Abstract
INTRODUCTION
Total knee arthroplasty (TKA) is an effective method for alleviating pain and restoring knee function in patients with severe osteoarthritis. However, despite the improvements in surgical technique and postoperative care, it has been reported that up to 19% of patients are dissatisfied after their operations. The aim of this study was to evaluate patient satisfaction levels after TKA in an Asian cohort, as well as assess the correlation between patient satisfaction levels and the results of traditional physician-based scoring systems.
METHODS
The medical data of 103 Asian patients who underwent 110 TKAs between December 2008 and June 2009 were obtained from our hospital’s Joint Replacement Registry. The minimum follow-up period was one year and patient expectations were assessed before TKA. Patient satisfaction was assessed postoperatively using a 5-point Likert scale. Reasons for patient dissatisfaction were recorded. Standardised instruments (e.g. the Knee Society Score, the Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC] and the generic Short Form-36 health survey) were used to assess the patient’s functional status and the severity of symptoms pre- and postoperatively.
RESULTS
Among the 110 TKAs performed, 92.8% resulted in patient satisfaction. Patient satisfaction correlated with postoperative WOMAC function scores (p = 0.028), postoperative WOMAC final scores (p = 0.040) and expectations being met (p = 0.033).
CONCLUSION
Although there was a high level of patient satisfaction following TKA in our cohort of Asian patients, a significant minority was dissatisfied. Patient satisfaction is an important outcome measure and should be assessed in addition to traditional outcome scores.
INTRODUCTION
Osteoarthritis of the knee is a relatively common condition that affects approximately 10% of the general population above the age of 55 years.(1) The later stages of osteoarthritis of the knee can be debilitating due to pain and a decrease in the functional range of motion.(2-4) While many methods of treatment have been developed to address this condition,(5) joint replacement is the definitive treatment of choice. Total knee arthroplasty (TKA) is an effective way to manage end-stage knee osteoarthritis, as it has been shown to alleviate pain and improve function.(6-11) Over the years, many refinements have been made to this surgical procedure to improve patient outcomes, reduce postoperative complications and, ultimately, improve the patient’s quality of life.(8)
Traditional standardised instruments such as the Knee Society Score (KSS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) are often used to assess patient outcomes following TKA. These instruments assess patient function and residual pain, along with more objective factors, such as the range of motion of the knee. However, several authors have highlighted that it is important to include patient-reported outcomes when evaluating TKA success, as there is discordance between the outcomes assessed by clinicians (using these traditional standardised instruments) and those reported by patients.(12,13)
Patient satisfaction is influenced by many factors, such as the presence of residual pain,(7,14) postoperative functionality(7,14) and the presence of postoperative complications.(15-17) Patient dissatisfaction has been reported to be as high as 19% among patients who have undergone TKA.(15) Patient expectations prior to TKA have also been identified as an important factor in determining postoperative satisfaction.(15,18-20) In addition, patient expectations can often be influenced by anecdotal evidence from friends and family members who have undergone TKA.
Much of the published data regarding patient satisfaction has been obtained from studies conducted on Western populations; however, there is a paucity of such data from Asian populations. Therefore, the present study aimed to evaluate the level of patient satisfaction after TKA in an Asian population. We also aimed to identify the reasons for patient dissatisfaction after TKA and assess the correlation between patient satisfaction and traditional physician-based scoring systems. Our findings will provide objective data that can be used in preoperative patient counselling.
METHODS
Patients who underwent TKA for late-stage osteoarthritis of the knee between December 2008 and June 2009 in the National University Hospital, Singapore, were included in this study. Patients who had rheumatoid arthritis of the knee, posttraumatic osteoarthritis, gout and other inflammatory arthritic conditions were excluded. The minimum follow-up period was one year. Prophylaxis against deep vein thrombosis for all patients consisted of mechanical prophylaxis, in the form of thromboembolic deterrent stockings, and early mobilisation (range of motion exercises by the first postoperative day and ambulation by the third day). Chemoprophylaxis was not routinely administered. Patient data, including demographic details, pre- and postoperative knee pain and function as well as postoperative complications, was obtained from the hospital’s Joint Replacement Registry.
Patient expectations were assessed by giving patients a choice of one or more of several responses, including improved mobility, reduced pain and better overall quality of life. Standardised instruments, namely KSS, WOMAC scoring system and generic Short Form-36 (SF-36) health survey, were used to assess the severity of symptoms and functional statuses of the patients pre- and postoperatively. KSS was chosen as it is an extensively validated method for measuring knee function (pain, stability and range of motion) and patient functional outcomes. The WOMAC scoring system was used to measure pain, stiffness and functional limitation. The scoring systems were administered before and one year after the operation. Patients were also asked if their preoperative expectations had been met.
