Abstract
INTRODUCTION
The ‘DOT & Shop’ scheme is sponsored by SATA CommHealth, a local non-governmental organisation. It was launched in July 2009, in collaboration with Singapore’s Tuberculosis Control Unit (TBCU). Under this scheme, grocery vouchers are disbursed to low-income patients with tuberculosis (TB) at each clinic visit if they have been adherent to directly observed therapy (DOT). This study aimed to determine the effect of this incentive scheme on treatment completion rates and to report the characteristics of patients who were non-adherent to the scheme.
METHODS
This descriptive study used data from the TBCU medical social worker database and the National TB Registry.
RESULTS
From July 2009 to December 2012, a total of 883 TB patients were enrolled in the scheme. The overall treatment completion rates of the patients before (July 2006–June 2009) and after (July 2009–December 2012) the implementation of the scheme improved from 85.3% to 87.2% (p = 0.02). Patients under this scheme had a higher treatment completion rate (90.0%) than those not under this scheme (86.4%) (p < 0.01). It was found that the non-adherent patients were more likely to be of Malay ethnicity, younger and unemployed.
CONCLUSION
We demonstrate the salutary effect of a non-governmental organisation-funded grocery voucher incentive scheme for low-income TB patients on DOT in Singapore.
INTRODUCTION
Singapore has seen a decline in the incidence rate of tuberculosis (TB), from 300 cases per 100,000 population in the 1960s to 55 cases per 100,000 population in 1987.(1) This decline occurred due to socioeconomic progress, the advent of short-course TB chemotherapy and the national TB programme. Following a ten-year stagnation in TB incidence rate, the Singapore TB Elimination Programme (STEP)(1) was launched in 1997. The key interventions were: (a) directly observed therapy (DOT) in public primary health clinics; (b) monitoring of treatment progress and treatment outcome via a National TB Surveillance Registry; and (c) preventive therapy for recently infected close contacts of infectious TB patients. STEP was successful in decreasing TB incidence until 2008, when Singapore’s TB rate among the resident population began to increase from an all-time low of 35 cases per 100,000 population in 2007 to 41 cases per 100,000 population in 2011.(2) This increase is likely due to multiple factors, including the influx of immigrants (from countries with high TB incidences) since 2005, a rapidly ageing population, increasing prevalence of diabetes mellitus and increasing diagnostic delay in cases of infectious TB. Furthermore, all these factors occurred against a backdrop of increasing population density.(3) Another important potential contributing factor is the failure of patients to complete their TB treatment. In response to this TB resurgence, a multipronged strategy was initiated. The strategy included the expansion of DOT, the enhancement of physicians’ awareness (via seminars and the media) that TB can be the cause of prolonged cough, and the expansion of TB Contact Clinic’s coverage. The present study reports our experience with an enhanced DOT strategy.
In 1994, the World Health Organization (WHO) launched the DOT short course,(4) a component central to the global strategy for effective TB control. In Singapore, ambulatory TB patients receive DOT at any one of the 18 public polyclinics located at town centres and population concentrations distributed throughout the island. Although these locations are accessible, patients have to make the effort to go to the polyclinic for their daily (or thrice-weekly) medicine. The structure of DOT keeps patients focused and adherent amid competing priorities. For patients who are recalcitrant non-adherents to TB treatment, legal action (under the Ministry of Health Infectious Diseases [ID] Act) is taken to compel them to undergo compulsory DOT until the completion of treatment.
The use of incentives has long been considered to have a positive impact on patient adherence.(5-15) As TB disproportionately afflicts the poor, financial and social factors may affect adherence to treatment. An incentive scheme called ‘DOT & Shop’, which is sponsored by SATA CommHealth, a local non-governmental organisation, was implemented in July 2009 for low-income TB patients treated at Singapore’s TB Control Unit (TBCU). The TBCU treats about 75% of all notified TB patients in Singapore. Eligible patients who were adherent to DOT were given grocery vouchers at each clinic visit (usually on a monthly basis) to enable and incentivise them to successfully complete treatment.
