Abstract
INTRODUCTION
Knowledge of the pattern of alcohol-associated injury (AAI) is lacking in Singapore. We aimed to determine the local demographic pattern, injury mechanism, injury severity and outcomes of AAI.
METHODS
Data on trauma cases presenting to emergency departments in 2012–2013 was extracted from the National Trauma Registry. Cases with missing data fields and those aged 1–15 years were excluded. Patients were classified as alcohol positive (A+) or negative (A−) based on clinical assessment. The two groups’ demographics, injury mechanism, injury severity, mortality and disposition were compared. Logistic regression analysis was used to determine independent associations with mortality.
RESULTS
105,468 trauma cases met the inclusion criteria. 3.9% were A+ and their peak age range was 25–44 years. The A+ group had more Indian males (p < 0.001), and significantly more assaults, self-harm and falls (p < 0.001). Injuries in the A+ group were more common in public areas and less common in homes, recreational facilities and workplaces. Outcomes in the A+ group showed higher mean Injury Severity Score and mortality (p < 0.001). Significantly more A+ patients were admitted to hospital but had shorter mean length of stay (p < 0.001). Multivariate logistic regression revealed age > 44 years and male gender as independent predictors of mortality.
CONCLUSION
AAI in Singapore is associated with more severe injuries and resource utilisation. Using data from the registry, ‘at risk’ demographic groups are identified for targeted injury prevention. However, alcohol use is not an independent predictor of mortality in trauma cases.
INTRODUCTION
Alcohol consumption is an important contributing factor for the presentation of injured patients to the emergency department (ED). The prevalence of alcohol-associated injury (AAI) presenting to EDs in the United States was reported to be 40%–50%.(1-3) Most of the publications on AAI in Singapore have concentrated on motor vehicle crashes (MVC).(4-7) Although sensational due to the criminal implications and higher likelihood of fatalities, alcohol-associated MVC are only the tip of the AAI iceberg. Alcohol-associated assaults and falls are far more common, carrying a significant burden of injury and strain on healthcare resources.(8,9) Epidemiological research shows that on a population-based level, most alcohol-associated harm, such as falls and assaults, is not attributed to those with severe alcohol dependence but to a much larger group of hazardous or harmful drinkers whose consumption exceeds recommended drinking levels. Secondary prevention strategies need to target this group. Data from other countries cannot be extrapolated locally because the role of alcohol in injury occurrence varies according to regional and cultural differences in drinking patterns.(10,11) Therefore, a better understanding of AAI in Singapore is important to inform preventative efforts.
This study aimed to evaluate the local demographic pattern, injury mechanism, injury severity and outcomes of AAI in Singapore by utilising data from the National Trauma Registry (NTR). It is an exploratory study that looked at associations between alcohol consumption and injury pattern, injury severity and outcomes.
METHODS
Data on trauma cases presenting to EDs in Singapore between 1 January 2012 and 31 December 2013 was extracted from the NTR, a nationwide registry mandated under the National Registry of Diseases Act. Data from all public hospitals’ emergency departments and trauma services; the Singapore Civil Defence Force (SCDF), which runs the country’s emergency medical services; and the forensic medicine division of the National Health Sciences Authority are electronically linked to the central NTR, housed in the National Registry of Diseases Office. Inclusion criteria were all trauma cases in the NTR during that time period. Exclusion criteria were any cases with missing data fields and patients who were aged 1–15 years, as this age group is considered too young to consume alcohol. A sensitivity analysis was also done because a large number of cases had to be excluded, as the ‘alcohol use’ field was not filled when the trauma information was compiled in the NTR.
A total of 401,035 trauma cases were identified at the start of the study. Upon application of the exclusion criteria, only 105,468 cases remained. These cases were then grouped into those coded as having consumed alcohol (A+) and those who had not (A−). A patient was coded as A+ if he or she gave a history of alcohol consumption before the injury was sustained or if alcohol fetor was detected by the attending physician. Ethical approval for the study was obtained from the National Healthcare Group Domain Specific Review Board.
The following data was extracted for each case: demographics (age, gender, ethnicity and citizenship); ED visit information (time, day and month); injury information (alcohol use, intention of injury, type of injury, mechanism of injury and place of injury); Injury Severity Score (ISS); Glasgow Coma Scale (GCS) score; patient disposition (discharged, admitted to general ward, admitted to high dependency unit or intensive care unit); length of stay; and repeat attendance within 72 hours of discharge.
The available literature revealed that the mortality rates of intoxicated and non-intoxicated patients were 23.1% and 12.7%, respectively.(12) Based on 80% power to detect a difference of 10% between the two groups, a sample size of 462 was required. The significance level was set at 0.05.
