Roy, an 18-year-old polytechnic student, presented to your clinic with an uncomplicated upper respiratory tract infection and requested for a medical certificate to rest at home. His medical records showed that he had visited the clinic several times for minor ailments over the past few months. You also noticed that he had multiple pimples over his face. When prompted, he shared that he has an upcoming graduation ball in a few months’ time and was worried about his appearance, particularly the pimples on his face.
WHAT ARE PIMPLES?
Pimples are inflamed comedones. They are red papules, pustules or nodules found most frequently on the face, neck and upper torso of adolescents and young adults.(1) Pimples are part of acne vulgaris, which is a chronic inflammation of the pilosebaceous unit of our skin. Vulgaris is the Latin adjective for ‘common’, while acne vulgaris is likely the most common variant of acne.
Comedones arise from proliferation of cells lining the sebaceous duct (cornification) and an increase in sebum production (seborrhoea), primarily owing to the hypersensitivity of pilosebaceous units to circulating androgens (e.g. testosterone). Increased inflammation in comedones is a consequence of rise in sebum production, increase in colonisation with Cutibacterium acnes (previously called Propionibacterium acnes), and release of bacterial enzymes and sebaceous proinflammatory cytokines.(2)
HOW RELEVANT IS THIS TO MY PRACTICE?
Pimples, often accepted as part of puberty, can have profound social and psychological effects on adolescents or young adults when these affect their self-esteem, how they fit in with their peers or as they cope with new colleagues in their first workplaces.
In a local study conducted in Singapore, 88% of adolescents aged between 13 and 19 years reported that they had acne.(3) Another study from National Skin Centre Singapore reported that 41% of adults seeking treatment had experienced acne since adolescence. Comedonal acne is more prevalent in adolescents, while cystic acne occurs more frequently in adults.(4)
WHAT CAN I DO IN MY PRACTICE?
Primary care doctors are well placed at the front line of healthcare to identify patients with moderate to severe acne, those at risk of scarring or those who are adversely affected socially and psychologically, when they present for any preventive or acute medical conditions. Informing patients of the availability of treatment modalities and stopping any preventable precipitating or perpetuating factors can be helpful even if the patients are not yet ready to start any clinical treatment.
Important aspects in history taking
History of aggravating and causative factors
A detailed history can help to exclude systemic disorders (e.g. Cushing syndrome, androgen-secreting tumours) or medications (e.g. corticosteroids, anti-epileptics, isoniazide, rifampicin, lithium) as a cause of acne. Women should be asked regarding symptoms of hyperandrogenism (i.e. are menstrual periods regular? Is there hirsutism?). Variations in acne severity should be assessed, as they may be associated with hormonal swings in pregnancy and menopause. Occupational history may suggest exposure to oils and greases (chloracne); prolonged use of safety apparatus, such as well-fitting N95 masks, or motorcycle or industrial helmets, may result in friction or pressure on the skin (acne mechanica). The patient should be evaluated for use of occlusive cosmetics and skin products that are acnegenic (acne cosmetica),(5) and their stress levels during an acne flare-up should be assessed.(5,6)
History of previous treatment
Patients often self-treat with over-the-counter medications and may have experienced treatment failure or relapse. It is important to explore the reasons for previous treatment failure or relapse. Patients should be asked what medications were taken, how they were taken (topical vs. systematic, dose, frequency, duration including maintenance and compliance), what adverse effects they experienced and what measures were taken to reduce the adverse effects.
Psychosocial assessment
Patients affected by acne might manifest a range of psychological abnormalities and social dysfunction. This information may not be volunteered and will require prompting by the physician. Clues to identifying patients at high risk of psychological issues include poor eye contact, limited speech, angry or belligerent remarks, poor personal hygiene, and verbal self-depreciation.(6,7) The physician should explicitly ask about low mood and/or anhedonia which, if positive, warrant further questioning on depression and suicidal ideation. The Cardiff Acne Disability Index is a patient-administered, easy five-question scale to use in routine clinical practice to assess a patient’s psychosocial function. Its first two questions address the psychological and social consequences of acne in general; the third question seeks to assess the patient’s self-image owing to acne over the back or chest; the fourth question enquires into his/her psychological state; and the last question asks for the patient’s (subjective) assessment of his/her current acne severity.(8)
Clinical features of acne vulgaris
Acne vulgaris is a polymorphic disease often characterised by simultaneous occurrence of comedones, papules, pustules, nodules and pseudocysts. Lesions develop from the sebaceous glands associated with hair follicles on the face, chest and upper back. Seborrhoea is frequently present.
