Abstract
Paediatric gastroenterology in Singapore began in the 1970s. Led by Professor Phua Kong Boo and Professor Quak Seng Hock, paediatric gastroenterology has enjoyed significant strides in the areas of diagnostics, interventions, patient care and research. Several advances such as endoscopy, parenteral nutrition and liver transplantation are well established. The first paediatric small bowel transplant is anticipated in the next decade. Robust research activities have ensured the generation of local data on gastrointestinal disorders. One such research led to the discovery of the changing trends in the incidence of inflammatory bowel disease among the paediatric population in Singapore. The impact of the nation’s paediatric gastroenterology extends internationally, with the notable involvement of Professor Phua in developing the rotavirus vaccine trials and other ongoing collaborative work with international centres. This review explores the history of paediatric gastroenterology from its origins to its remarkable transformation over the decades as centres of excellence in the region.
THE BEGINNING OF PAEDIATRIC GASTROENTEROLOGY
The last few decades have witnessed a remarkable development of paediatric medicine in Singapore, particularly with the rapid establishment and evolution of paediatric subspecialties including paediatric gastroenterology. Paediatric care in Singapore first began in the 1950s at the Singapore General Hospital, following the building of a children’s wing with 280 beds. This was made possible by the generous donation of a philanthropist, Mr NR Mistri.(1) The building, known as the Mistri Wing, consisted of the West Wing housing the University department and the East wing housing the government department of paediatrics. In the early years, children admitted there were cared for by general paediatricians, who managed all their medical conditions. However, the beginning of the 1970s saw a keen interest in developing subspecialist care, as more clinicians and patients appreciated its value. Two eminent paediatricians, namely Professor Phua Kong Boo from the East Wing and Professor Quak Seng Hock from the West Wing, are undoubtedly the pioneers of paediatric gastroenterology.
Professor Phua Kong Boo started providing focussed gastroenterology care following his fellowship at renowned teaching hospitals in Sydney and Melbourne in 1976. Paediatric gastroenterology service under Professor Phua, together with the rest of the department, relocated to KK Women’s and Children’s Hospital (KKH) in 1997. Professor Quak Seng Hock received his fellowship training at Birmingham Children’s Hospital in 1983 and 1989. He subsequently headed the paediatric gastroenterology and hepatology department at the National University Hospital (NUH). With the inception of these two departments, the specialty has seen remarkable growth in both services and technological advances over the last 50 years.
Paediatric gastroenterology remains one of the broadest subspecialties, as it encompasses gastrointestinal (GI), nutrition and hepatology conditions. Various techniques have been developed to aid in disease diagnoses. This article aims to highlight the key areas of development in this field over the last few decades.
DEVELOPMENT OF PAEDIATRIC ENDOSCOPY
Several diseases of the GI tract require mucosal biopsies for diagnostic and therapeutic purposes. Conditions such as celiac disease, inflammatory bowel disease (IBD), eosinophilic GI disease and peptic diseases are typically diagnosed based on specific macroscopic appearance of the gut mucosa and histological features.
The Crosby capsule, invented by William Crosby in 1957,(2) gained wide acceptance as a reliable method for obtaining gastric and intestinal biopsies in adults in the late 1960s in Singapore. The capsule is first attached to a long tube and swallowed by the patient. Once it reaches the desired area of the stomach or bowel, suction is applied, which triggers a spring-loaded knife to obtain the biopsy tissues. Over time, the Crosby capsule was deemed too big for safe biopsies in children and was replaced by the smaller Watson capsule in the 1960s.(3)
The Watson capsule was first used in Singapore by Professor Phua in the 1970s (
Fig. 1
Photograph shows the Watson capsule that was used for small intestinal biopsy in the 1970s (courtesy of Prof Phua Kong Boo).
