Dear Sir,
We report a case of platypnoea-orthodeoxia syndrome (POS), a condition characterised by a sensation of breathlessness (platypnoea) and low oxygen saturation in the upright position that improves on lying down (orthodeoxia), which was diagnosed and demonstrated elegantly on transoesophageal echocardiography (TEE). First described by Burchell et al,(1) this condition is associated with patent foramen ovale (PFO) or combined with an atrial septal aneurysm (ASA).(2) Up till the 20th century, only 40 cases were reported,(3) but a review of the current literature reveals at least 150 case reports to date. What was previously deemed uncommon is now increasingly recognised as an important and reversible cause of hypoxaemia.
An 86-year-old man first presented with unwitnessed fall and head injury to the neurosurgical team. He had transient episodes of dyspnoea and desaturation during rehabilitation. Cardiorespiratory examinations, haematological and biochemical analysis, and resting electrocardiogram were normal. Chest radiograph revealed clear lung fields. An arterial blood gas test done in room air showed significant hypoxaemia (PaO2 48 mmHg) and an elevated alveolar-arterial gradient of 68 mmHg (expected 21 mmHg). Computed tomography angiography of pulmonary arteries showed no evidence of pulmonary embolism or intrapulmonary vascular malformation.
Transthoracic echocardiography revealed normal left ventricular ejection function and no pulmonary hypertension. Bubble study with Valsalva manoeuvre showed a right-to-left shunt at the level of the atria. The patient was further evaluated with TEE in the absence of sedation, which confirmed the presence of an ASA and PFO. In the supine position, the saturation was 97% on 2 L of intranasal oxygen, and there was no significant right-to-left shunt with agitated saline contrast and on colour Doppler (
Fig. 1
Echocardiographic images taken while the patient was in the supine position show: (a) before the bubble study, no separation of the inter-atrial septum (IAS); and (b) during the bubble study, no bubbles going across the IAS. RA: right atrium
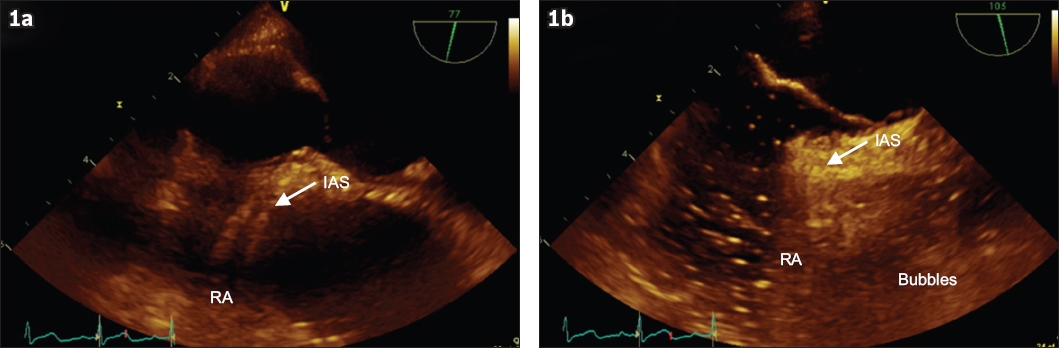
Fig. 2
Echocardiographic images taken while the patient was in sitting position show: (a) before the bubble study, separation of the inter-atrial septum (IAS); and (b) during the bubble study, significant right-to-left shunting, with bubbles going across the IAS. LA: left atrium; PFO: patent foramen ovale; RA: right atrium
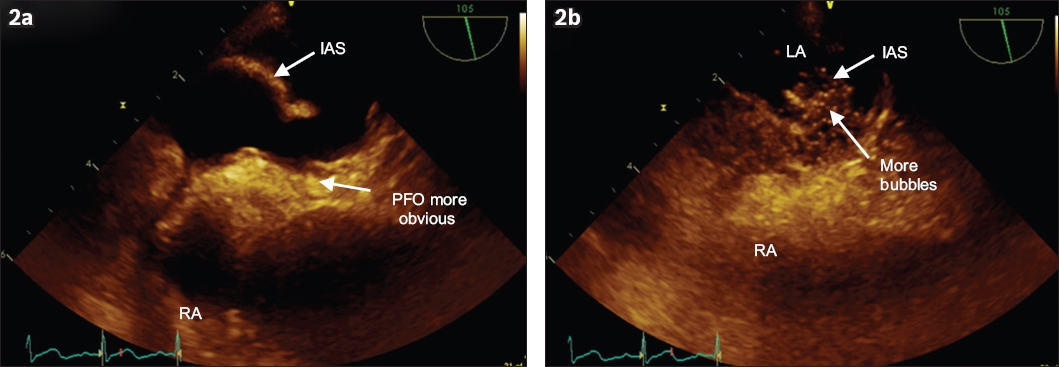
POS occurs as a result of right-to-left shunting in the absence of pulmonary hypertension and persistent right-to-left pressure gradient. To cause this phenomenon, two components are required:(3) an anatomical component in the form of an inter-atrial communication and a functional component that promotes abnormal shunting of blood with positional change. In our patient, POS was likely precipitated by dehydration, reducing left atrial pressure more than the right. The upright position stretches the inter-atrial communication, allowing increased streaming of venous blood from the inferior vena cava through the defect, thus causing desaturation and dyspnoea whenever he sat up. Performing a TEE with dynamic postural manoeuvres allows for a ‘live’ demonstration of this phenomena and elegantly confirms the diagnosis of POS. Definitive treatment involves closure of the intracardiac communication(4) via open surgery or transcatheter occlusion.(5)
Therefore, POS should be considered in the workup of dyspnoea. TEE with postural manoeuvres readily establishes the diagnosis when POS is suspected.
Yours sincerely,