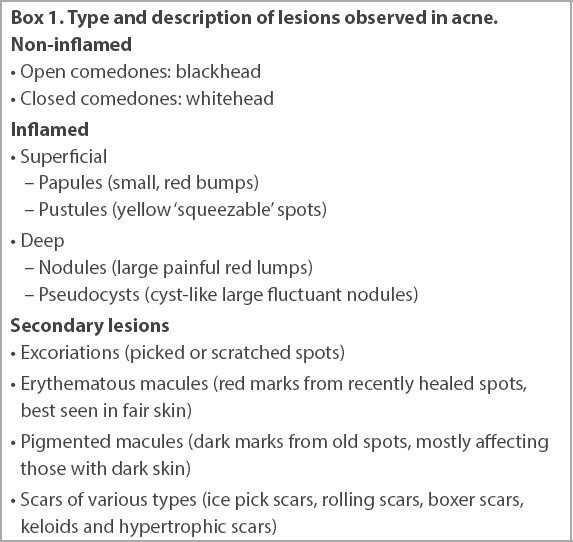
Box 1
Type and description of lesions observed in acne.
Severity of acne
The severity of the acne can be classified based on physical findings or the social and psychological impact on the individual. Based on the type of lesions and area affected, acne severity can be graded using the Comprehensive Acne Severity Scale (
Table I
Comprehensive Acne Severity Scale.
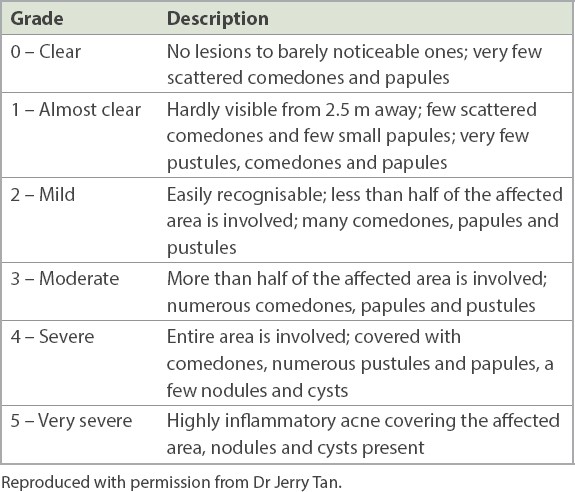
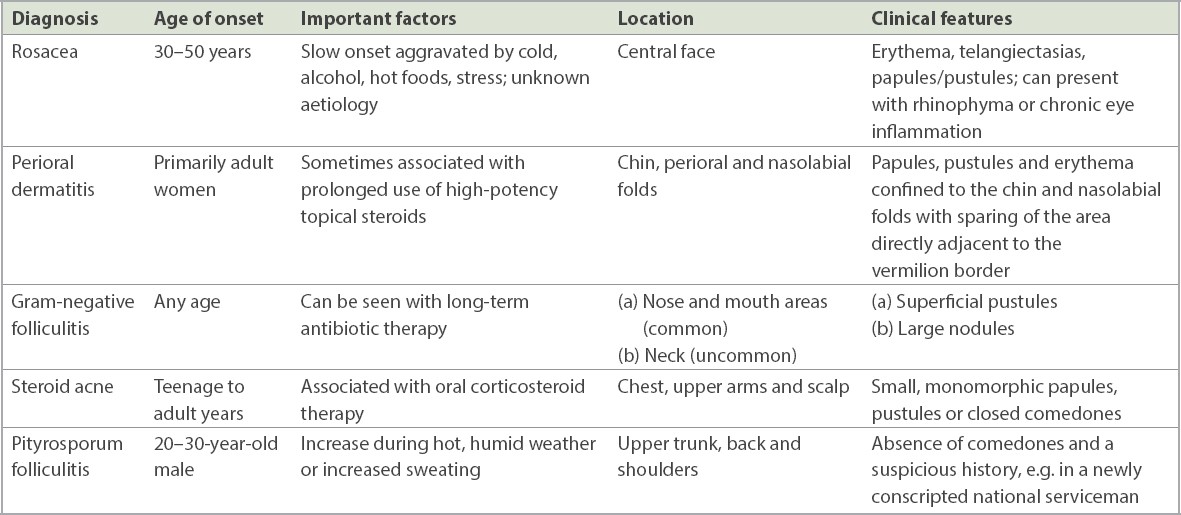
Table II
Differential diagnosis of acne vulgaris.
