Abstract
INTRODUCTION
The purpose of this study was to assess the application of the early warning score system (EWS-S) and gauge physician awareness, perceptions of necessity and attitudes regarding these tools based on previously experienced unnoticed clinical deterioration (CDET).
METHODS
A cross-sectional survey was carried out via an online questionnaire at a large 3,500-bed Class 3A general hospital in China. A total of 299 physicians of adult general wards were asked to answer a translated questionnaire that was localised from the original version. Demographic profiles of patients were included as well as three other sections assessing awareness of CDET/EWS-S and gauging attitudes towards and perceptions of the necessity of EWS-S at our hospital.
RESULTS
A high level of physician awareness of the CDET problem was observed. Most physicians knew about the existence of a systematic assessment tool for clinical application. Physicians with previous experience in reanimation, unplanned transfer to intensive care unit (UTICU) and/or death tended to consider EWS-S necessary in attentive and well-trained staff (p < 0.05). Physicians who had previous experience with UTICU were more likely to recommend implementing EWS-S in their wards compared with those without such experience (p < 0.05).
CONCLUSION
Most physicians have positive attitudes towards EWS-S. However, their awareness should be further heightened. Physicians who had previous experience with CDET/UTICU were more likely to employ EWS-S in their clinical practices. To better facilitate the implementation of EWS-S in Chinese hospitals, existing facilities, policy supports, standardised managements and the development of information systems should be strengthened.
INTRODUCTION
Failure to promptly identify and appropriately manage deteriorating patients may result in severe adverse in-hospital events such as death, cardiac arrest, myocardial infarction, stroke, pulmonary embolism and unplanned transfer to intensive care unit (UTICU),(1) leading to higher morbidity/mortality, longer hospital stay and unnecessary medical costs.(2,3) Such serious adverse events might be prevented by identifying and managing the early signs of clinical deterioration (CDET).(4) Some retrospective studies have indicated that CDET is usually characterised by an extended period of physiological instability.(5) Early identification of CDET translates to better overall outcomes.(6) Over 80% of patients are not observed within 24 hours before the onset of serious adverse events.(7) However, mounting evidence has revealed that warning signs of CDET may sometimes not be recognised and reported because of the limited capabilities of clinical staff, leading to suboptimal care and delayed medical interventions.(8)
To resolve these problems, early warning score systems (EWS-Ss), rapid response teams (RRTs) and patient-at-risk teams (PARTs) have been introduced in the United Kingdom (UK), the United States (US) and Australia.(9) A wide variety of EWS-Ss have been employed to identify CDET by observing different parameters (i.e. single-parameter, multiple-parameter and aggregated systems).(10,11) The early warning score (EWS) uses a simple algorithm based on the physiological measurement of patient vital signs (i.e. heart rate, systolic blood pressure, respiratory rate, temperature and mental status), from which a score is calculated and recorded.(12-14) When an overall EWS rises above a certain level, it prompts healthcare providers to intensify patient care and triggers an RRT/PART for managing these deteriorating patients in a timely manner, thus helping to improve inpatient outcomes.(15) In 2001, the modified early warning score (MEWS) became a simpler and more accurate scoring tool for routine bedside observations.(16) The tool made it clearer and easier for staff to recognise the signs of acute deterioration in patients and provide timely assistance. Other forms of EWS-S tools include the VitalPAC Early Warning Score, Standardised Early Warning Score and National Early Warning Score (NEWS).
Currently, EWS-S has become an excellent tool for predicting adverse events and evaluating patient status and outcomes. Most junior physicians have employed MEWS as a severity score for prioritising clinical tasks. Nurses tend to employ MEWS because it simplifies their clinical dialogues with physicians.(17) Therefore, it is applied widely all over the world. In the UK, application of EWS-S is mandatory.(1,10) In other countries, NEWS has been implemented as a significant stratification tool for admission into acute medical wards.(16) According to a literature review focusing on mainland China, most applications of EWS-S are in prehospital first aid and hospital emergency cases rather than patients in general wards. Furthermore, the lack of standardised management of EWS-S in general wards has been a great barrier to improvement.(13,18)
Since 2016, our hospital took the initiative to apply EWS-S (mainly MEWS) comprehensively in China. It is an ongoing project and staff are trained to do so from early on in their medical training. Because physicians and nurses play vital roles in recognising and handling patient CDET, their awareness, needs and attitudes are crucially important. However, little is known about the awareness, necessity and attitudes towards such tools. In the current study, we sought to provide rationales for continuing improvement programmes and strengthening physician-nurse collaborations by assessing current applications of EWS-S and gauging the awareness, necessity and attitudes of physicians at our hospital.
