Abstract
INTRODUCTION
The obesity paradox, where obesity is associated with improved survival, has been described in patients undergoing haemodialysis and in those with heart failure. It was also demonstrated in patients undergoing valve replacement for aortic stenosis (AS). We explored this phenomenon in medically managed severe AS.
METHODS
154 patients with medically managed severe AS (aortic valve area index [AVAi] < 0.6 cm2/m2; mean pressure gradient > 40 mmHg and peak velocity > 400 cm/s) and preserved left ventricular ejection fraction (> 50%) were categorised into the obese (body mass index [BMI] Asian cut-off ≥ 27.5 kg/m2) and non-obese groups. Their clinical and echocardiographic profiles were compared.
RESULTS
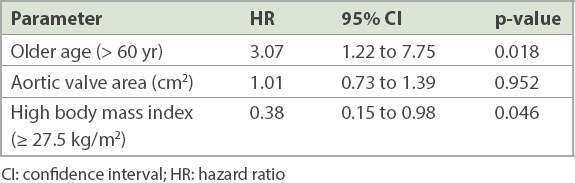
24 (15.6%) patients were obese. Obese patients were similar to non-obese patients in age (68.5 ± 11.6 years vs. 68.9 ± 13.1 years) but had higher prevalence of cardiovascular risk factors. Left atrial diameter (43.7 ± 6.7 mm vs. 38.5 ± 10.2 mm) was larger in obese patients, while left ventricular outflow tract diameter (19.5 ± 1.7 mm vs. 20.4 ± 2.1 mm) was smaller. Despite lower AVAi in obese patients (0.36 ± 0.10 cm2/m2 vs. 0.43 ± 0.11 cm2/m2), there was lower mortality (37.5% vs. 41.0%, log-rank 4.06, p = 0.045) on follow-up (8.0 ± 5.7 years). After adjusting for age and AVAi, higher BMI ≥ 27.5 kg/m2 remained protective for mortality (hazard ratio 0.38, 95% confidence interval 0.15 to 0.98, p = 0.046).
CONCLUSION
We demonstrated that obesity was associated with improved survival in severe AS despite lower AVAi and increased prevalence of cardiovascular risk factors.
INTRODUCTION
Obesity is a recognised risk factor associated with greater morbidity and mortality.(1) This may be partly explained by the association of obesity with other important medical conditions that are part of the metabolic syndrome, such as hypertension, hyperlipidaemia and diabetes mellitus.(2) The ‘obesity paradox’ refers to a phenomenon where the presence of obesity in certain patient populations may counterintuitively be protective and associated with better survival. This has been consistently described in patients undergoing percutaneous coronary intervention or coronary artery bypass grafting for ischaemic heart disease.(3,4) More recently, the obesity paradox has also been described in other forms of cardiac surgery or intervention, including surgical and transcatheter aortic valve replacement (TAVR) for severe aortic stenosis (AS).(5-7) Obese patients undergoing cardiac procedures and intervention tended to have better short- and long-term outcomes compared to their non-obese or underweight counterparts.
The rising trend and burden of disease that both obesity and AS pose in the context of a global ageing population highlight the importance of studying this phenomenon.(8) Beyond cardiac surgery, the obesity paradox has also been described in patients with renal failure undergoing haemodialysis and, separately, in patients with heart failure.(9,10) For patients with symptomatic severe AS, aortic valve replacement remains the mainstay of therapy, with TAVR being an attractive, minimally invasive alternative to surgical valve replacement for moderate- to higher-risk elderly patients.(11,12) It is still unclear whether the protective effect of obesity is limited to better periprocedural or surgical outcomes with lower complication rates, or if it also influences the natural history of severe AS. In fact, a previous study had denied the presence of the obesity paradox in patients with severe asymptomatic AS, and showed that obesity was instead associated with increased morbidity and mortality.(13)
Furthermore, a significant proportion of patients with AS, especially in the Asian context, remain medically managed. These patients either declined intervention for aortic valve (both transcatheter and surgical) or were deemed medically unfit for either procedure. The prognosis of these patients is understandably poorer compared to those who undergo valve replacement. However, the impact of obesity on this population with medically managed AS remains unclear. The present study aimed to examine the relationship between obesity (as defined by elevated body mass index [BMI]) and the echocardiographic profiles and clinical outcomes of Asian patients with medically managed severe AS.