In order to evaluate the effect of the ‘DOT & Shop’ scheme, we compared: (a) the treatment completion rates of TBCU patients (Singapore residents) during the implementation of the scheme (July 2009–December 2012) with those of historical controls (July 2006–June 2009); and (b) the treatment completion rates of patients who were enrolled in the ‘DOT & Shop’ scheme during the implementation period with those of patients who were not enrolled in the scheme during the implementation period. We also looked at: (a) the proportion of TBCU patients who were served under the ID Act before and after the implementation of the scheme; and (b) the characteristics of the patients who were non-adherent to DOT even though they were enrolled in the scheme.
METHODS
Patients on DOT were interviewed by TBCU nurses and medical social workers (MSWs) to determine their eligibility for inclusion in the ‘DOT & Shop’ scheme. They were eligible if they met the following criteria: (a) Singapore residents (i.e. Singapore citizens or permanent residents); (b) aged 16 years and above; and (c) per capita income (PCI) (i.e. household income divided by the number of occupants) of less than SGD 900. Patients enrolled in this incentive scheme had to sign a letter of undertaking to signify that they understood the purpose of the scheme and that the grocery vouchers would be disbursed by the MSWs under the conditions stipulated by SATA CommHealth. At each clinic visit, the attending physician checked the patient’s DOT polyclinic attendance form. Patients routinely made a total of eight visits, of which six were eligible for vouchers, if they were on a six-month TB regimen. Patients received grocery vouchers worth SGD 40 from the MSWs each time if they did not miss any DOT doses at the Week 2 visit, the Week 8 visit and the subsequent three visits (visits were made every 4–5 weeks), following which the patients would have received a total of SGD 200 worth of grocery vouchers. Patients were given a bonus SGD 100 voucher if they completed the entire TB treatment (i.e. at the eighth and final visit on the sixth month). Patients fully adherent to the six-month and nine-month regimens (three additional visits) would thus receive a total of SGD 300 and SGD 420 worth of vouchers, respectively. Patients were taken off the scheme if they persistently missed DOT doses, collected four or fewer vouchers, were lost to follow-up, or if their treatment delivery mode was changed to self-administered therapy.
A subpopulation of 659 patients enrolled in the ‘DOT & Shop’ scheme from July 2009 to December 2011 was analysed to ascertain the association, if any, between sociodemographic factors and non-adherence (i.e. missed doses). There were 12 patients who were adherent to treatment but failed to receive the vouchers because they were granted self-administered therapy, as they were either travelling or hospitalised; these patients were excluded from the analysis.
Data pertaining to patient demographics, housing type and treatment outcome were obtained from the Singapore National TB Registry, while data on the patient’s PCI, missed doses and adherence to the scheme were extracted from the MSW database. The treatment outcome of notified TB patients in Singapore has been monitored by the Treatment Surveillance Module (TSM) of the STEP Registry since 2001; our ten-year experience with TSM has been reported previously.(16) The outcomes are determined on a quarterly cohort basis at the end of each corresponding quarter of the following year.(17-21) Using data from the registry, the treatment completion rate and other outcomes (e.g. death, lost to follow-up, still on treatment) of all patients treated at the TBCU before implementation of the scheme (July 2006–June 2009) and after implementation of the scheme (July 2009–December 2012) were compared. We also compared the treatment completion rates of patients who were placed on the scheme with those of patients who were not, during the period after scheme implementation (i.e. July 2009–December 2012). The proportion of patients who were served under the ID Act in order to complete their TB treatment before and after the scheme was also compared.
Data analysis was performed using the STATA software version 10.0 (StataCorp, College Station, TX, USA). Descriptive statistics were computed, and either the Chi-square test or Fisher’s exact test (for sample size < 20) was used to compare categorical variables. Continuous variables were analysed using Student’s t-test. A p-value ≤ 0.05 was considered statistically significant. Ethics approval was not sought for the present study, as it was embedded into our existing TB services (i.e. it fit into the routine practices and job descriptions of our healthcare workers).
RESULTS
A total of 883 patients were enrolled in the ‘DOT & Shop’ scheme between July 2009 and December 2012 (
Table I
Sociodemographic characteristics of the patients from Singapore’s Tuberculosis Control Unit who were on the ‘DOT & Shop’ scheme (from July 2009 to December 2012) (n = 883).
