Abstract
INTRODUCTION
Ingestion of fish bones is a common clinical complaint among adult patients. The aim of this study was to evaluate the epidemiological and behavioural risk factors for fish bone ingestion.
METHODS
Between 2009 and 2010, a physician-administered questionnaire was administered to 112 consecutive patients who presented to the emergency department of an adult tertiary hospital with the complaint of fish bone ingestion.
RESULTS
The wearing of dentures, the use of utensils to eat fish and the practice of deboning fish in one’s mouth were found to be associated with an increased risk of fish bone ingestion.
CONCLUSION
To prevent the occurrence of fish bone ingestion and its possible complications, at-risk populations should be advised on the precautions to take when eating boned fish.
INTRODUCTION
In Singapore, ingestion of fish bones is one of the most common reasons for emergency referrals to an otolaryngologist. In the majority of these cases, the fish bones are readily removed in the emergency department (ED) using a flexible therapeutic nasoendoscope, through which a grasping forceps is passed to retrieve the bone. However, in a small proportion of cases, the fish bones become impacted distal to the cricopharynx and require removal with rigid endoscopy under general anaesthesia. A small minority of cases may present with complications such as extraluminal migration of the fish bones into the neck or thorax and abscesses in the neck or mediastinum, as well as complications from the bones passing further down the gastrointestinal tract, such as bowel perforation and liver abscesses.(1-4) Rare but disastrous sequelae such as aorticoesophageal fistulae have also been reported.(5)
In Lim et al’s 1994 study conducted on 397 patients in the same ED as the present study, fish bones were found to account for the majority (83.9%) of ingested foreign bodies. The incidence of fish bone ingestion was significantly higher among Chinese patients as compared with Malay or Indian patients, which led to the postulation that the use of chopsticks and the traditional Chinese practice of deboning fish in one’s mouth (using the teeth, lips and tongue) may be associated with a higher risk of fish bone ingestion. The authors also found that people who wore dentures were at a higher risk of swallowing foreign bodies, possibly because the use of dentures impairs the wearer’s ability to detect foreign bodies in the food bolus during mastication.(6) Similarly, studies conducted in Singapore(7) and Hong Kong(8) (which has a similarly high proportion of Southern Chinese) have reported a disproportionately higher prevalence of fish bone ingestion among the Chinese. This has led to the postulation that the Chinese habit of eating unfilleted fish with chopsticks may account for the higher prevalence of ingested fish bones in this population.
Thus, the aim of this prospective survey was to elucidate the epidemiological and behavioural risk factors (namely age, race, choice of utensils, method of deboning fish, use of dentures and vision problems) for fish bone ingestion and to account for its high prevalence in Singapore.
METHODS
Between 2009 and 2010, consecutive patients who presented to the ED with the complaint of fish bone ingestion were invited to participate in the survey. The patients answered a physician-administered questionnaire (
The patients then underwent routine management with direct examination of the oral cavity and oropharynx, flexible nasoendoscopic examination of the upper aerodigestive tract, and imaging (e.g. lateral neck radiography and plain computed tomography), if clinically indicated. The patients were categorised into two groups – those with fish bone lodged in the upper aerodigestive tract or oesophagus (fish bone positive group) and those without any fish bone (fish bone negative group) found on physical or radiological examination – and a comparison was made between the groups. A subgroup analysis was conducted to determine whether there were any differences in the risk factors between patients with impacted bones (assumed to be larger) and those with negative findings (presumably because the ingested bones were smaller and able to pass distally).
RESULTS
A total of 112 patients (51 male, 61 female) were surveyed. Most of the presenting patients surveyed were Chinese (79.5%), 7.1% were Malay, 3.6% were Indian and 9.8% were of other ethnicities (
Table I
Patient characteristics (n = 112).
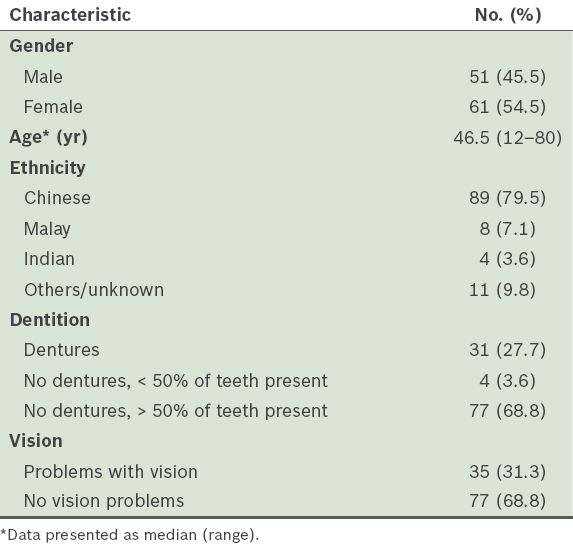
Among the 112 patients, 31 (27.7%) were wearing dentures at the time when the fish bone was ingested, while 77 (68.8%) had grossly intact dentition. Based on the patient report and oral examination performed by the physician administering the questionnaire, the remaining 4 (3.6%) patients had fewer than half their teeth intact but were not wearing dentures at the time of fish bone ingestion. 35 (31.3%) of the patients reported problems with their vision (i.e. short- or long-sightedness), while the remaining 77 (68.8%) patients had normal or good corrected vision.