METHODS
In this study, 154 consecutive patients with an index echocardiographic diagnosis of severe AS (defined as aortic valve area index [AVAi] < 0.6 cm2/m2, transaortic mean pressure gradient > 40 mmHg and transaortic peak velocity > 400 cm/s) were examined from 2000 to 2012. We included only patients with preserved left ventricular ejection fraction (LVEF) > 50% and excluded those with other concomitant valvular pathologies such as significant mitral regurgitation. At the time of the index echocardiography, the anthropomorphic measurements were also obtained, and height and weight were used to compute the BMI. As the study population was Asian, a cut-off BMI of 27.5 kg/m2 was used to define the presence of obesity.(14)
We compared obese and non-obese patients based on differences in their echocardiographic and clinical profiles. The diagnosis and classification of AS, as well as other echocardiographic parameters studied, were made in accordance with the guidelines of the American Society of Echocardiography/European Association of Cardiovascular Imaging.(15,16)
Subsequently, all 154 patients were followed up prospectively for at least five years after the index echocardiography to evaluate for clinical outcomes in the form of all-cause mortality. These patients were all medically managed, and patients who underwent valve replacement (transcatheter or surgical) were excluded, as their clinical course would likely have been significantly different. The patients in our study population may have either declined valve replacement or may been deemed medically unfit for the procedure. Predicted in-hospital mortality derived from EuroSCORE II was calculated for each patient when echocardiography was performed.(17,18)
Univariate analyses of clinical characteristics and echocardiographic parameters were used to compare the obese and non-obese patients, and these included Student’s t-tests to examine the association between continuous variables and Pearson’s chi-square test (or Fisher’s exact test where appropriate) to evaluate categorical variables. A multivariable Cox regression model was then constructed to quantify the hazard ratios of parameters associated with all-cause mortality in the study population, adjusting for the effects of older age and aortic valve area on the outcomes. Kaplan-Meier survival curves were constructed to compare the differences in survival between the obese and non-obese groups, along with calculation of the log-rank test statistic. A p-value < 0.05 was considered significant. All data was analysed using IBM SPSS Statistics version 20.0 (IBM Corp, Armonk, NY, USA). This study was approved by the relevant institutional review board.
RESULTS
Of the 154 patients studied, 24 (15.6%) were obese (BMI ≥ 27.5 kg/m2), while the remaining 130 (84.4%) patients were non-obese at the time of the index echocardiographic diagnosis of severe AS (AVAi < 0.6 cm2/m2 and transaortic mean pressure gradient > 40 mmHg and transaortic peak velocity > 400 cm/s). The obese patients were similar in age (68.5 ± 11.6 years vs. 68.9 ± 13.1 years, p = 0.892), trended towards a higher prevalence of male gender (66.7% vs. 50.0%, p = 0.133) and had a higher prevalence of cardiovascular risk factors, such as diabetes mellitus (35.0% vs. 23.8%, p = 0.293), hypertension (70.0% vs. 48.5%, p = 0.079) and hyperlipidaemia (65.0% vs. 33.7%, p = 0.009). There were no significant differences in the prevalence of ischaemic heart disease (20.0% vs. 27.7%, p = 0.474) and chronic kidney disease (10.0% vs. 5.9%, p = 0.504). Predicted in-hospital mortality based on EuroSCORE II was also similar between the two groups (7.3% ± 3.7% vs. 7.9% ± 5.0%, p = 0.706;
Table I
Univariate analysis comparing obese and non-obese patients having severe aortic stenosis with preserved left ventricular ejection fraction greater than 50%.