Treatment goals for acne vulgaris
Acne should be actively managed, with goals to reduce comedonal and inflammatory lesions, improve psychosocial symptoms and prevent permanent scarring. Multiple treatment agents and formulations are available, and the treatment of acne depends on the patient’s age and gender, disease severity, duration of the acne and tolerability.
Table III
Management of acne vulgaris.
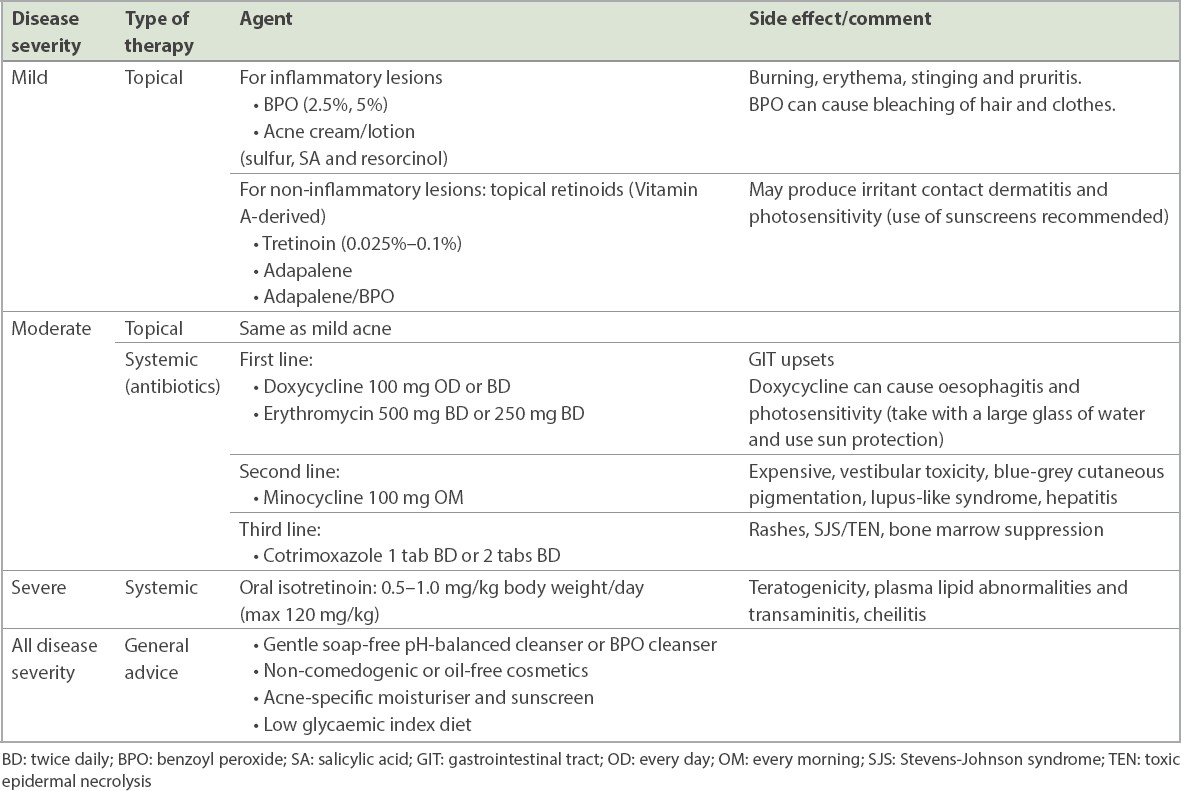
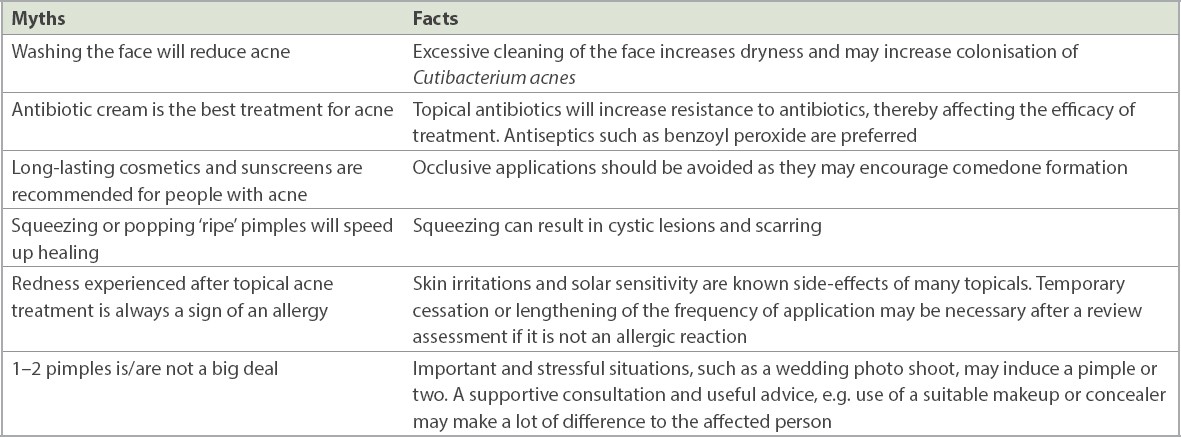
Table IV
Myths and facts regarding treatment of acne.
Topical therapy
Topical agents used for treatment of acne include creams, lotions and gels. The choice of preparation depends on the extent of area affected: creams and gels are preferred for small areas, and lotions are reserved for larger surfaces such as the upper torso. They should be applied to the entire site that is prone to acne rather than to the acne lesions alone. Most topical preparations can cause skin irritation, resulting in erythema, desquamation, dryness, stinging and pruritus, especially if applied excessively. Skin irritation can be improved by initiating the treatment at a low dose on alternate days, slowly titrating upward as required. A simple topical regime is recommended to improve compliance.
Benzoyl peroxide (BPO; 2.5% or 5%) has comedolytic, anti-inflammatory and bactericidal actions against Cutibacterium acnes (C. acnes). It can be used alone or in combination with topical antibiotics or retinoids. The use of BPO in itself does not induce bacterial resistance, and it can be used in pregnancy. In addition to skin irritation, BPO can cause bleaching of hair or clothing.