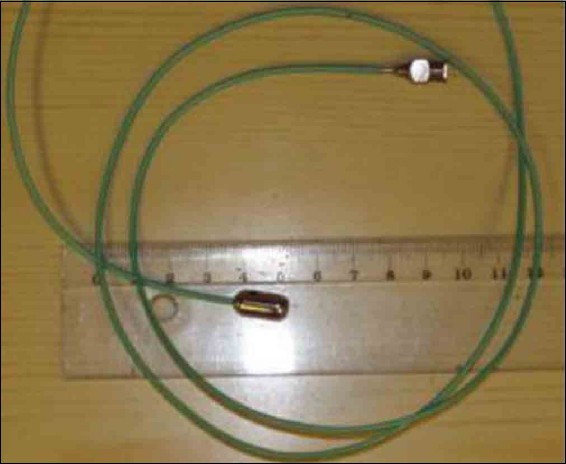
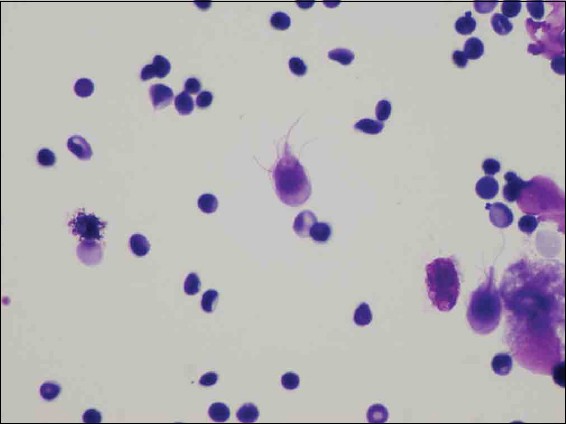
Fig. 2
Photomicrograph shows giardiasis diagnosed using the Watson capsule.
The early 1990s saw the advent of gastroscopy and colonoscopy, which enable gastroenterologists to have a direct vision of the GI tract and perform biopsies for histology. Luminal endoscopy has replaced capsule biopsy and transformed paediatric gastroenterology practice by allowing rapid and accurate diagnosis of various GI conditions such as peptic diseases, celiac disease, inflammatory bowel disease, GI infections, intestinal polyps, etc.(4,5) Initially, gastroscopy and colonoscopy in children were performed by adult gastroenterologists owing to a lack of trained paediatric endoscopists. Professor Quak Seng Hock was the first paediatric gastroenterologist in Singapore to perform these procedures in children from as early as 1982. The first endoscopy was performed in the treatment room in Ward 32 at Mistri Wing. In 1990, Dr Ooi Boo Chye started performing GI endoscopies in Paediatric East after his return from The Royal Children’s Hospital Melbourne. Initially, only a few cases were observed per month; however, the caseloads have increased steadily over the years, with hundreds of endoscopies performed annually.
Wireless video capsule endoscopy is a new technology developed in 2001 to explore the small intestine.(6) This technique is used in case of occult GI bleed, unexplained iron deficiency anaemia, small bowel Crohn’s disease and small bowel polyps, and it has been performed in children for evaluation of small bowel pathology from the early 2010s in Singapore.(7)
MOTILITY DISORDERS, IMPEDANCE pH MONITORING AND GI MOTILITY INVESTIGATIONS
Although gastroesophageal reflux is common in infants, gastroesophageal reflux disease (GERD) is much less common in healthy children. By contrast, preterm infants and children with neurological impairment experience significant complications from GERD, including pulmonary aspiration, apnoea and poor nutrition.(8) The last decade has witnessed rapid development in diagnostic modalities for GI motility disorders including GERD.
Impedance-pH study remains the gold standard diagnostic tool for paediatric GERD. This tool correlates reflux occurrences with clinical events such as desaturation, cough and apnoea. Appropriate management plans are subsequently formulated based on the study results. Impedance-pH study has been conducted in children and infants since the early 2010s and is now the mainstay diagnostic tool for GERD. Other motility investigations such as manometry studies are performed in conjunction with adult gastroenterologists for indications such as achalasia and gut dysmotility.
DEVELOPMENT OF PARENTERAL NUTRITION SERVICES IN CHILDREN
Parenteral nutrition (PN), also widely known as total parenteral nutrition (TPN), involves provision of nutrition to a patient via the parenteral route. TPN is indicated when a patient is unable to meet his or her nutritional requirements by the enteral route alone owing to his or her clinical conditions. Dudrick et al(9) first introduced the concept of TPN in the 1960s by successfully administering intravenous nutrition to an infant.