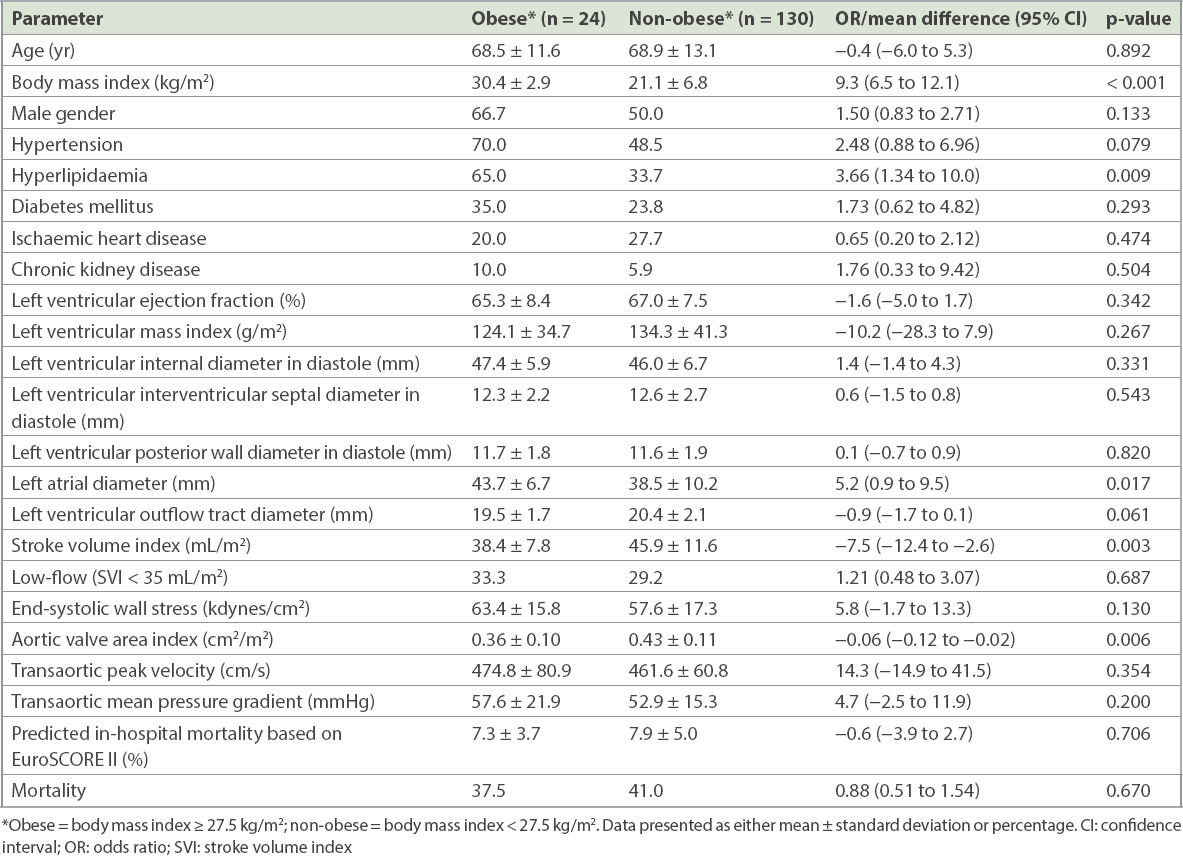
In terms of echocardiographic profile, LVEF was preserved in both groups, and was not significantly different. Left ventricular (LV) mass index was similar between the two groups (124.1 ± 34.7 g/m2 vs. 134.3 ± 41.3 g/m2, p = 0.267), with similar thickness of the LV wall but slightly larger LV internal diameter for obese patients. The left atrial diameter was slightly larger in obese patients (43.7 ± 6.7 mm vs. 38.5 ± 10.2 mm, p = 0.017), but the LV outflow tract diameter (19.5 ± 1.7 vs. 20.4 ± 2.1 mm, p = 0.061) and stroke volume index (38.4 ± 0.7.8 mL/m2 vs. 45.9 ± 11.6 mL/m2, p = 0.003) were smaller compared to the non-obese group. In terms of AS severity, it appeared that obese patients had lower AVAi (0.36 ± 0.10 cm2/m2 vs. 0.43 ± 0.11 cm2/m2, p = 0.006), but there were no significant differences in the transaortic mean pressure gradient or transaortic peak velocity between the groups (
On subsequent prospective follow-up (mean 8.0 ± 5.7 years), mortality was lower in the obese group (37.5% vs. 41.0%). Constructed Kaplan-Meier survival curves showed improved survival in the obese group compared to the non-obese group (
Fig. 1
Kaplan-Meier survival curves show improved survival in obese patients compared to non-obese patients with medically managed severe aortic stenosis.