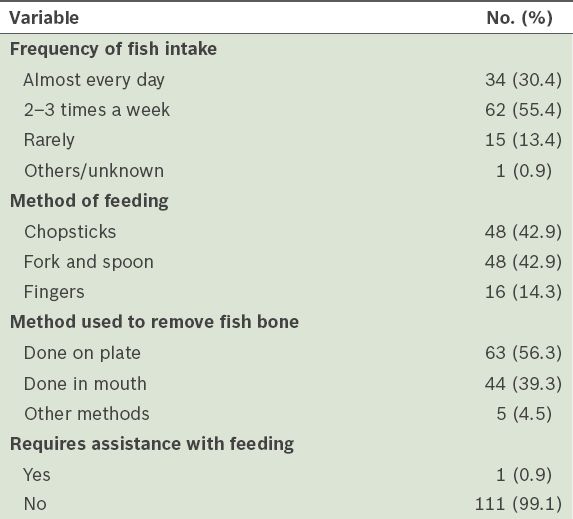
Among the 112 patients, 34 (30.4%) reported eating fish almost every day, while 62 (55.4%) patients ate fish 2–3 times per week (
Table II
Methods used by the patients (n = 112) to eat fish.
On clinical and radiological examinations, 87 (77.7%) patients had fish bones lodged in their upper aerodigestive tract or oesophagus and 25 (22.3%) patients did not (
Table III
Comparison of risk factors for fish bone ingestion between the two groups.
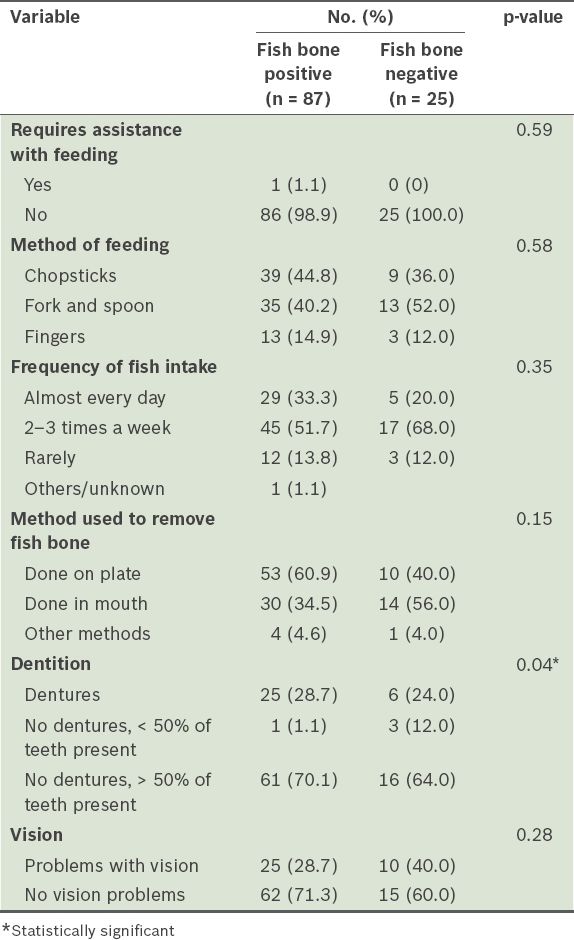
When the risk factors between the ‘fish bone positive’ and ‘fish bone negative’ groups were compared using Fisher’s exact test or chi-square test, the only risk factor that showed a statistically significant difference was the use of dentures. The ‘fish bone positive’ group had a higher proportion of patients using dentures (25/87 vs. 4/25, p = 0.04). There was no significant difference between the two groups in terms of age, gender, ethnicity, method of eating fish or presence of vision problems.
