Abstract
INTRODUCTION
Two strategies are available for prevention of early-onset group B streptococcal (GBS) sepsis – clinical risk factor-based screening and routine culture-based screening of pregnant women for GBS colonisation. In our hospital, we switched from the former to the latter approach in 2014.
METHODS
We compared the incidence of early-onset GBS sepsis during 2001–2015 between infants born to pregnant women who were screened for GBS colonisation and those born to women who were not screened.
RESULTS
Among 41,143 live births, there were nine cases of early-onset GBS sepsis. All infants with GBS sepsis were born to pregnant women who were not screened for GBS colonisation. The incidence of early-onset GBS sepsis among infants of women who were not screened was 0.41 per 1,000 live births (95% confidence interval [CI] 0.19–0.77) when compared to infants of women who were screened, for whom the sepsis incidence was zero per 1,000 live births (95% CI 0–0.19; p = 0.005).
CONCLUSION
Our data suggests that routine culture-based screening of pregnant women for GBS colonisation is a better preventive strategy for early-onset GBS sepsis in neonates when compared to clinical risk factor-based screening.
INTRODUCTION
Group B streptococcal (GBS) sepsis/infection has been recognised as a major cause of neonatal sepsis for over four decades.(1,2) Vertical transmission from mother to infant may result in early-onset GBS (EO-GBS) infection during the first week of life. EO-GBS infection carries significant fatality rates and many survivors have poor long-term neurological outcomes.(3,4) The infection risk can be reduced significantly by administering intrapartum antibiotic prophylaxis (IAP) to the pregnant woman before the infant’s birth, if certain risk factors are present (i.e. clinical risk factor-based strategy) or if an antenatal rectovaginal swab reveals GBS colonisation (i.e. routine screening strategy).(5) The incidence of EO-GBS sepsis has declined after IAP was used more frequently by obstetric units worldwide.(6) At our hospital, IAP is usually given based on maternal clinical risk factors, but obstetricians have lately been keener on the routine culture-based screening approach, as it is perceived to be a more targeted, logical and easier-to-implement strategy, especially when coupled with increased patient demand due to heightened societal awareness.(7)
This retrospective review aimed to delineate the trend in antenatal screening for GBS colonisation at our hospital and its impact on EO-GBS sepsis rates in infants over a 15-year period.
METHODS
The study period was from 1 January 2001 to 31 December 2015. Anonymised clinical details of EO-GBS sepsis (blood-culture positive) in infants were obtained from the neonatal intensive care unit patient database at the National University Health System, Singapore, with ethical approval from the hospital’s Domain Specific Review Board. The hospital laboratory provided data for antenatal screening rates for GBS colonisation of pregnant women. This data was available from 2006 to 2015. For the period 2001–2005, when laboratory GBS screening data was not available, a screening rate of 5.0% was assumed based on the 2006 screening rate of 5.5%, which was consistent with the approach adopted at that time, the clinical risk factor-based prevention approach without routine culture-based GBS screening.(8)
Rectovaginal swabs were taken between 35 and 37 weeks of gestation and sent to the hospital laboratory without unnecessary delay. Samples were submitted in Amies transport medium without charcoal (Copan, Brescia, Italy). Prior to January 2012, samples were plated directly onto trypticase soy agar with 5% sheep blood (bioMérieux, Marcy-l’Etoile, France). Inoculated agar plates were incubated in ambient air at 36°C for up to two days. Colonies suspicious for GBS were identified via MALDI Biotyper (Bruker Daltonics, Bremen, Germany). An enrichment step with Todd-Hewitt broth (bioMérieux, Marcy-l’Etoile, France) was introduced in January 2012, wherein samples were inoculated into the Todd-Hewitt broth and incubated in ambient conditions at 36°C for 6–8 hours before being plated, as above.