TPN in children was first started in the 1970s by Professor Wong Hock Boon and Professor Phua Kong Boo at the Mistri Wing. They published a report of 12 infants with malignant diarrhoea who were successfully treated with PN.(10) In this study, intravenous access was obtained using a scalp vein needle. Instead of the commercial intralipid, post-prandial plasma was harvested and used as a source of lipids. Protein was provided by an essential amino acid infusion known as Sohamin (Tanabe Seiyaku, Japan). The final component of the PN, which was prepared and administered to the infants by nursing staff, was 10% glucose.
To date, TPN provision for children with various medical or surgical conditions has been well established. The last few decades have also seen improved survival of patients with short-gut syndrome and intestinal failures owing to advances in surgical techniques and administration of TPN. Hence, the nutrition support team at KKH was formally established to provide multidisciplinary care to these patients in the early 2010s. The team consisted of paediatric gastroenterologists, dieticians, TPN pharmacists, nutritional support nurses and paediatric surgeons. Most patients received only short-term TPN support; however, certain patients with intestinal failure would require long-term TPN. For this purpose, the KKH Intestinal Rehabilitation Programme was established in 2014. Under this programme, wherever possible, patients were transitioned to home PN following intensive training by the nutrition support team.
Small bowel transplantation is a recognised treatment for patients with intestinal failure who develop complications due to long-term TPN.(11) Paediatric small bowel transplantation programme is currently at the planning stage in Singapore. The transplant team, comprising paediatric gastroenterologists, surgeons, intensivists, pharmacists and nurses recently went on training attachments to overseas transplant centres supported by the Human Manpower Development Plan grant. It is envisioned that the first paediatric small bowel transplant in Singapore will be performed in the next five to ten years.
RAPID RISE OF PAEDIATRIC INFLAMMATORY BOWEL DISEASE IN SINGAPORE
IBD, Crohn’s disease, ulcerative colitis and IBD unclassified are chronic inflammatory conditions of the GI tract. Their aetiology is multifactorial, involving genetic predisposition, environmental factors, intestinal microbiome and immune dysregulation.(12) Historically, IBD was considered a disease of affluent Western countries. However, in recent years, the incidence rate of IBD has plateaued in Western countries, and a rising incidence has been observed in Asia.(13,14) Singapore has also witnessed a rapid rise in the incidence of paediatric IBD over the last three decades. A recent publication on the epidemiology of paediatric IBD in Singapore over a 22-year period showed an overall incidence of 1.26 per 100,000 individuals. During the first decade (1994–2004), the incidence of IBD was 0.23 per 100,000 individuals, which increased almost 10-fold to 2.28 per 100,000 individuals during the second decade (2005–2015). Additionally, paediatric IBD in the Singapore cohort had a more aggressive phenotype than that observed in Western data.(15)
Specialised multidisciplinary paediatric IBD clinics (comprising gastroenterologists, IBD nurses, dieticians and social workers) were established to provide care to paediatric patients with IBD since the early 2010s. Patients who reached adolescence were transitioned to the care of adult IBD physicians in a systematic manner via specialised transition clinics established in 2016. A national database for paediatric patients with IBD and collaborative work with other countries has been developed to better characterise disease phenotype and encourage future research in this area.
ADVANCES IN HEPATOLOGY
The last five decades have seen significant advances in the care of paediatric liver diseases in Singapore. This section will highlight the development of hepatology services and technological advances. Neonatal jaundice is a common condition affecting 50% of term and 80% of preterm infants.(16) Phototherapy is the recognised mainstay treatment for neonatal jaundice. Before phototherapy was discovered, babies with jaundice were exposed to early morning sunlight at the hospital attics in KKH. The first phototherapy for neonatal jaundice was performed in 1975 and it has since been well established in hospitals nationwide.
Singapore was an endemic region for hepatitis B infection, with a hepatitis B carriage rate of around 5%–6%.(17) Hepatitis B vaccination has drastically altered the epidemiology of hepatitis B infection in the population.(17) The vaccination was offered to neonates whose mothers were hepatitis B carriers from October 1985 and to all neonates from September 1987. Hepatitis B immunoglobulin was first introduced around 2005 to infants whose mothers were hepatitis B carriers.