Data collected was analysed against patient satisfaction, which was measured on a 5-point Likert scale (extremely satisfied, satisfied, neutral, dissatisfied, extremely dissatisfied). Based on the responses, the patients were categorised into the ‘satisfied’ (answered ‘extremely satisfied’ or ‘satisfied’) or ‘dissatisfied’ (answered ‘neutral’, ‘dissatisfied’ or ‘extremely dissatisfied’) group. Patient satisfaction was assessed at the follow-up session one year after the operation. The patients were also asked whether they would recommend the surgery to others and undergo the surgery again.
Data was presented in frequency tables and using descriptive statistics (mean ± standard deviation or median, where appropriate). Categorical variables were presented as proportions, while continuous variables were presented as median values. Chi-square and Fisher’s exact tests were used to compare categorical variables, while student’s t-test was used for continuous variables. Statistical significance was set at p-value ≤ 0.05. Data analysis was performed using the Statistical Package for the Social Sciences version 17 (SPSS Inc, Chicago, IL, USA). Ethical approval was sought and obtained from the licensing institution of our hospital’s healthcare cluster, the Domain Specific Review Board.
RESULTS
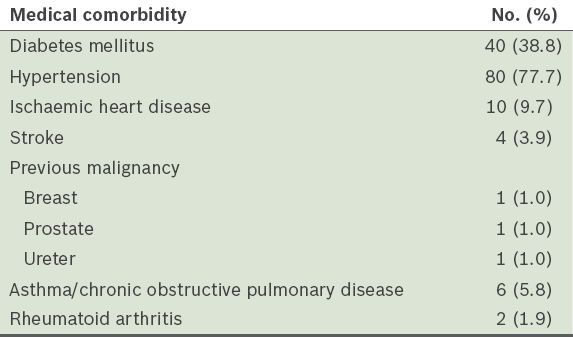
A total of 103 patients met the inclusion criteria of the study and 110 TKAs (96 unilateral and 7 bilateral TKAs) were performed. Of the 110 TKAs, 78 (70.9%) were performed on female patients and 32 (29.1%) on male patients. The median age of the patients was 64 (range 45–83) years, and the mean body mass index (BMI) was 26.7 (range 17.3–42.2) kg/m2. The medical comorbidities of these 103 patients are shown in
Table I
Medical comorbidities of the patients (n = 103).
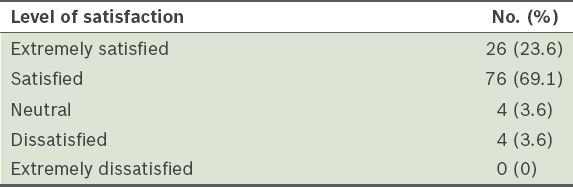
Of the 110 TKAs performed, 102 (92.8%) were reported to be satisfactory. In each of their TKAs, most of the patients reported that they would recommend the procedure (101/110 TKAs, 91.8%) and undergo TKA again (89/110 TKAs, 80.9%). The proportion of TKAs for each level of patient satisfaction is shown in
Table II
Proportion of total knee arthroplasties for each level of patient satisfaction (n = 110).
A total of 5 (15.6%) male patients and 3 (3.8%) female patients were categorised in the ‘dissatisfied’ group following TKA. Gender was not found to be statistically significant in predicting patient dissatisfaction (p = 0.296). The mean age of patients in the ‘dissatisfied’ group was slightly higher than that of those in the ‘satisfied’ group (67.9 years vs. 64.8 years), and the mean BMIs of the patients in the two groups were largely similar (27.4 kg/m2 vs. 27.6 kg/m2). Neither mean age nor mean BMI was significant in predicting lower patient satisfaction (p = 0.332 and p = 0.984, respectively).