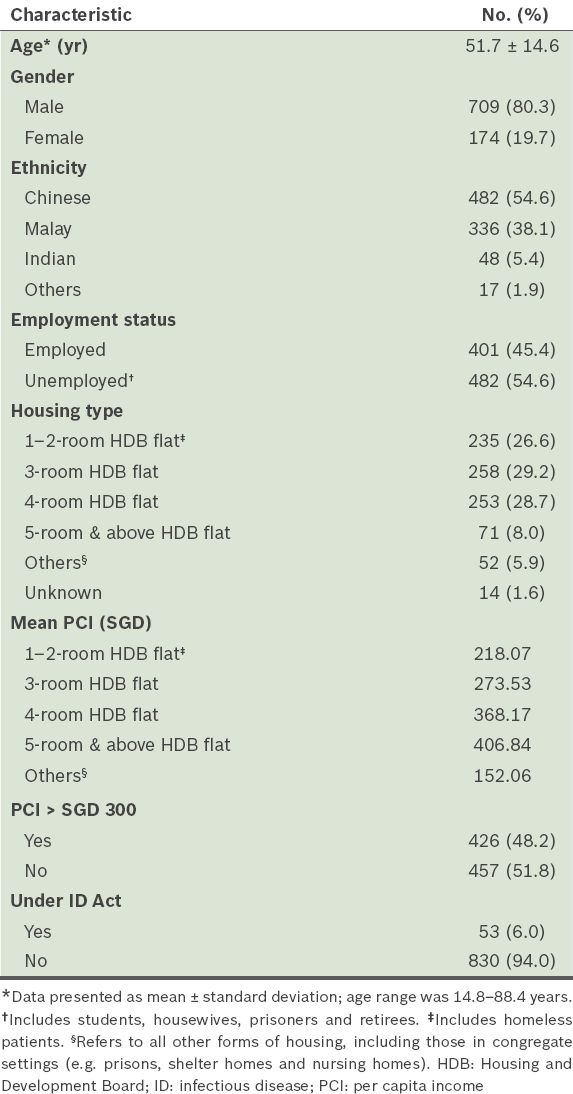
Fig. 1
Flowchart shows the proportion of patients from Singapore’s Tuberculosis Control Unit (TBCU) who were on directly observed therapy (DOT), enrolled in the ‘DOT & Shop’ scheme, and under the Infectious Diseases (ID) Act.
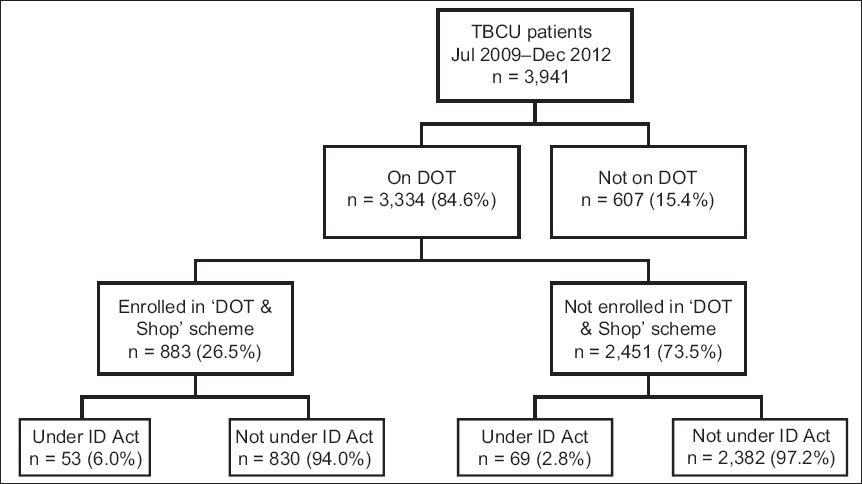
The treatment completion rate of the patients treated at the TBCU in the 36 months (July 2006–June 2009) before implementation of the incentive scheme was 85.3% (2,449/2,872). This rate improved to 87.2% (3,436/3,941) after implementation of the scheme (July 2009–December 2012) (p = 0.02) (
Fig. 2
Graph shows the treatment outcomes of Singapore residents treated at Singapore’s Tuberculosis Control Unit before (July 2006–June 2009) and after (July 2009–December 2012) the implementation of the ’DOT & Shop’ scheme. DOT: directly observed therapy
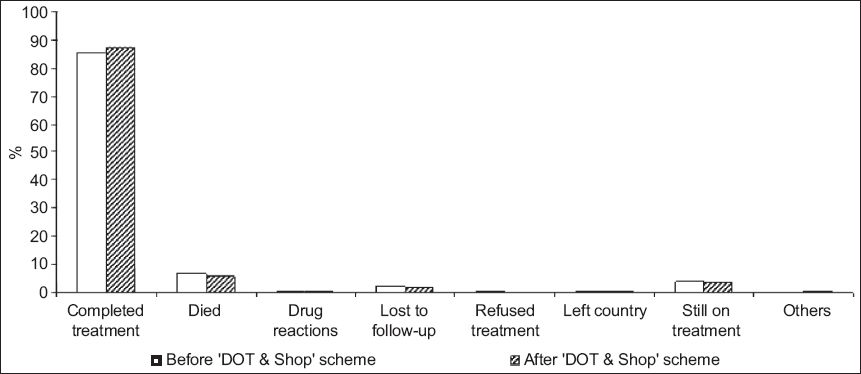
Fig. 3