Statistical analysis was performed using IBM SPSS version 21.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics for continuous, non-categorical data consisted of central tendency measures (mean or median), and the percentage frequency of occurrence was used for data that could be categorised. Statistical significance was taken as p < 0.05. Univariate analysis was performed with the Mann-Whitney U test, bivariate analysis with the chi-square test, and multivariate logistic regression using binomial regression.
RESULTS
3.9% of all trauma patients were coded positive for alcohol consumption on presentation to the ED.
Table I
Demographics of the study population.
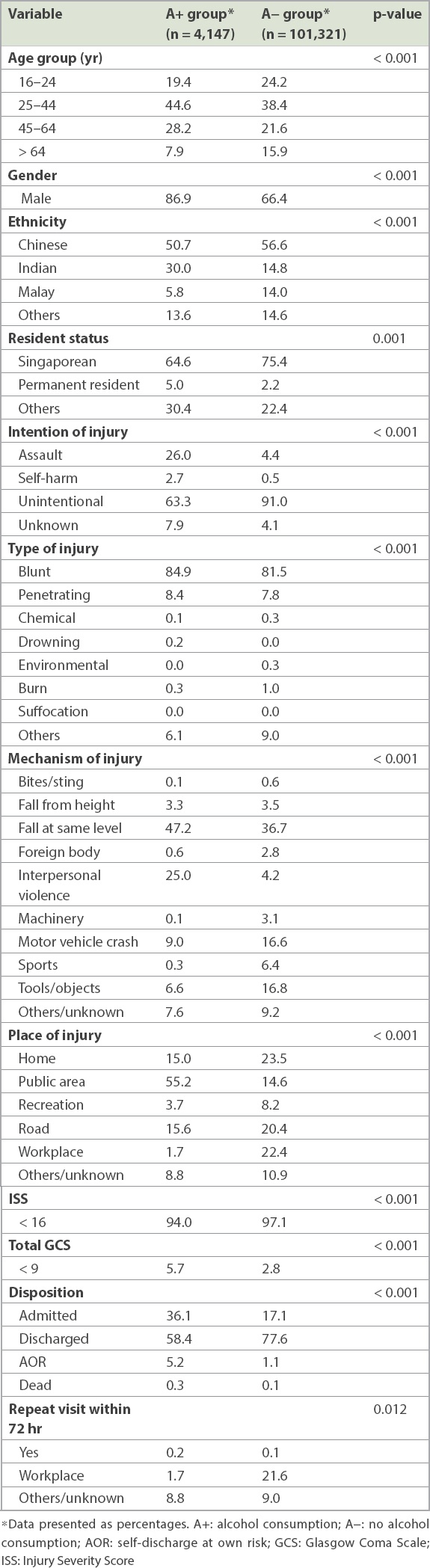
Table II
Comparison of age and admission characteristics of study population.
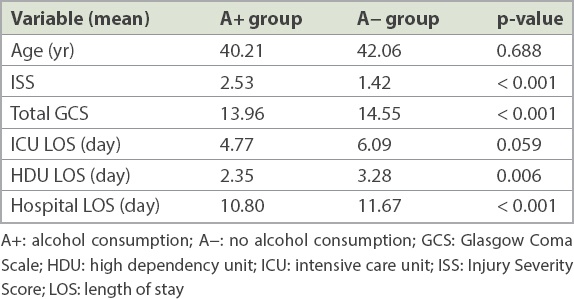
Multivariate logistic regression revealed that age 45–64 years (odds ratio [OR] 2.8; 95% confidence interval [CI] 1.6–4.7), age > 64 years (OR 3.2, 95% CI 1.8–5.6; p < 0.001) and male gender (OR 2.0, 95% CI 1.4–3.1; p = 0.001) were significant predictive factors for mortality. Alcohol use was not an independent predictor of mortality (p = 0.157,
Table III
Logistic regression model for the outcome of mortality.
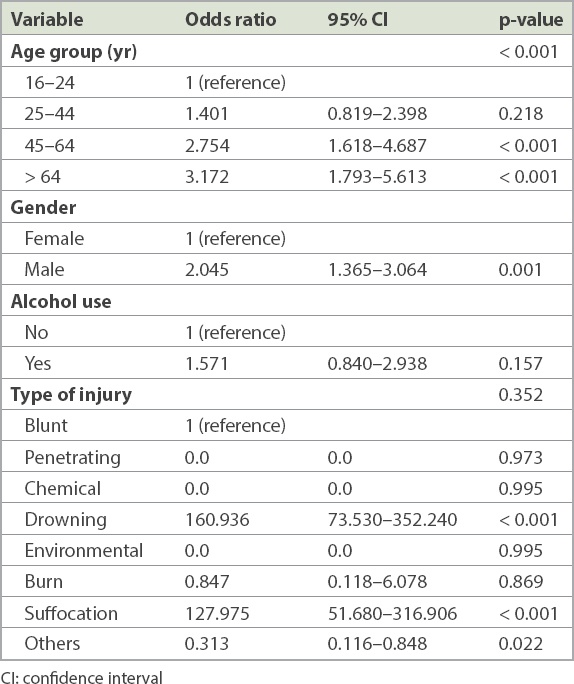
Fig. 1
Bar chart shows the arrival pattern of A+ and A− patients by hour of day.