Topical retinoids (tretinoin, adapalene) are Vitamin A derivatives that reduce microcomedones and mature comedones, promote desquamation of follicular epithelium and have an anti-inflammatory effect. Tretinoin may cause photosensitivity, and the use of sunscreens is advised. Clinical evidence does not support the belief that topical retinoids cause a flare-up in acne in the initial few weeks.(12) Adapalene is better tolerated than tretinoin, as it causes less skin irritation.(13) Topical retinoids are recommended for maintenance after successful treatment of acne.
Acne creams and lotions are available over the counter and contain active ingredients such as sulfur, salicylic acid and resorcinol. These topicals induce a comedolytic effect by causing inter-corneocyte cell detachment; they improve skin texture and are recommended for inflamed comedones.
Systemic therapy
C. acnes has shown growing antibiotic resistance in Singapore.(3) To reduce antibiotic resistance and increase efficacy, oral antibiotics should be used in combination with non-antibiotic topical agents. Oral antibiotics are indicated in the management of moderate to severe inflammatory acne owing to their anti-inflammatory effect as well as their action against C. acnes. Treatment for a minimum duration of 4–6 weeks is generally required to see a clinical improvement. The dosage is maintained until clearance, after which it is gradually decreased. Some patients require a low dose maintenance treatment for 1–2 months to prevent relapse. Oral antibiotic treatment should not exceed 3–4 months.