In 2014, routine GBS screening became unit policy and closely followed the United States (USA) Centers for Disease Control and Prevention (CDC) guidelines.(9) The antibiotic used was intravenous ampicillin, given as a 2-g loading dose followed by 1 g every four hours.(10) Prior to 2014, intrapartum ampicillin was generally given to women in labour in case of maternal fever, prolonged rupture of membranes more than 18 hours and preterm labour ≤ 34 weeks, according to the clinical risk factor-based protocol.(11) Since 2008, however, obstetricians at our hospital also began offering pregnant women routine culture-based GBS screening at 35–37 weeks gestation. This decision was taken after two infants with EO-GBS sepsis were born at the centre in 2008 after no such instances in the preceding four years.
If GBS screen-positive pregnant women had received adequate IAP, their infants would be observed for 24–48 hours after birth for signs of neonatal sepsis.(9) If, however, IAP was inadequate (ampicillin < 4 hours before delivery) or not administered, our policy for the asymptomatic well infant was to perform a full blood count, C-reactive protein test and blood culture, and commence the infant on intramuscular penicillin for 48 hours until a negative blood culture was obtained. This approach for cases of inadequate IAP was different from the American Academy of Pediatrics guideline, which recommends observation for signs of infection without the need to administer empirical antibiotics to an asymptomatic infant.(9) The Royal College of Obstetricians and Gynaecologists Green-Top Guideline does not have a clear recommendation in this regard.(12)
All statistical analyses were performed using IBM SPSS Statistics version 24.0 (IBM Corp, Armonk, NY, USA), with statistical significance set at p-value < 0.05. Fisher’s exact test was used to compare the incidence of EO-GBS sepsis between infants born to screened and unscreened pregnant women as well as the differences in GBS colonisation rates across the various ethnic groups. Linear regression analysis was performed to determine the rise in screening rate per year.
RESULTS
The GBS screening rate was 5.5% in 2006, and this increased significantly to 34.2% in 2007 and 60.6% in 2008 (
Table I
Overall GBS screening data at our centre during 2001–2015.
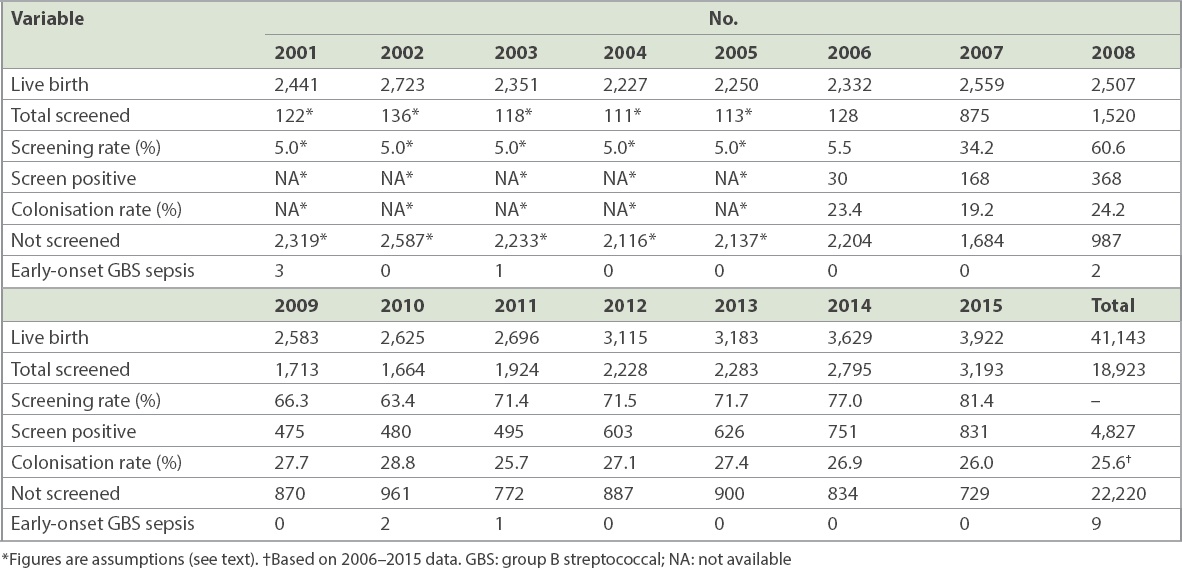
During the 15-year study period, there were 41,143 live births and nine infants with EO-GBS sepsis, giving an incidence of 0.22 per 1,000 live births (95% CI 0.12–0.42 per 1,000). The majority of affected infants were born term (66.7%) and presented with respiratory distress within the first eight hours of birth (
Table II
Clinical details of infants with GBS sepsis at our centre during 2001–2015.
