2 ± 1.3 mm at C7. The measurements of the present study parallel those recorded in Tan et al’s(31) study (
In conclusion, most published studies on the UP and vertebral body obtained measurements using dry bones. However, in the present study, morphometric measurements relating to the UP and vertebral body were taken directly and on CT of the same cadavers, with preservation of the complete vertebra of the cadaver in the vertebral series. This should result in more valid measurements of the anatomical structures that surgeons may encounter during surgical intervention. We hope that the measurements obtained in the present study will help spinal surgeons to achieve greater success in cervical operations.