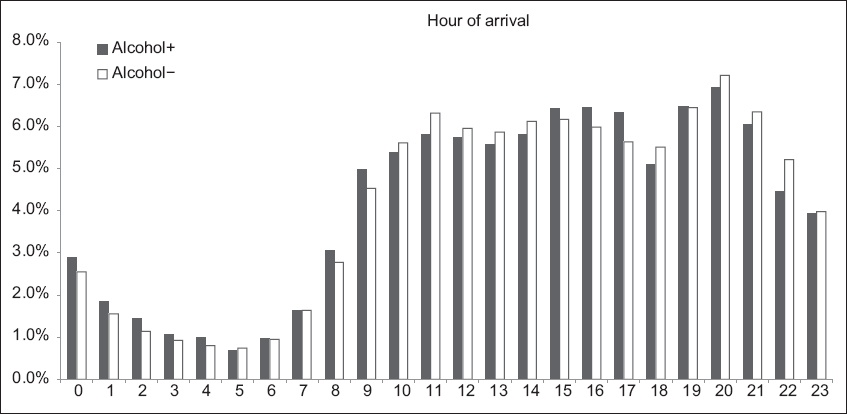
Fig. 2
Bar chart shows the arrival pattern of A+ and A− patients by day of week.
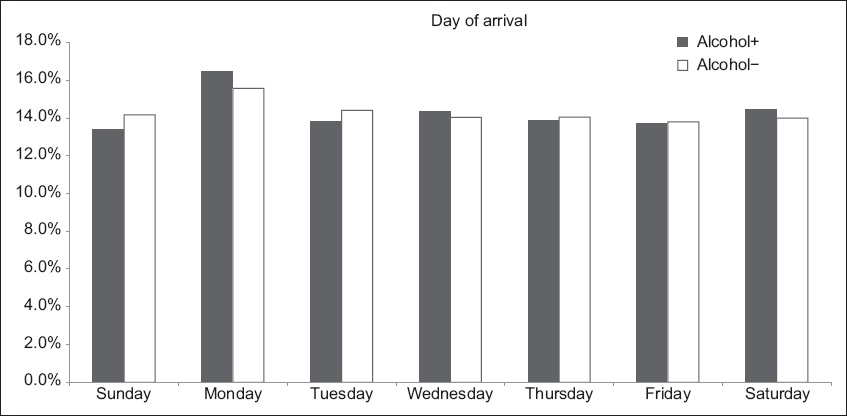
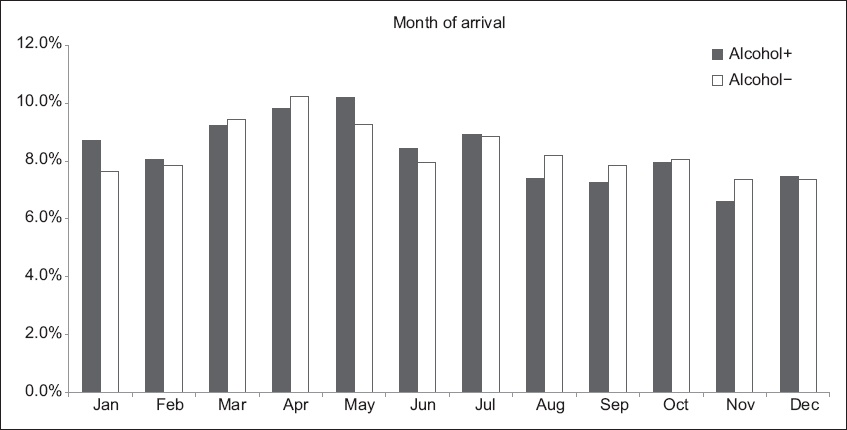
Fig. 3
Bar chart shows the arrival pattern of A+ and A− patients by month of year.