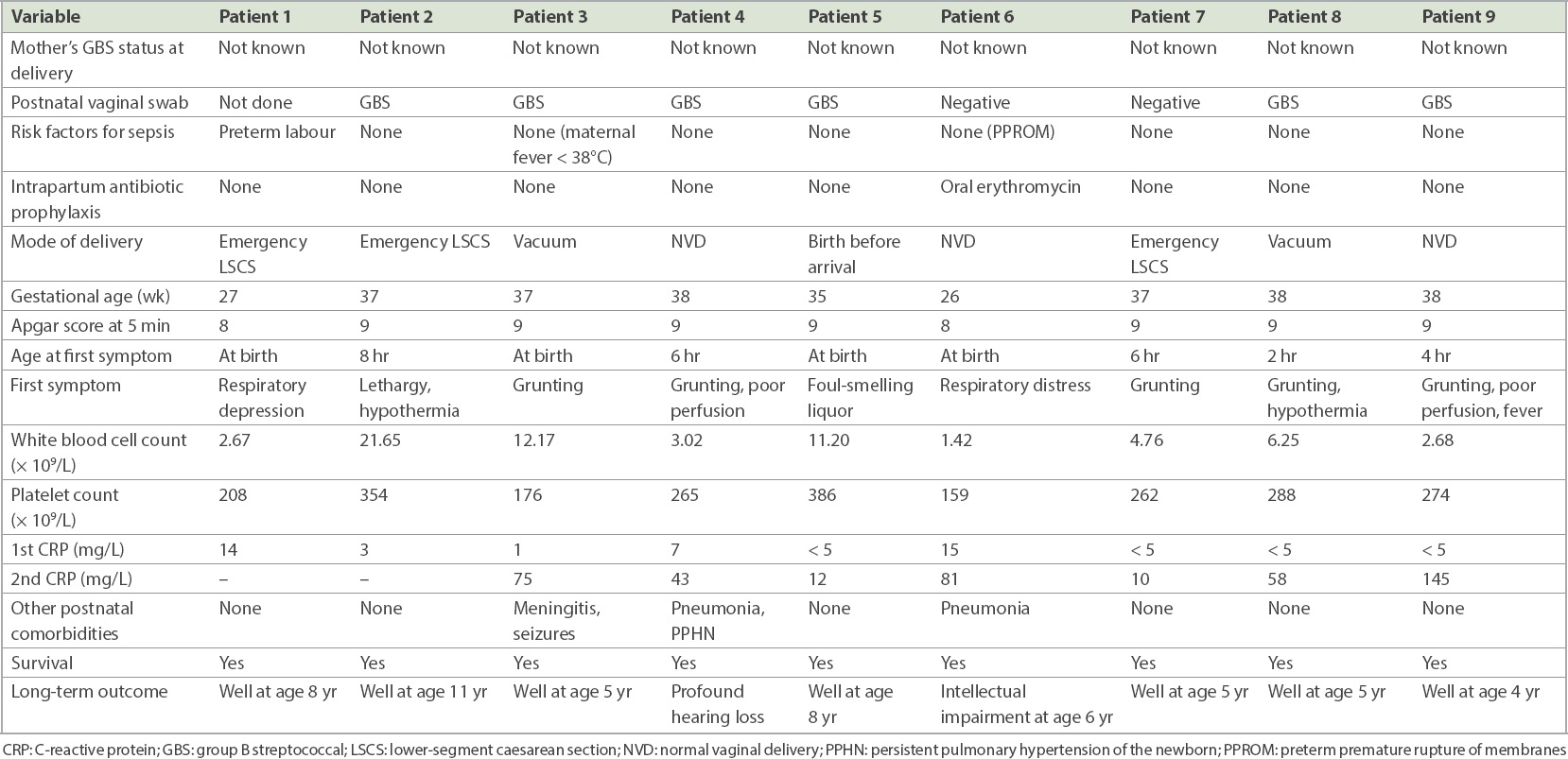
All nine infants with EO-GBS sepsis were born to women who were not screened for GBS colonisation. Thus, the incidence of EO-GBS sepsis among infants born to pregnant women who were not screened was 9/22,220 or 0.41 per 1,000 live births (95% CI 0.19–0.77) when compared to that of infants born to women who were screened, which was 0/18,923 or zero per 1,000 live births (95% CI 0–0.19) (p = 0.005). Since three infants with GBS sepsis were born preterm and it was not preventable by antenatal screening, and the population of preterm infants in the whole cohort was 3,415/41,143 (8.3%) live births, the EO-GBS sepsis incidence among infants born to women not screened for GBS colonisation after excluding preterm deliveries was 6/18,805 or 0.32 per 1,000 live births (95% CI 0.11–0.69). Hence, to prevent one case of EO-GBS sepsis, 3,125 (95% CI 1,449–9,091) pregnant women needed to be screened and 822 (95% CI 381–2,391) treated, based on the GBS colonisation rate of 26.3% in our study.