BA is preponderant among the Asian population, and Kasai portoenterostomy is a well-established first-line treatment option. Chiang et al(18) reported the outcome data of 58 infants with BA who were treated from 1997 to 2013 at KKH. The majority of these infants had undergone Kasai portoenterostomy. Outcomes, as measured by survival of native liver at two and five years of age, were comparable to those reported by major centres internationally.
The first paediatric liver transplantation was performed in 1991 at NUH. To date, the well-established National Liver Transplant Programme in NUH has covered over 140 paediatric liver transplantations.
TECHNOLOGICAL ADVANCES IN THE DIAGNOSIS OF LIVER DISEASES
As percutaneous liver biopsy allows for histological diagnosis, it remains the gold standard for evaluation of hepatic diseases.(19-21) This procedure was traditionally performed using a ‘blind’ percussion technique. In recent years, imaging assistance has been shown to reduce complication rates and increase the likelihood of obtaining adequate sampling.(22) Ultrasound-guided liver biopsies are currently the investigative modality of choice, as opposed to the percussion technique.
Transient elastography (also known as FibroScan) is a recognised and well-established bedside method to measure liver fat deposition and stiffness in the liver without the need for liver biopsy.(23) In recent years, this technique has been increasingly performed to monitor liver fibrosis and steatosis in children with chronic liver diseases such as non-alcoholic fatty liver disease, BA and hepatitis B infection.
MULTIDISCIPLINARY TEAMS FOR MANAGEMENT OF COMPLEX GASTROINTESTINAL CONDITIONS
A multidisciplinary approach to patient care has long been established as one of the best models of care. Over the last 50 years, the paediatric gastroenterology departments at both KKH and NUH have witnessed a steady increase in the number of multidisciplinary teams and clinics. These services include: (a) the multidisciplinary feeding clinic (comprising gastroenterologists, speech therapist, dieticians and psychologists) set up for the management of children with feeding difficulties; (b) liver disease clinic (comprising paediatric surgeons and hepatologists) for the management of complex hepatology conditions; (c) multidisciplinary inflammatory bowel disease clinic; (d) metabolic liver disease clinic (comprising hepatologists and geneticists); (e) eosinophilic gastrointestinal disease clinic (comprising gastroenterologists, allergists and dieticians); and (f) nutrition support team for the management of children on long-term TPN.
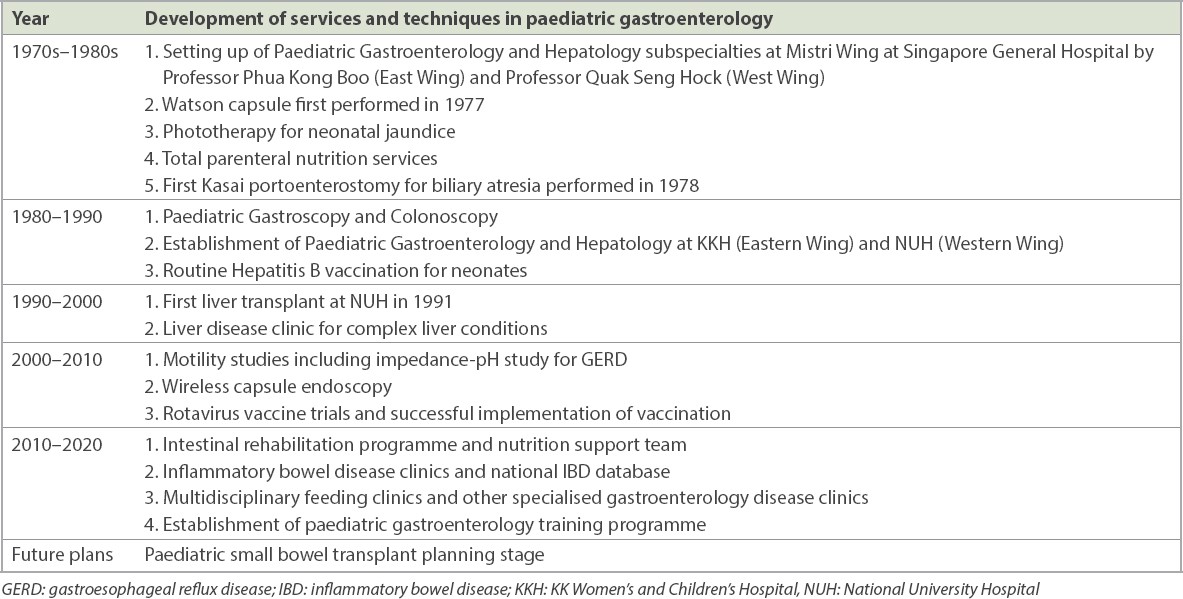
Table I
Journey of paediatric gastroenterology in Singapore over the last five decades.