METHODS
This was a cross-sectional survey of physicians using a self-administered questionnaire conducted in March 2019 at a large 3,500-bed Class 3A general hospital that undertakes medical treatment, education and research. Since 2016, our research-oriented hospital has pioneered the application of MEWS in adult general wards in mainland China.
The questionnaire was translated from its German version by a professional translator.(1) There were minimal changes to the wording of the questions, different study sites and item sequences. Our institutional EWS-S experts double-checked the quality of the translations. Section I consisted of basic profiles, including years of practice, job titles and work specialty. The questions in Section II were formulated to explore awareness of existing CDET problems (four items). Answers were coded on a 4-point Likert scale (1 = fully agree, 2 = rather agree, 3 = rather not agree, 4 = do not agree). Two advanced questions were as follows: ‘How many cases have you experienced during the last 12 months when unnoticed or late-noticed deterioration of a patient led to an unplanned transfer to ICU (intensive care unit)?’, and ‘How many cases have you experienced during the last 12 months of unnoticed or late-noticed deterioration of a patient leading to death?’ The perceived frequencies were assessed and categorised as follows: 0, 1–2 cases, 3–5 cases, 6–10 cases or > 10 cases. Section III covered whether or not EWS-S was known (three items). In Section IV, attitudes towards early recognition of CDET and EWS-S were assessed: five items assessed more general statements regarding early recognition of CDET, another ten items focused on specific attitudes towards EWS-S, and two items assessed the perceived utility and necessity of EWS-S for the participants’ own clinical tasks. Answers were coded on a 4-point Likert scale (1 = fully agree, 2 = rather agree, 3 = rather not agree, 4 = do not agree). The Cronbach’s alpha of the questionnaire was 0.72.
Convenience sampling was used. The required sample size was 5–10 times of the number of included items. As there were 28 items in the current study, at least 140–280 participants were needed. The questionnaire was emailed to 1,000 physicians, who were provided with an individual link to an online survey. Physicians who worked in the emergency department, ICU and paediatric ward were excluded from the study. A total of 299 physicians participated, yielding a response rate of 29.9%.
Descriptive statistics were expressed as mean ± standard deviation or percentages. To test differences in attitudes towards EWS-S between chief physicians with and without prior experiences of UTICU, reanimation and/or death from CDET, an independent t-test, chi-square test or Fisher’s exact test was used, as appropriate. All analyses were performed using IBM SPSS Statistics version 25.0 (IBM Corp, Armonk, NY, USA). A one-sided p-value < 0.05 was deemed statistically significant.
According to Chinese law, this survey did not require formal approval by an ethics committee. The participants consented to their participation, and their anonymity was emphasised. Records were processed anonymously, and the recordings were accessible only to the researchers.
RESULTS
Among the participants, 68 (22.7%) had practiced for ≤ 2 years, 59 (19.7%) for 3–5 years, 66 (22.1%) for 6–10 years and 106 (35.5%) for > 10 years.
Table I
Demographic profiles of the participants (n = 299).
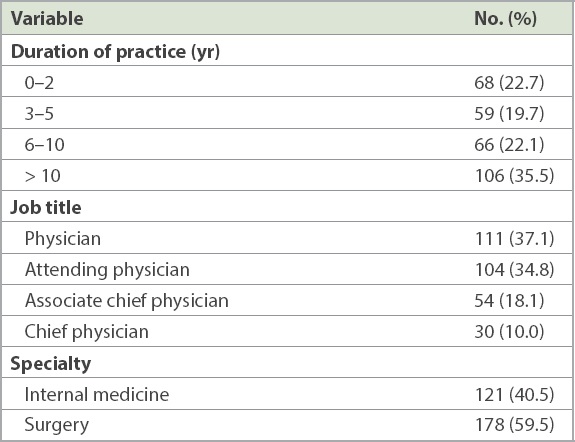
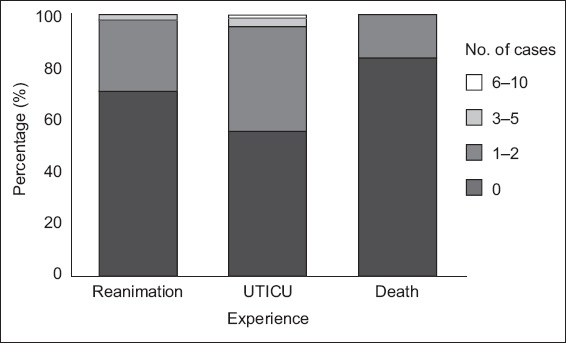
Fig. 1
Chart shows the frequency of cases of unnoticed clinical deterioration of a patient during the past 12 months, leading to unplanned transfer to intensive care unit (UTICU), reanimation or death of the patient.