DISCUSSION
Our EO-GBS prevention policy prior to 2014 was, in general, clinical risk factor-based. However, the criteria used under this strategy were variable depending on the individual obstetrician’s preference. GBS screening increased significantly in 2008 following the finding of two infants with EO-GBS sepsis at our centre after a four-year hiatus. The EO-GBS sepsis rate for the entire 15-year study period in 2001–2015 was 0.22 per 1,000 live births (95% CI 0.12–0.42 per 1,000 live births). During 2009–2015, when GBS screening was offered to more patients, the EO-GBS sepsis rate was lower at 0.14 per 1,000 live births (95% CI 0.03–0.40). During the earlier period (2001–2008), when the clinical risk factor-based strategy was prevalent, the EO-GBS sepsis rate was higher at 0.31 per 1,000 live births (95% CI 0.11–0.67).
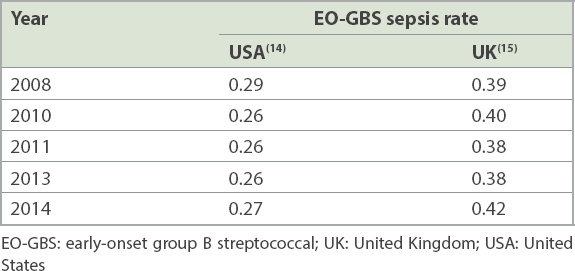
Our results offer a better perspective when compared with data from two other countries that have differing GBS prevention protocols. In the USA, universal culture-based screening for GBS has become the norm since the CDC issued its guidelines in 2002.(13) Meanwhile, the United Kingdom (UK) follows the clinical risk factor-based prevention protocol. A comparison of population-based EO-GBS sepsis rates between the two countries is shown in
Among the nine infants with EO-GBS sepsis in our cohort, none of the mothers were given IAP. Only one infant (Patient 1) had a risk factor (i.e. preterm labour) that called for the administration of IAP. However, for this infant, the delivery was too precipitous and there was insufficient time for IAP administration. This illustrates one drawback of the clinical risk factor-based prevention protocol, in that many of our pregnant women whose infants later developed EO-GBS sepsis did not have clinical risk factors for GBS sepsis during labour.(16) Three instances of EO-GBS sepsis in our cohort were among infants born preterm; in all likelihood, their mothers would not have been screened even if routine culture-based screening protocol had been practised. However, some guidelines do recommend IAP for all preterm labours due to the higher risk of EO-GBS sepsis in preterm deliveries. This observation was borne out by the data in our cohort, where the risk of EO-GBS sepsis was one in 1,371 live births in preterm deliveries when compared to one in 6,172 live births in term deliveries – a 4.5-fold higher risk.