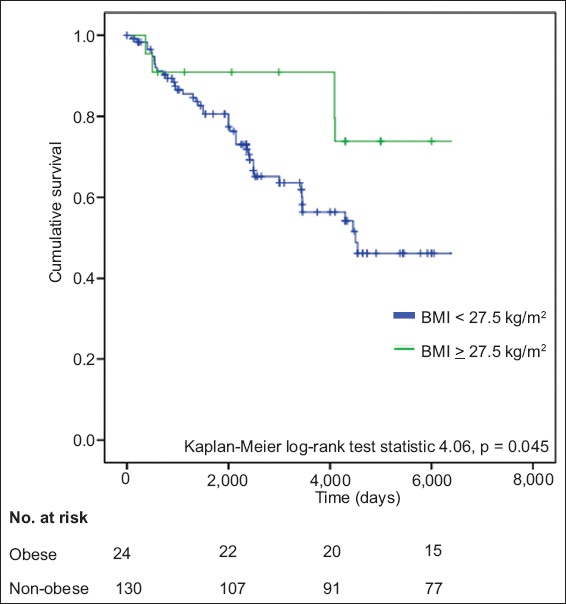
Table II
Multivariable Cox regression analysis comparing adjusted hazard ratios for mortality in severe aortic stenosis.
DISCUSSION
In the context of postoperative or post-surgical patients who underwent valve replacements, clinical outcomes have been consistently demonstrated to be better in obese patients compared to their non-obese counterparts.(19,20) These trends were also seen in other forms of cardiac surgery and intervention, including LV assist devices for heart failure.(21) Consequent findings were also true – patients with lower BMI were found to have higher rates of periprocedural or surgical mortality and sepsis.(22)
Of note, previous studies have consistently demonstrated better short-term (30-day) periprocedural outcomes for valve replacement in AS among obese patients.(7,17) However, in terms of longer-term prognosis (one-year overall survival), the trends were less clear. A few studies have found no significant differences in prognosis between obese and non-obese patients.(23-25) However, these studies may have been limited by smaller sample sizes and, consequently, may have been underpowered to demonstrate significant differences in longer-term survival between obese and non-obese patients. In fact, in a recent meta-analysis and systemic review where these studies on TAVR outcomes were pooled, it was convincingly demonstrated that higher BMI was associated with both lower short-term (30-day) mortality and better longer-term (one-year) overall survival.(26)
There could be several possible reasons to explain this phenomenon, one of which is the larger body surface areas of obese patients, which may account for the better short-term periprocedural outcomes. These patients would have larger vessels that could be easier to traverse, which would, in turn, result in lower risks of complications and vascular injury during TAVR. In patients undergoing TAVR, smaller vessel size has been shown to be an important cause of early mortality.(27)
In the present study, we examined a population of patients with severe AS that was medically managed. We adopted a more ‘stringent’ criteria for defining severe AS, where all patients met the valve area, transaortic mean pressure gradient and peak velocity criteria for severe AS (i.e. AVAi < 0.6 cm2/m2 and transaortic mean pressure gradient > 40 mmHg and transaortic peak velocity > 400 cm/s). This population of patients with severe AS was studied because in our Asian context, a significant proportion of patients with severe AS either declined aortic valve replacement or were deemed unfit for the procedure. This population also had a significant prevalence of medical comorbidities such as ischaemic heart disease (25.0%) and chronic kidney disease (7.0%). The predicted in-hospital mortality based on EuroSCORE II was comparable in the two groups (7.3 ± 3.7 vs. 7.9 ± 5.0%, p = 0.706). Furthermore, TAVR was introduced in our centre only in 2010 and thus, a significant proportion of our study population was in the pre-TAVR era. This meant that they would not have been offered TAVR if they declined surgical aortic valve replacement.
In the context of medically managed severe AS, there may have been other important protective effects of obesity. Obese patients in our study were similar in age to non-obese patients. In prior studies on the obesity paradox in patients with severe AS undergoing valve replacement, obese patients tended to be younger in age.(22,28) The protective effect of obesity may, thus, be partly confounded by the younger age and correspondingly better cardiac and renal function in these patients, which resulted in better clinical outcomes. However, in this study, we adjusted for the effect of age and, therefore, higher BMI remained an independent protective factor for mortality in medically managed severe AS.