Doxycycline and erythromycin are recommended as first-line oral antibiotics. Erythromycin can be used to treat severe acne in pregnancy. Doxycycline is contraindicated in pregnancy and in children younger than eight years of age. Doxycycline should be taken with a large glass of water (to reduce oesophagitis and dyspepsia) and sun protection should be used (to alleviate photosensitivity).
Minocycline, advocated as the second-line oral antibiotic treatment for acne, is expensive, is associated with more central nervous system side effects, and has been linked to lupus and autoimmune hepatitis. Cotrimoxazole is recommended as the third-line treatment only when the patient is intolerant or unresponsive to other treatments. It is effective but carries a risk of serious adverse events (e.g. Stevens-Johnson syndrome/toxic epidermal necrolysis, bone marrow suppression). It is also contraindicated in glucose-6-phosphate dehydrogenase deficiency.
Topical antibiotics may be considered only if the patient is unable to tolerate oral antibiotics and should be used in combination with other topical agents to avoid bacterial resistance.(14,15)
Further clinical options such as systemic isotretinoin or oral hormones may also be considered after further assessment if the initial therapies are ineffective or if the acne recurs after the treatment course has ended. Common dose-dependent adverse effects of isotretinoin include xerosis, cheilitis, acne flare-up, dry eyes, headache, and elevated lipid and hepatic enzyme levels. Pregnancy must be ruled out prior to starting therapy with oral isotretinoin, and female patients should be counselled regarding the risk of teratogenicity and appropriate contraceptive methods.
Combined oral contraceptives may be considered in female patients with moderate-to-severe papulopustular acne, signs of hyperandrogenism, need for effective contraception (e.g. during oral isotretinoin use), and as an adjuvant therapy to topical and systemic therapies.
WHEN SHOULD I REFER TO A SPECIALIST?
Referral depends on treatment goals, severity of acne, and availability of formulary and equipment. Dermatologist referral is recommended in cases of severe, recalcitrant acne that fails to respond to first-line treatments. Severe scarring, psychological and/or physical distress or contraindications (e.g. allergies or intolerance) to the first lines of topicals and systemic therapy are also indications to refer for further assessments and early treatment. If clinical findings suggest underlying systemic disease, appropriate referrals to other specialty should be considered. The presence of a significant psychiatric comorbidity (depression, suicidal ideation) warrants prompt referral for counselling and, if required, psychiatric assessment.
TAKE HOME MESSAGES
-
Acne vulgaris is a common variant of acne that is commonly encountered by adolescents and young adults.
-
Although affected individuals may not visit a doctor for acne vulgaris, some may suffer from profound social and psychological effects and may be unaware that skin complications such as scars and keloids can be prevented or made less noticeable.
-
Acne vulgaris should be actively managed to prevent potential sequelae of acne, such as scarring, dyspigmentation and low self-esteem.
-
In addition to clinical findings, patients’ perception of the severity of their acne should direct acne management.
-
Effective topical and systemic therapeutics for comedones and inflamed papulopustular acne can be offered by primary care physicians.
-
Antibiotics should be used only in combination with BPO and retinoids and for a maximum duration of four months to reduce the development of antibiotic resistance.
-
Referral to a dermatologist should be considered in severe, recalcitrant acne and in case of severe scarring, psychological distress or contraindications to conventional therapy.
On examination, Roy was found to have moderate acne with numerous comedones, papules and pustules involving more than half of his face. He said that he had used acne creams (sulfur resorcinol cream) with slight improvement. He had decided to stop taking oral doxycycline owing to mild dyspepsia. He was not aware that he needed to take this oral medication after food. On further probing, you realised that Roy felt judged at polytechnic when he had bad acne flare-ups. His topical medication was changed to adapalene 0.1% cream every alternate night, to be applied for one week and then gradually increased to nightly use. Adequate use of sunscreen was emphasised. He was able to tolerate oral doxycycline 100 mg twice daily for six weeks, when taken after food and with a full glass of water. On follow-up six weeks later, his acne had improved, with a definite reduction in the number of acne lesions. You reduced his oral doxycycline to 100 mg every day for another 4–8 weeks, and advised him to continue the adapalene cream for 3–6 months to prevent a relapse. Roy was looking forward to his graduation ball and was advised to use concealer to cover the remaining pimples for the event.
Supplementary Material
SMJ-62-573.pdf