The maternal GBS colonisation rate at our centre, which is a multidisciplinary tertiary general hospital with an obstetric unit, was 26.3%. This was consistent with recent reports.(17,18) We also noticed significantly different GBS carriage rates among local ethnic groups, with significantly higher rates among Malay and Indian patients when compared to those of Chinese and other ethnicities. Differences in GBS carriage rates among various ethnic groups have previously been noted in other countries as well.(19,20)
There are concerns that significantly more women would receive antibiotics if a routine screening strategy is employed, compared to a clinical risk-based strategy. Two studies, however, have suggested that this may not necessarily be the case. A 1996 Morbidity and Mortality Weekly Report found that the proportion of screened pregnant women who received IAP during a screening approach was 26.7% when compared with 24.7% of pregnant women who had clinical risk factors during the intrapartum period that warranted administration of IAP.(21) Hiller at al determined that in their cohort, 20% of women were GBS colonised compared to 18% of women who were identified as being eligible for IAP based on the clinical risk factor algorithm.(22) These studies suggest that the risks from antibiotic overuse (e.g. antibiotic-induced anaphylaxis, antimicrobial resistance, antibiotic-associated asthma and other allergies) should not be amplified if a routine culture-based screening strategy is used for pregnant women.(23,24)
Implementation of routine GBS screening at our hospital was quite straightforward, with very few pregnant women declining it when it was offered at the 35–37 weeks’ gestation visit. Deciding on the need for IAP was also simple, as doctors who were busy in the labour wards would only need to consider the test results of a single GBS screening, which was positive, negative or not available. In contrast, decision-making regarding IAP, when using the clinical risk factor-based approach, is much more challenging because there are many more variables to consider and is thus more complex to comply with in real-world clinical practice.
However, studies on EO-GBS sepsis from the USA have surprisingly found that 70%–82% of infants with EO-GBS sepsis were born to women who were screened negative for GBS colonisation despite the use of rectovaginal swabs and employing appropriate laboratory methods, as recommended by the CDC.(16,25) Such apparently false-negative screening results precluded the use of IAP in these pregnant women. Hence, it would be very important for any screening programme to look into the possible reasons for false-negative maternal GBS screening results when using the culture-based approach. These may include the time interval between swab collection and delivery; using vaginal rather than rectovaginal swabs, swab storage and transfer practices; and inappropriate culture methods.(9) In our study, there were no cases of EO-GBS sepsis among infants born to women who screened negative for GBS colonisation. This was reassuring in terms of quality control for a screening programme.
There were some limitations to our study due to its retrospective nature. Data for GBS screening rates for 2001–2005 was not available, and while our assumption of a 5.0% screening rate (based on actual 2006 data) should not be far off the mark, it could nevertheless have affected statistical calculations. There was no information on the proportion of GBS-colonised women who were given IAP, even though none of the infants born to such women had EO-GBS sepsis in our study. Also, our analysis included only blood culture-positive infants. There might have been infants who had GBS infection but were blood-culture negative, and were symptomatic and treated as clinical infection. Such cases might conceivably occur more commonly in infants born to screen-positive mothers who were given IAP, an effect analogous to partial treatment. Lastly, although EO-GBS sepsis usually presents during the first 48 hours of life, in rare cases, infants can become symptomatic later at up to six days of life, requiring re-admission for treatment. Such cases would not have been captured in this retrospective review.
In summary, our findings of a lack of EO-GBS sepsis in infants born to GBS-screened pregnant women seem to support the effectiveness of a routine culture-based GBS screening approach for pregnant women. Our experience was that it was not difficult to implement such a strategy, as screening rates rose rapidly soon after process change at our centre. What remains unknown is the true cost effectiveness of either a clinical risk factor-based or a routine culture-based screening strategy, which could probably be ascertained only by large randomised controlled trials. Such trials may, however, be difficult to justify in view of the already very low incidence of EO-GBS sepsis in infants regardless of the GBS screening approach adopted for pregnant women.(26,27)
About the First Author
A/Prof Lee Jiun is Senior Consultant and Research Director at the Department of Neonatology, National University Hospital. He was Head of Department from 2005 to 2016. He specialises in neonatal ventilation. His research interests include prevention of bronchopulmonary dysplasia, non-invasive detection of hyperbilirubinemia, and improving outcomes for very-low-birth-weight infants.