DISCUSSION
In Western populations, meat boluses are the most commonly encountered foreign bodies in the gastrointestinal tract.(9) Western studies have shown that patients who are at risk of foreign body ingestion include denture wearers, alcoholics, prisoners, patients with psychiatric disorders and individuals with intellectual impairment.(10) In Asian studies, fish bones are the most commonly ingested foreign body reported, and the aforementioned at-risk patient groups are not commonly encountered in Asian populations.(11)
The patients in the present study were relatively young, with a median age of 46.5 years. Most of the patients (n = 96, 85.7%) surveyed reported eating fish at least 2–3 times a week, which accurately reflects the dietary habits of our local population. Also, Chinese patients (79.5%) were most likely to present with complaints of fish bone ingestion; this percentage is only slightly higher than the Singapore population demographic of 74.1% Chinese.(12) All the patients in the present study who reported having eaten fish using chopsticks were Chinese. Among the Chinese patients surveyed, the majority (53.9%) used chopsticks, while 41.6% used fork and spoon and 4.5% used their fingers. Among the 23 non-Chinese patients, about half of them used fork and spoon, while the rest used their fingers.
When analysed collectively, we did not find any evidence that eating fish using chopsticks was more of a risk factor for fish bone ingestion than using fork and spoon. The proportion of patients using these two methods was found to be equal (42.9%). Only 14.3% of the 112 patients had used their fingers to eat fish. Thus, the use of utensils (whether chopsticks or cutlery) to eat boned fish may be a risk factor for fish bone ingestion. The tactile advantage gained when one eats using the fingers may explain the lower observed incidence of ingested foreign bodies among the Malays and Indians, who traditionally eat using their fingers.
Although the majority of patients in the present study reported that they had deboned the fish on the plate, a significant proportion (39.3%) had the practice of deboning fish in their mouths using their teeth, lips and tongue. Although this practice was previously thought to be unique to the Chinese,(6) it was reported in only a third of the Chinese in the present study; interestingly, it was reported in half of the Malay and Indian patients and about 80% of patients of other ethnicities. Thus, the practice of deboning fish in one’s mouth is possibly a strong independent risk factor for fish bone ingestion. It would be interesting to determine the prevalence of this practice in a control group who has not had an episode of fish bone ingestion, to determine if this is indeed a preventable risk factor.
In the present study, poor corrected vision was not easily quantifiable as a risk factor for the ingestion of fish bones. A minority (31.3%) of the participants reported problems with their vision. The mean age of those who reported vision problems (52.3 years) was slightly higher than that of the overall study population (46.5 years). The types of vision problems reported included presbyopia, presbyopia with myopia, cataract, recent eye surgery, uncorrected or insufficiently-corrected myopia, as well as not wearing spectacles at the time of fish bone ingestion. Given the high local incidence of myopia (40%) in adults aged over 40 years,(13) it is difficult to postulate whether the incidence of vision problems in our study cohort is significantly different from that of the general population.
Although most of the patients in the present study did not wear dentures (72.3%), it is possible that denture wearers made up a higher percentage (27.7%) of our study cohort than of the general population. All but four of the denture wearers were aged over 50 years, and there was no gender or racial predilection. It is reasonable to assume that the use of dentures impairs the wearer’s ability to sense sharp objects in a food bolus using the palate and gums, hence increasing the risk of fish bone ingestion. Interestingly, nine of the 31 patients who wore dentures still practiced the deboning of fish in their mouths despite the reduced sensation afforded by dentures. On further analysis, we found that there were significantly more denture wearers in the ‘fish bone positive’ group. These findings are similar to that of a previous local study, in which the prevalence of denture wearers in a subgroup who had impacted fish bones was found to be 1.8 times higher than that of another subgroup who did not have impacted fish bones.(6) The aforementioned findings add weight to the proposition that the use of dentures is a significant risk factor for fish bone ingestion.
As fish bones were not found in only a quarter of our participants during examination, the imbalance in the sample size of the two subgroups (i.e. the ‘fish bone positive’ group was much larger than the ‘fish bone negative’ group) may have led to the inability to detect other statistically significant epidemiological risk factors (type II error) other than the use of dentures. This error could have been reduced if the overall number of patients surveyed was increased, or if both the ‘fish bone positive’ and ‘fish bone negative’ groups were combined and then compared with a separate control group (e.g. patients who present to the ED for other ear, nose and throat complaints but without previous episodes of ingested fish bones). Thus, the absence of a true control group is a limitation of the present study, as its inclusion could have helped to determine the prevalence of identified epidemiological and behavioural risk factors in the unaffected general population.
To conclude, ingestion of fish bones is a very common otolaryngological emergency in Singapore, as fish is a staple food in the local diet. The present study identified behavioural factors, such as the use of chopsticks or cutlery to eat boned fish, the practice of deboning fish in the mouth and the wearing of dentures while eating fish, as likely risk factors for fish bone ingestion. A large majority of the participants who presented with ingested fish bones were of Chinese ethnicity, possibly because of the aforementioned behavioural factors and the population demographics of Singapore. It may be worthwhile to address some of the modifiable risk factors through patient education so as to prevent rare but potentially serious complications that may arise from ingesting fish bones.
Supplementary Material
SMJ-56-333-appendix.pdf