Differences in nutrition may also be important in this context. This has been examined more thoroughly in patients with non-cardiac chronic diseases. The presence of weight loss often reflects malnourishment and is an indicator of severe disease, which, in turn, would be predictive of poorer clinical outcomes.(29) Frailty with lower skeletal muscle mass and BMI may also reflect lower biological reserves, resulting in poorer clinical outcomes.(30)
Furthermore, as obese patients tend to have higher prevalence of cardiovascular risk factors such as hypertension, hyperlipidaemia and diabetes mellitus, they are consequently more intensively treated with cardioprotective drugs. These patients are also more likely to be on closer follow-up with a cardiologist and compliant to guideline-based medical therapy.(31) Closer monitoring and follow-up of obese patients, as well as the use of cardioprotective drugs in the obese population, may have conferred additional survival benefit.
Some authors have postulated that adipose tissue itself may be a source of reserves for better recovery. Adipose tissue produces receptors for tumour necrosis factor alpha and helps to counteract and reduce the effect of inflammation, thereby promoting recovery.(32,33) This mechanism may be important in surgical patients, where wound healing is crucial, but may be less relevant in medically managed patients with severe AS and for patients undergoing less invasive procedures such as TAVR.
In contrast to the abovementioned studies and the findings of this study, a recent large study conducted in a population of patients with severe asymptomatic AS demonstrated that mortality and morbidity were higher among obese patients.(13) However, the patients studied were all relatively younger (mean age 67 ± 10 years vs. 72 ± 10 years in our study) and asymptomatic, and hence, they were likely to be earlier in the course of their disease. The obesity paradox may, thus, only be apparent in patients who are more frail, more elderly and have more advanced disease, which was supported by findings on subgroup analyses of subsequent follow-up studies.(34) Our study also adjusted for the effect of age and demonstrated that higher BMI was independently associated with improved survival.
Furthermore, it is important to note that the obesity paradox may be partially explained by the cross-sectional nature of the study design, which was subjected to lead-time bias. Patients were studied and compared at the time of the index echocardiographic diagnosis of severe AS, but they may individually have been at different time points along the natural history of the disease progression of AS. Patients with higher BMI may have been earlier in the course of the disease, while patients later in the course with more advanced disease may have had more symptoms of heart failure and cardiac cachexia, which resulted in a lower BMI. This may have led to an apparent protective benefit of higher BMI on patients with severe AS, rather than obesity conferring a true survival benefit.(35) Longitudinal prospective follow-up of obese patients with serial measurements of BMI over time and follow-up echocardiography may be important to further evaluate these trends.
This study was not without limitations. We studied a moderately sized Asian cohort of medically managed patients with severe AS. The definition of severe AS relied on parameters such as aortic valve area, transaortic mean pressure gradient and peak velocity, but we did not quantify the degree of aortic valve calcification or the symptom status of the patients. However, we ensured accurate measurement of transaortic gradients in all our echocardiographic studies by performing multiple assessments to obtain the highest transaortic gradients, including routinely using Pedoff transducer probes. Of note, a significant proportion of our Asian cohort had paradoxical low-flow AS (31.2%), which was similarly demonstrated in a previous study. The impact of obesity on this subgroup of patients, who may have distinct and poorer clinical outcomes, could be an important subject for future studies.(36,37)
Although we studied a heterogeneous group of symptomatic and asymptomatic patients, the obesity paradox was still demonstrated after adjusting for confounding factors. Establishing the time of onset of symptoms along the course of a patient’s disease and consequently comparing the duration in which these patients had been symptomatic may be useful in predicting clinical outcomes.(38) We did not examine serial echocardiographic studies on follow-up for progression of AS and changes in echocardiographic profile over time. Furthermore, BMI was measured only at the time of the index echocardiography, and changes in each patient’s BMI on subsequent follow-up were not tracked. Also, obesity was quantified by means of BMI only; we did not examine or compare waist circumference or estimated body fat percentages. Abdominal obesity, which has been shown to be important in Asians, was also not evaluated.(14) The cross-sectional nature of this study also meant that it was subjected to lead-time bias, where patients may have been studied at differing time points of the natural history of AS progression. Nevertheless, this study remains important, as it was both exploratory and hypothesis-generating, and the findings suggest that the obesity paradox may extend beyond periprocedural risks and complications to apply to patients with severe AS who are medically managed. Further prospective and longitudinal studies are warranted to confirm and evaluate the clinical significance of these findings.
In conclusion, this study found that obesity (BMI ≥ 27.5 kg/m2) was associated with improved survival in an Asian population of patients with medically managed severe AS. This trend of improved survival was independent of age and AS disease severity, and was also observed in spite of lower AVAi and higher prevalence of cardiovascular risk factors in patients with obesity.