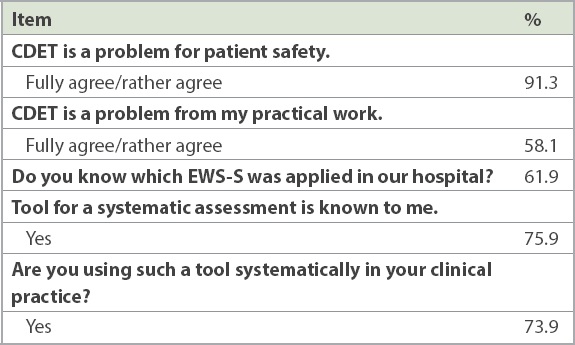
Awareness of the problem of CDET was described by 91.3% of the physicians; 58.1% considered it a clinical problem, while 61.9% of the physicians considered MEWS to be a tool for systematically assessing CDET. The usefulness of such a systematic assessment tool was apparent for 75.9% of the physicians, and 73.9% reported using it clinically (
Table II
Awareness of the problem of unnoticed clinical deterioration (CDET) and knowledge about early warning score systems (EWS-S) (n = 299).
Physicians who had previous experience with reanimation, UTICU and/or death were significantly more likely to report CDET as a clinical problem (p < 0.001) and tended to agree that EWS-S remained necessary in attentive and well-trained staff (p < 0.001). Of the respondents, 281 (96.6%) considered EWS-S to be a good measure for enhancing patient safety; 275 (94.5%) regarded EWS-S as useful for systematically recognising any deterioration of patients’ general condition; and 271 (93.1%) assumed that EWS-S should be used