Sensitivity analysis was performed on two hypothetical scenarios of cases with missing data on alcohol intoxication versus no alcohol intoxication (Appendix). One scenario assumed that the patients with missing data were alcohol intoxicated while the other assumed that they were not alcohol intoxicated. Sensitivity analysis showed that the variables’ significance was not affected by classifying unknown alcohol use cases as A+ or A−. The results below indicate the differences between the original and sensitivity analyses.
When the unknown cases were classified as A+, in the logistic regression model, all ages were found to be significant (p < 0.001) for the outcome of mortality, as were alcohol use (p < 0.001) and type of injury (p < 0.001). Within the type of injury subgroup, penetrating trauma, drowning and suffocation were significantly associated with mortality, while the other types of injury were not significantly associated with mortality.
When the unknown cases were classified as A−, in the logistic regression model for the outcome of mortality, the age groups 45–64 years and > 64 years (p < 0.001), alcohol use (p = 0.008) and type of injury (p < 0.001) were significantly associated with mortality. Within the type of injury subgroup, penetrating trauma, drowning and suffocation were also significantly associated with mortality, while the other types of injury were not significantly associated with mortality.
DISCUSSION
The NTR is a comprehensive record of all trauma cases in Singapore and we were able to study the local demographic pattern, injury mechanism, injury severity and outcomes of all types of AAIs. Previous reports on AAI rates in Singapore have mainly focused on MVC, which vary from 2.3%–3.0%(4) to 10%(5) in the 1980s. In 2004, Tham et al(6) reported that alcohol consumption was 0.9% among motor vehicle injury victims, while Heng et al(7) reported in 2006 that alcohol was detected in 11.3% of bicycle crashes in Singapore. Comparatively, the rates of AAIs in MVC in Taiwan were 4.2% for bicycles and 9.6% for motor vehicles, whereas in Germany, bicycle injury related to AAIs was reported to be 57%.(13,14)
Since these studies were published, there have been increased education and enforcement efforts,(15-17) albeit confounded by changes in population demographics. A decade later, our study finds that AAI remains an injury burden. The vulnerable population at which injury prevention efforts should be targeted has been identified. Resource utilisation, in terms of the rate of hospitalisation among patients in the A+ group, is shown to be greater, albeit with shorter lengths of stay. In the current climate of chronic bed shortage, ED observation protocols for these patients have been developed to preserve valuable resources such as hospital beds. However, whether the patient is admitted to a ward bed or occupies a ‘trolley bed’ in an ED observation ward, medical and nursing resources are still required to care for these patients.
Contrary to the common belief that AAIs occur more commonly around festive periods,(18-20) our study found that AAIs peaked in April and May. This could be due to the increase in anti-drunk-driving media exposure and highly visible police enforcement with random alcohol breath screening testing, which usually takes place in December and January, around the major holidays, and relative lull in the middle of the year. Law enforcement and the media may wish to alter their publicity timing with regular ‘boosters’ throughout the year. AAI is no longer a weekend phenomenon and occurs evenly throughout the week. The SCDF and EDs may also need to alter their staffing plan based on these AAI patterns.
There are some limitations to the present study. First, the NTR does not receive data from private hospitals because the SCDF ambulance service, which responds to all 995 calls, does not convey trauma patients to private hospitals. Hence, the public hospitals, which report to the NTR, see all but the most trivial trauma cases; therefore, missing data on trauma cases is negligible. However, many cases had to be excluded, as the entries in the NTR contained a large number of blank data fields. Second, alcohol consumption was determined based on clinical detection of alcohol intake (e.g. alcohol fetor accompanied by flushing, inebriated speech or patient declaration of alcohol intake before sustaining injury). As blood alcohol concentration (BAC) sampling is not mandated in Singapore, unless specifically requested by the police for prosecutory purpose, it was decided when the NTR was set up that clinical detection by the attending physician was sufficient. Usage of clinical detection of alcohol alone has been previously reported. Although the BAC and degree of intoxication could not be determined in our cohort, we opine that it is immaterial, as evidence shows that any departure of BAC from zero is sufficient to impair performance.(21) We have noted the clinical detection method of alcohol use in publications by O’Connor and Ruiz(22) and Asante et al,(21) which used a clinical definition of alcohol involvement based on the history of alcohol consumption within six hours, as well as clinical symptoms and signs of alcohol intoxication. We agree that there could have been limitations such as misclassification and potential measurement bias with this approach. Furthermore, sensitivity analysis resulted in changes in OR for most of the variables. This is to be expected due to the significant amount of missing data, which is the main limitation of this study.
In conclusion, AAIs in Singapore are associated with increased injury severity and resource utilisation. Through the use of data from a local NTR, ‘at risk’ demographic groups were identified for targeted injury prevention. However, alcohol use was not found to be an independent predictor of mortality in trauma cases.