RESEARCH ADVANCES IN PAEDIATRIC GASTROENTEROLOGY
With the rapid development of services at the two centres, research in paediatric gastroenterology has begun to take centre stage in recent years. Prestigious research grants, including National Medical Research Council grants and SingHealth Foundation grants, have been awarded to researchers within the specialty. The number of publications in peer-reviewed journals has also increased steadily over the years, with more than 200 publications to date. While it is beyond the scope of this article to delve into the many distinguished publications, the authors wish to highlight notable research by the pioneers of the specialty.
Professor Phua Kong Boo has made significant contribution to the prevention of rotavirus in children. He was the lead researcher in the development of the rotavirus vaccine RIX4414 (Rotarix) during Phase 2 and Phase 3 trials. The team recruited more than 10,000 infants in the vaccine trials, which demonstrated a high efficacy rate of 96.1% (95%CI: 85.1%, 99.5%) against severe rotavirus gastroenteritis up to two years of age.(24,25) The vaccine also has a good safety profile and is currently a part of routine vaccination for infants in Singapore and internationally.
Professor Quak Seng Hock is an avid researcher who has published widely in peer-reviewed journals. One of his notable research areas was GERD. His team at NUH demonstrated the efficacy of low-dose erythromycin in reducing GERD among preterm infants in a double-blind, randomised control trial.(26) Hence, low-dose erythromycin is a well-recognised therapeutic option for GERD and other gut dysmotility conditions.
TRAINING OF PAEDIATRIC GASTROENTEROLOGISTS
Both Professor Phua and Professor Quak started their careers as general paediatricians having a personal interest in gastroenterology, and would manage patients with more complex gastroenterological conditions. Following their return from fellowship training in the United Kingdom and Australia in the 1970s and 80s, they introduced specialised gastroenterology services, as detailed in earlier sections of this article. They trained rotating residents and developed the workforce by admitting interested trainee registrars into the service. There were no formal training programmes during those days, and trainees obtained the required knowledge through hands-on experience and in-service training.
In the 1980s, the Ministry of Health set up a Health Manpower Development Programme. This sponsored programme provided an opportunity for trainee registrars to further hone their skills and expertise through attachments at reputable overseas centres. In 2015, a structured paediatric gastroenterology subspecialty training programme was introduced in Singapore. This allows trainees who have completed the Paediatric Medicine Residency Training programme to receive sub-specialty training in the fields of paediatric gastroenterology, hepatology and nutrition. Upon fulfilling all the requirements of the two-year programme, the trainee would have to pass the exit examination to become an accredited paediatric gastroenterologist. Since 2015, three trainees have entered the subspecialty training programme.
CONCLUSION
Since its inception at the Mistri wing of Singapore General Hospital, paediatric gastroenterology has evolved tremendously along with the growth of medical services, technological advances, research and international collaboration under the leadership of its pioneers. The establishment of paediatric gastroenterology as a subspecialty has led to better patient care, especially with the adoption of the multidisciplinary care model. With constantly emerging therapies, interventions and insight into disease states, further exciting progress in this specialty is anticipated. Continued efforts in implementing the best models of care, keeping abreast of therapeutic advances and robust research will ensure that Singapore’s paediatric gastroenterologists continue to improve the lives of children with GI disorders.