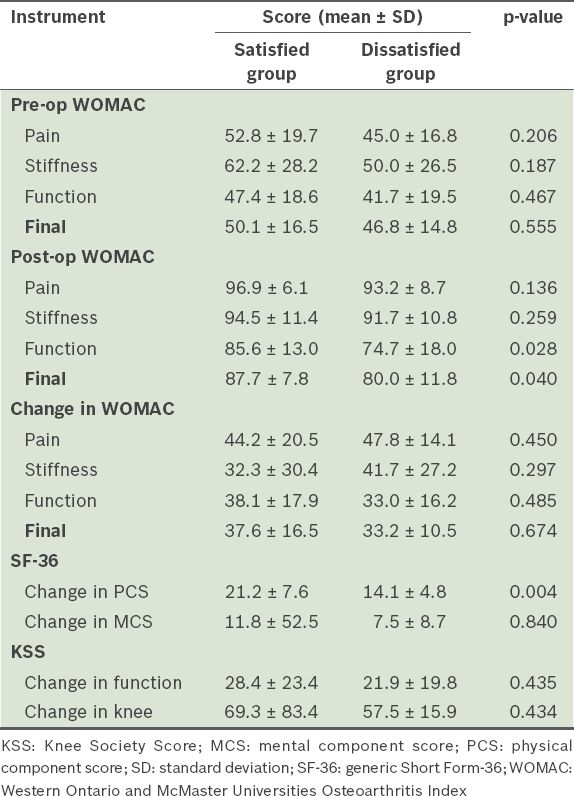
The KSS, SF-36 and WOMAC scores of the patients were analysed. We found that patients who had improved WOMAC function and final scores were significantly more satisfied; however, the postoperative pain and stiffness components of the WOMAC score were not statistically significant for patient satisfaction. Improvements in the physical health component of the SF-36 score correlated well with patient satisfaction, whereas improvements in the mental health component did not. Improvements in KSS were not statistically significant for patient satisfaction. The relationship between patient satisfaction and improvements in the various components of the three scoring instruments is shown in
Table III
Correlation between patient satisfaction and the three scoring instruments.
Patient expectations were assessed before each TKA, and these expectations were expressed in the form of standard response options, including results related to mobility, pain and overall quality of life. Among the patients who underwent TKAs, the following patient expectations were reported: (a) less pain (60/110 TKAs, 54.5%); (b) improved mobility (53/110 TKAs, 48.1%); and (c) improved overall quality of life (36/110 TKAs, 32.7%). These preoperative expectations were met in 106 of the 110 TKAs (96.4%) performed. Preoperative expectations were found to be statistically significant in predicting patient satisfaction (p = 0.033).
In the present study, the following complications were noted among patients who underwent TKAs: (a) distal deep vein thrombosis (6/110 TKAs, 5.5%); (b) proximal deep vein thrombosis (4/110 TKAs, 3.6%); and (c) bilateral pulmonary embolism (1/110 TKAs, 0.9%). The four cases of proximal deep vein thrombosis and the one case of bilateral pulmonary embolism received anticoagulation therapy in the form of low-molecular-weight heparin and warfarin. Among the six cases of distal deep vein thrombosis, two received anticoagulation therapy, one experienced popliteal artery thrombosis (causing an ischaemic limb) and was treated with vascular bypass and fasciotomies, one suffered from an acute myocardial infarction and underwent angioplasty, one developed bradycardia intraoperatively and was managed in the high-dependency unit, and one had a superficial wound infection that was treated with oral antibiotics. Although some patients cited the development of operative complications as a reason for dissatisfaction, it was not found to be significantly correlated with lower patient satisfaction (p = 0.174).
DISCUSSION
Osteoarthritis of the knee is a relatively prevalent condition(1,21) that can progress to a point where it is debilitating.(2) It adversely affects the patient’s quality of life due to pain and decreased function.(3,4) While there are many modes of treatment,(5) including conservative(22-26) and surgical management,(27-30) the definitive method of treatment is joint replacement. In this regard, TKA has been shown to be safe and effective in addressing end-stage osteoarthritis of the knee.(7,30,31) This surgical procedure has become more common(32) due to its effectiveness in alleviating pain and improving function,(7-11,33) and will continue to play a key role in the management of osteoarthritis.
While TKA has been touted as an effective treatment modality,(7,30,34) several studies have reported that not all patients are satisfied after the operation.(14-16,35) Many outcome measures have been used to measure the efficacy of TKA, including subjective methods (e.g. the surgeon inquiring about the patient’s pain and function levels at follow-up visits)(15) and objective scales (e.g. WOMAC, KSS and SF-36 scoring systems).(36,37) The latter has been shown to correlate well with patient satisfaction.(38) Although the use of these scales may indicate improvement in the majority of patients,(14,35) there remains a significant proportion of patients who are dissatisfied with the outcome of the TKA.(14-16,35) In fact, the dissatisfaction rate for TKA has been reported to be as high as 19%.(15) Additionally, it has been suggested that clinician-assessed outcomes may not always match those reported by patients. In other words, there is a need for patient-reported outcomes and satisfaction levels to be included in the routine postoperative assessment of patients who undergo TKAs.