Graph shows the treatment completion rates of patients after the implementation of the ‘DOT & Shop’ scheme (i.e. July 2009–December 2012). DOT: directly observed therapy
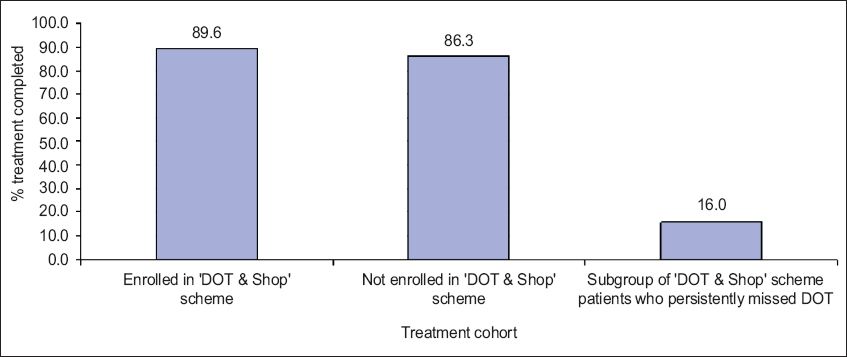
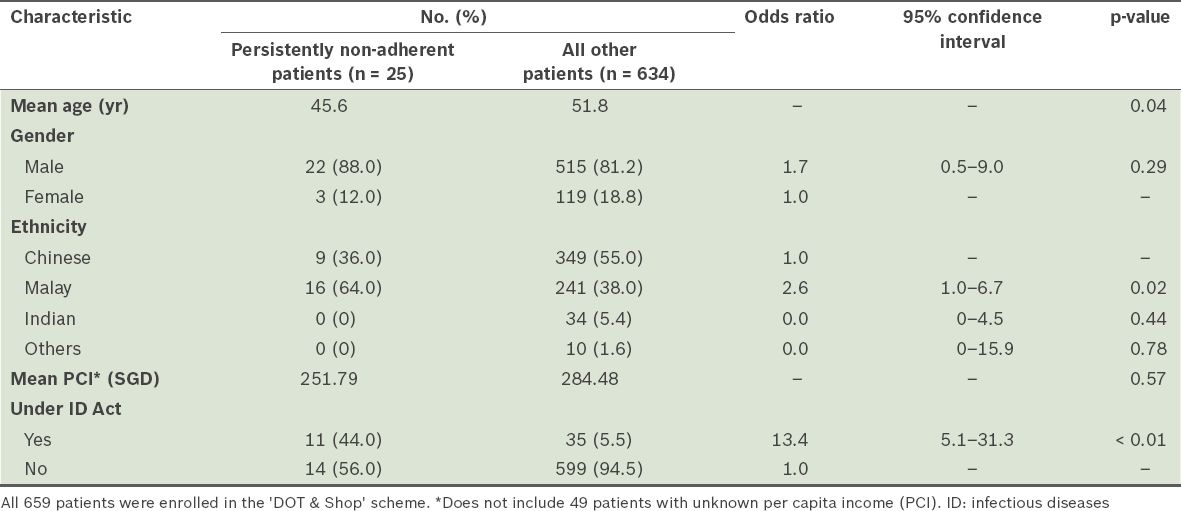
From the MSW database, we analysed the subgroup of 659 patients who were enrolled in the scheme between July 2009 and December 2011; they were analysed for missing DOT doses (i.e. did not receive the maximum number of grocery vouchers). The mean age of these patients was 45.6 years. Of these 659 patients, 75 (11.4%) missed one or more DOT doses. Most of these patients cited work commitments as their reason for missing DOT doses. A total of 25 patients were taken off the ‘DOT & Shop’ scheme because they were persistently non-adherent to DOT (
Table II
Comparison of the characteristics of the patients who were persistently non-adherent to directly observed therapy (DOT) (n = 25) and all other patients (n = 634).