systematically in all wards. However, 212 (72.9%) respondents judged EWS-S to be too time-consuming and 201 (69.1%) considered it to be disproportionately inflating the workload of nurses. Despite this, 260 (89.3%) felt that EWS-S might guide nurses’ decisions regarding whether or not to inform physicians about CDET, and 273 (93.8%) agreed that EWS-S could assist physicians in properly evaluating nurses’ feedback and responding promptly (
Table III
Awareness and attitudes towards the early warning score system (EWS-S), as stratified by cases during the past 12 months, unnoticed clinical deterioration (CDET) leading to unplanned transfer to intensive care unit (UTICU), reanimation or death.
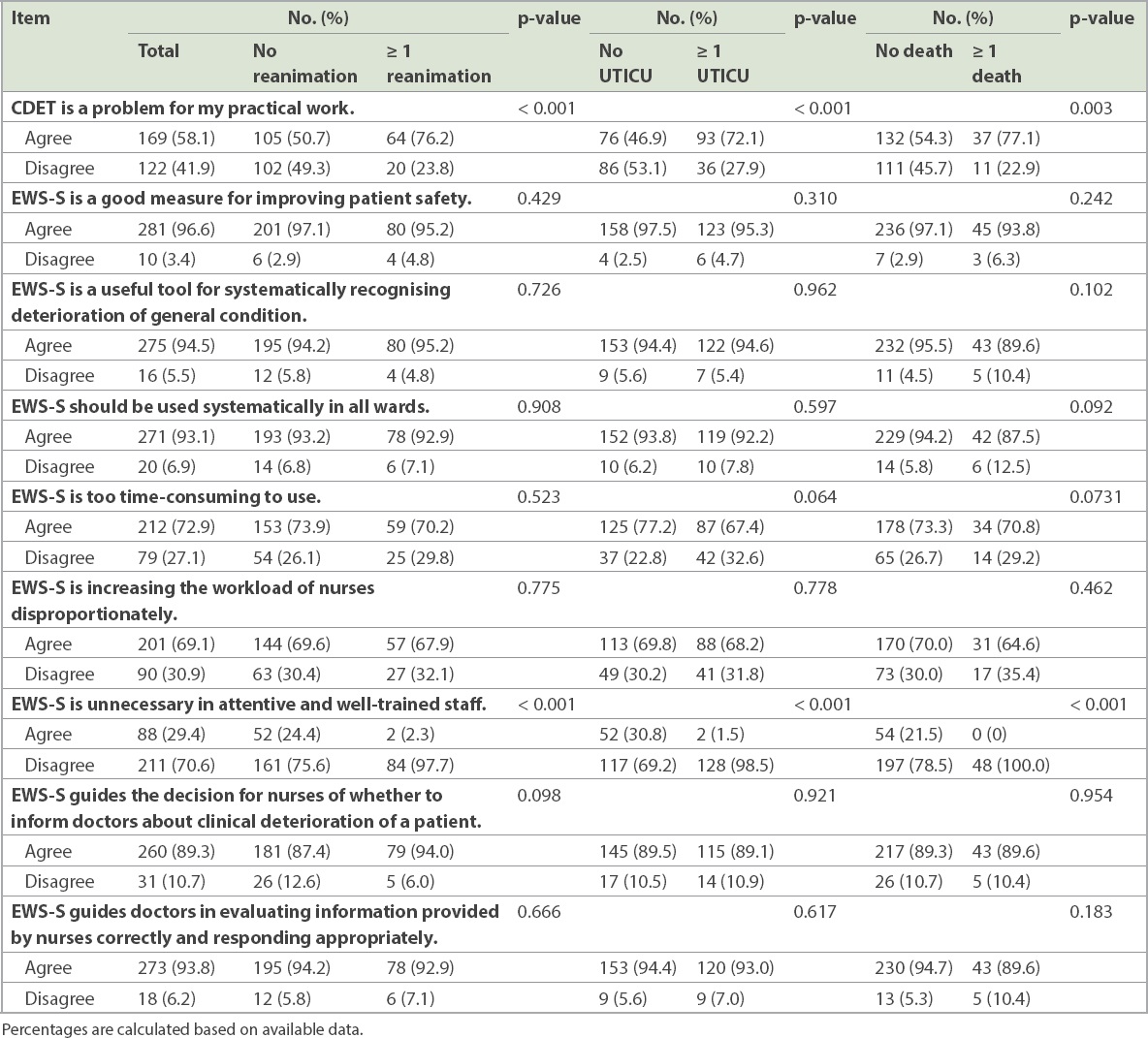
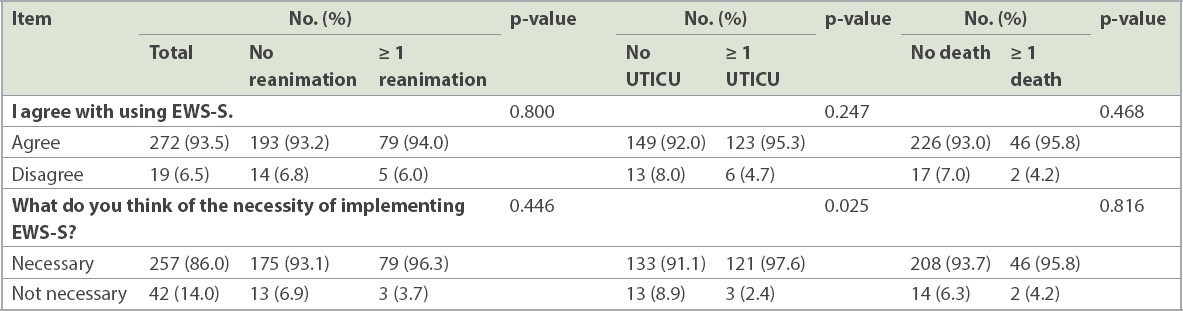
Physicians with previous UTICU experience were more likely to report the necessity of implementing EWS in their wards (p = 0.025) as compared with those without any relevant experience (
Table IV
Agreement towards and evaluation about the necessity of implementing EWS-S.