In a study by Yuan et al, which examined the patient outcomes of a group of 60 patients who underwent 74 TKAs, the patient satisfaction rate was reported to be 91%.(16) Nunez et al, in their study involving 112 patients, reported an 86% satisfaction rate.(35) The results of the present study are consistent with these two studies; 93% of our patients expressed that they were satisfied or extremely satisfied with the TKA. Similar to Nunez et al’s study, in which 80% of their patients indicated that they were willing to undergo TKA again,(35) 81% of the patients in the present study expressed willingness to undergo TKA again. Furthermore, 92% of the patients in the present study reported that they would recommend the procedure to others.
Preoperative expectations have been shown to be strongly predictive of postoperative patient satisfaction.(15,18-20) Gandhi et al demonstrated that preoperative expectations of pain relief affected postoperative satisfaction levels,(19) while Mahomed et al showed that expectations of pain relief were related to postoperative function and pain levels.(18) In contrast, the present study showed that the presence or absence of preoperative patient expectations (e.g. improved mobility, reduced pain and better overall quality of life) was not predictive of patient satisfaction. However, the fulfilment of patient expectations was found to be significant in predicting postoperative satisfaction; this finding was in agreement with that of Bourne et al’s study.(15)
Patient satisfaction is affected by many factors, and several studies have analysed the various determinants of patient satisfaction. Factors that have been repeatedly highlighted in the literature include mental health,(14,39-42) preoperative knee function and pain,(40,42,43) postoperative function and pain,(7,14,44) operative complications,(15-17) and the need for revision surgery.(45-47) Other factors are gender,(19,48) age(19,48) and type of knee arthritis.(45,49)
Some studies have demonstrated that poor preoperative WOMAC scores are predictive of lower patient satisfaction levels.(40,43,44) However, Lingard et al found that there was no significant difference in WOMAC function scores between satisfied and dissatisfied patients.(39) The results of the present study support the findings of Lingard et al’s study;(39) preoperative WOMAC scores in our study were not predictive of patient satisfaction (p = 0.555). In addition, absolute changes in SF-36 and KSS scores were not predictive of patient satisfaction. However, good postoperative WOMAC function and overall scores as well as good SF-36 physical component scores were found to be predictive of patient satisfaction.
While a meta-analysis on knee arthroplasty concluded that the complication rate for the procedure was approximately 30%,(50) Yuan et al reported a lower complication rate of 13.5% (complications consisted of common peroneal nerve paralysis, failure of wound union, wound infection, joint infection, knee stiffness, deep vein thrombosis and patellofemoral joint complications).(16) Similar to Yuan et al’s study, the complication rate in the present study was 14.6%, and the complications encountered included thrombotic events, cardiac problems and a single superficial wound infection. Ruban et al reported a 14% rate of deep vein thrombosis following TKA (5% proximal and 9% distal thrombosis).(51) In a study of Singaporean patients undergoing TKA, Nathan et al reported a proximal deep venous thrombosis rate of 4.38%.(52) In the present study, similar rates of deep vein thrombosis were observed (3.6% proximal and 5.5% distal deep vein thrombosis). Yuan et al correlated the development of complications with lower patient satisfaction,(16) and Bourne et al’s findings supported this.(15) However, the present study found that patient satisfaction was not significantly influenced by the development of operative complications (p = 0.174). While some studies correlate the presence of medical comorbidities with a poorer outcome,(40,53) we did not find any such correlation (p = 0.678). As patients are often influenced by anecdotal evidence from friends and family members who have had TKA, it is important that they receive proper preoperative patient counselling. The present study provides objective data that can be used for preoperative patient counselling.
The present study was not without limitations. It had a relatively small sample size of 103 patients undergoing 110 TKAs. Also, while other authors have associated poorer mental health with lower patient satisfaction,(39,40,42) we did not analyse the influence of mental health on patient satisfaction. While our follow-up period was one year following the primary TKA, similar to that of several studies,(15,41,44) there are studies that have a follow-up period of up to seven years,(35) allowing for a more comprehensive view of the patients involved.
To conclude, TKA is an effective treatment modality for end-stage osteoarthritis of the knee, but a significant proportion of patients are not satisfied with their surgery. The present study shows that patient satisfaction is correlated with postoperative WOMAC function and final scores, a change in the SF-36 physical component score and patients’ expectations being met. Patient satisfaction is an important outcome measure and should be assessed in addition to traditional outcome scores. According to the present study, there is a high level of patient satisfaction following TKA in Asian patients.