DISCUSSION
We found that there was a significant improvement in the overall treatment completion rate of the patients treated at the TBCU after the implementation of the ‘DOT & Shop’ scheme. We also found that the rate of treatment completion for patients enrolled in the scheme was significantly higher than that for those who were not enrolled, and that the proportion of patients who were placed under the ID Act was lower after the implementation of the scheme. In the present study, patients who were younger, of Malay ethnicity and/or unemployed were found to be more likely to be non-adherent to DOT.
Completion of TB treatment is a major goal of any public health programme. TB patients on DOT with any type of incentive are more likely to complete treatment than those on DOT without incentives, and patients on DOT are more likely to complete treatment than those on self-administered therapy.(5-10) Non-adherent patients are more likely to fail treatment, develop drug resistance, take a longer time to convert their bacteriological status, transmit the disease and relapse.(22-24) The use of incentives in TB treatment is a crucial public health measure, as it can encourage the completion of treatment and enhance public health programmes. The findings of Davidson et al’s(5) study conducted in New York, United States, support the theory that increasing incentives (i.e. incentives that gradually increase in value, as they are distributed in a progressive manner with a bonus at the end of treatment) improved adherence to treatment; they found that there was a direct relationship between patient adherence and completion of treatment (p = 0.016). In the present study, a similar incentive scheme model was applied. However, the use of cash incentives is controversial.(12-15) In Tulsky et al’s study,(15) homelessness, alcoholism and drug abuse were identified as reasons for poor adherence, and cash incentives were found to be more effective than non-cash incentives in improving treatment adherence in these patients. Nevertheless, like Bock et al,(7) we opted to use non-cash grocery vouchers instead of cash incentives. This is because patients may use the cash incentives to buy alcohol and/or cigarettes, which may adversely affect treatment outcome. In Bock et al’s inner-city study conducted in the United States,(7) the use of USD 5 grocery coupons as an incentive for a group of non-adherent patients significantly increased treatment completion rate (89%), compared with a historic control group of similarly non-adherent patients who did not receive the incentive (52% treatment completion rate). In the present study, the ‘DOT & Shop’ scheme improved treatment completion rate from 85.3% to 87.2%. It is very likely that the increase in the treatment completion rate of the present study was not as large as that of the aforementioned study because the patients in the present study were not a select non-adherent group. Wei et al(12) found that when poor, migrant patients with TB in a Shanghai district were given financial incentives, TB treatment completion rates significantly improved by 11% (from 78% to 89%). The use of modest incentives via a structured programme has been proven to improve the effectiveness of public health interventions conducted in poor, urban populations.(5,13-14)
Compared with all TB patients in Singapore, male patients and patients of Malay ethnicity were disproportionately represented among the patients in the ‘DOT & Shop’ scheme in the present study. In 2012, 64% of notified TB patients in Singapore were male and 21.6% were Malays;(25,26) in the ‘DOT & Shop’ scheme in the present study, 80.3% of the patients were male and 38.1% were Malays. In most countries, TB notification is twice as high in men as in women.(27) This gender bias has been attributed to genuine biological differences between male and female (in terms of their susceptibility to Mycobacterium tuberculosis infection and the development of TB disease) and not to differential access to healthcare.(27) The PCI of the patients in the ‘DOT & Shop’ scheme was low as compared with the median PCI of Singaporeans (i.e. SGD 2,127); this is not unexpected, given that in order to qualify for enrolment into the scheme, the patients had to have a PCI of less than SGD 900. It is also not unexpected that the Malays were overrepresented in our cohort of TB patients; based on the findings of Lim et al’s study,(28) TB rates were increasing in the Malay population, and Malay TB patients were more likely to reside in low-cost housing, have increased socioeconomic risk factors for TB transmission and be incarcerated. However, the magnitude of the percentage of persistently non-adherent patients who were Malays (64.0%, 16/25) was unexpected. Further studies should be performed to determine whether sociocultural factors account for this observation.