DISCUSSION
To the best of our knowledge, the current study represents the first attempt at exploring physician awareness of and attitudes towards EWS-S at a large Chinese general hospital. It also examines the associations between previously experienced CDET and UTICU, reanimation and/or death. Knowing the awareness and attitudes regarding EWS-S is an important prerequisite for the recommendation and implementation of EWS in Chinese hospitals. In our findings, most physicians considered unnoticed CDET to be problematic in their clinical practices. However, only 75.9% knew about a systematic assessment tool such as MEWS, and only 73.9% used it clinically. Only 61.9% physicians learnt about MEWS at research hospitals. Our results are similar to those of a comparable Swiss study.(1)
Since 2016, MEWS has been extensively applied in general wards of domestic research hospitals. However, there is an urgent need to enhance physician awareness of applying EWS-S, because physician awareness has been closely associated with task improvements. Hospitals in the UK have widely implemented EWS-S for many years. In 2012, the Royal College of Physicians started promulgating NEWS as a mandatory standard of early warning system in all UK hospitals.(19) However, the domestic application of EWS-S is still in its early infancy in mainland China. Actual project implementation will take a long time. The difference in implementation might be explained by the diverse national situations and compulsory policies in both hospitals and governments. Most physicians had positive attitudes towards EWS-S. As an excellent measure for improving patient safety, it was also considered a useful tool for systematically recognising deterioration of patients’ general conditions. The current study’s results are similar to those of the study by Richard et al,(1) in which 91.6% of all physicians considered EWS-S as a useful tool for recognising patients’ deterioration. A positive attitude is a strong impetus for recommending and implementing EWS-S at domestic hospitals. There is also mounting evidence that EWS-Ss are associated with lower mortality and fewer UTICUs.(1,20,21)
In the present study, the consensus among physicians was that EWS-S should be used systematically in all wards. However, over 50% of the physicians with and without previous CDET experience considered applying EWS-S to be too time-consuming and thought that it would generate a heavier nursing workload. This finding was consistent with the reports of Cherry et al(22) and Lydon et al.(23) Cherry et al explained that when staff members across the hospital work under time constraints, a miscalculation of MEWS scores could occur. Lydon et al also suggested that a large number of ‘false-positive’ patients may cause an increased workload for junior doctors responding to elevated NEWS scores because of score issues with low specificity.(6)
Furthermore, not establishing a MEWS electronic system has increased the nursing workload and caused calculation errors. In both the UK and US, there have been distinct advantages to using an electronic system, such as a personal digital assistant and VitalPAC, for collecting, calculating and storing the relevant data in a central database;(24-26) this enabled more complete, accurate and faster data processing than the traditional pen-and-paper method did. Thus, constructing an information system is vital for EWS if Chinese hospitals plan to implement the project.
Physicians who had previous experience with UTICU, reanimation and/or death were more likely to consider EWS-S as necessary in attentive and well-trained staff. This was possibly because their ability to see a cost-benefit relationship was affected by previous experiences, which is consistent with psychological theories of emotional, cognitive, and motivational processes and attitude changes. Physicians might also look for psychological consistency between their attitudes and behaviours.(27) Those with previous CDET experience might have a more positive attitude towards EWS-S.
Most physicians felt that it was necessary to implement an EWS, particularly those with previous UTICU experience. It is doubtless that EWS-S offers many advantages in terms of detecting patient deterioration.(28) Applying EWS-S to reduce the number of adverse events is gaining popularity at many domestic hospitals. However, owing to the large variety of EWS-Ss, selection of a suitable tool becomes a clinical challenge. Considering the need for sensitivity in certain subspecialties, practitioner engagement, reactions after escalations and clinical judgements, domestic hospitals should consider their current status, healthcare delivery system and specialties during the implementation of EWS-S. Establishing an electronic system capable of automatically alerting staff to CDET is vital for patient safety.
Three major limitations were inherent in the present study. First, we recruited physicians only from a single hospital. Hence, the small sample size and selection bias might affect the results. In future studies, the sample size should be expanded and multiple-centre surveys should be conducted. Second, the questionnaire was imported from Switzerland. Future studies should take cultural issues and national conditions into consideration. Third, only physician awareness and attitudes were addressed. Further studies focusing on a wider scope of behaviour, awareness and attitudes may yield more representative results.
In conclusion, most of the physicians we studied in a research hospital had a positive attitude towards applying EWS-S. However, their awareness remained low and further improvement is required. Generally, those with previous experience with UTICU, reanimation and/or death consider EWS-S to be essential in attentive and well-trained staff. Physicians who had previous experience with UTICU are more likely to support the implementation of EWS-S. Therefore, it is essential to educate physicians with evidence-based knowledge about EWS-S. This would enable them to improve their awareness and alter their behaviour towards using EWS-S more efficiently. To better facilitate the implementation of EWS-S in Chinese hospitals, existing facilities, policy supports, standardised management and the development of information systems should be strengthened. A survey with a large sample size should be conducted in future to obtain a better understanding of physicians’ awareness, attitudes and behaviours.
ACKNOWLEDGMENTS
The authors would like to acknowledge the financial support from the Regional Collaboration Innovation Project of Xin Jiang Municipality (2017E0278) and express their appreciation to all participating physicians from Xiangya Hospital, Hunan, China.