Most of the patients in the ‘DOT & Shop’ scheme informed our MSWs that the grocery vouchers were beneficial and a good motivator for them to follow through with treatment. Even though the incentives were generally effective, 3.8% (25/659) of the patients in the ‘DOT & Shop’ scheme persistently missed doses and were taken off the scheme. The treatment completion rate among these persistently non-adherent patients was only 16.0%. The reasons for non-adherence to TB treatment include economic reasons, healthcare provider failure and deeply held cultural beliefs.(29-31) In the present study, the reasons cited included work commitments and feeling unwell. Previous studies conducted in Singapore have shown that patients of Malay and Indian ethnicities were more likely to interrupt their treatment, and thus have poorer treatment completion rates.(28,32,33) Rubel and Garro(31) coined the phrase ‘health culture of patients’ in reference to the understanding and information (regarding the nature of a health problem, its causes and implications) that patients acquire from family, friends and neighbours. Cultural factors are associated with misinformation about the medical aspects of TB and the stigmatisation of patients with TB. Knowledge of the health culture of patients and an awareness that the health culture of patients may differ from that of healthcare workers (HCWs) is critical if TB programmes are to be successful.(34-36)
The present study was not without limitations. First, to compare treatment completion rates before and after the implementation of the incentive scheme, historical controls were used. They are less reliable than controls obtained from randomised controlled trials, as changes may have occurred in TB epidemiology, diagnosis, supervision and surveillance monitoring. However, the diagnostic methods and surveillance monitoring in the two cohorts (before and after implementation of the ‘DOT & Shop’ scheme) did not change, apart from the following: (a) the increased incidence of Malays with TB over the period of the present study; (b) the implementation of the ‘DOT & Shop’ scheme; and (c) the improved supervision of TB patients with the introduction of the scheme. Second, the incentive scheme was not fully taken up; in some years, when the outcome data were determined (on a quarterly basis), less than 50% of eligible patients were enrolled. Some patients were not identified by the HCWs and MSWs, and others declined further financial assessment and means testing. We were unable to compare the outcomes of the low-income patients who were and were not enrolled in the ‘DOT & Shop’ scheme, as there was no systematic capture of the PCIs of all patients treated at the TBCU. Third, the non-adherent patients were directly asked for their reasons for missing DOT. As such, they may not have been forthcoming about the real reason (e.g. if the HCW’s behaviour was the cause) and the reasons given could not be validated.
No fixed set of incentives and enablers is likely to be appropriate, feasible or effective across all countries or programmes. Documented evidence indicate that incentives and enablers that are directly linked to measurable performance improvements may be more effective than those that are not linked.(37,38) In the present study, only 52.7% of the TBCU patients residing in 1–2-room HDB flats were enrolled in the incentive scheme. Thus, it may be beneficial to increase the PCI threshold and to assign a case manager to each patient.(39) To optimise accessibility, opening DOT centres in neighbourhoods where patients live, with opening hours that are compatible with their work schedules, can be considered. As of 1 April 2014, TB patients managed at the TBCU have benefited from an increased government subsidy. Outreach DOT, a programme in which nurses go to the homes of frail elderly patients with TB, was implemented in 2013. It is hoped that these measures will improve patient adherence to DOT.
ACKNOWLEDGEMENTS
We thank SATA CommHealth for sponsoring the grocery vouchers. We are grateful to our medical social workers, especially Regina M DeSilva, and all DOT nurses at the polyclinics for their dedication and care of patients.


