Dear Sir,
Systemic sclerosis (SSc) is an immune-mediated disease characterised by endothelial vasculopathy and diffuse fibrosis of internal organs. The extent of skin sclerosis and the accompanying pattern of internal organ involvement are closely related to disease activity. Various nationwide cohort studies have shown that SSc is associated with an elevated incidence of malignancy.(1) Although the role of immunosuppressive therapies and the effects of autoantibodies associated with malignancies are not clearly defined, patients with a later onset of SSc and diffuse cutaneous subtype are at higher risk for malignancy.(2)
Pheochromocytoma is a rare tumour associated with high mortality if not diagnosed early. As adrenergic symptoms such as hypertension, headache, palpitations and diaphoresis may be absent, the diagnosis of pheochromocytoma can be missed in cases of atypical presentation.(3,4) There have been very few cases in which a pheochromocytoma mimics SSc or occurs in an SSc patient.(5)
In our case, a 57-year-old man presented with hand pain and facial skin thickening that rapidly progressed to the neck and both upper arms over a period of three months. Physical examinations indicate that the patient had Raynaud’s phenomenon (RP), which had appeared 12 months before, with sclerodactyly (
Fig. 1
(a) Photograph shows diffuse oedema, depigmentation and sclerodactyly on both hands. (b & c) Nailfold capillaroscopy images show microhaemorrhage and a minimal avascular area.

Fig. 2
(a) CT image shows a 5.4 cm × 4.2 cm enhanced mass with central dense calcification in the left adrenal gland (black arrowheads). (b) PET-CT image of the same area shows a 5.4-cm hypermetabolic mass with calcification in the left adrenal gland (white arrowheads).
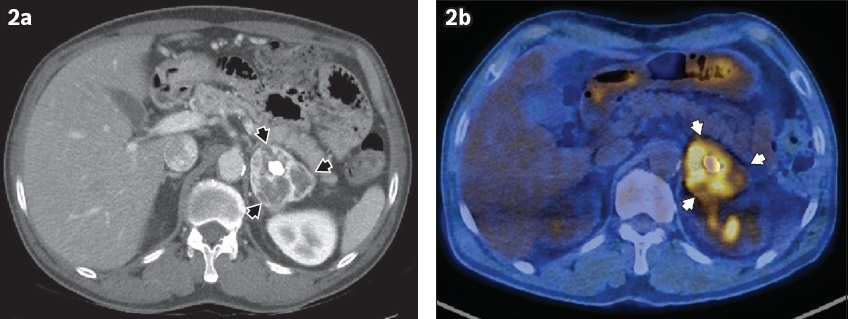
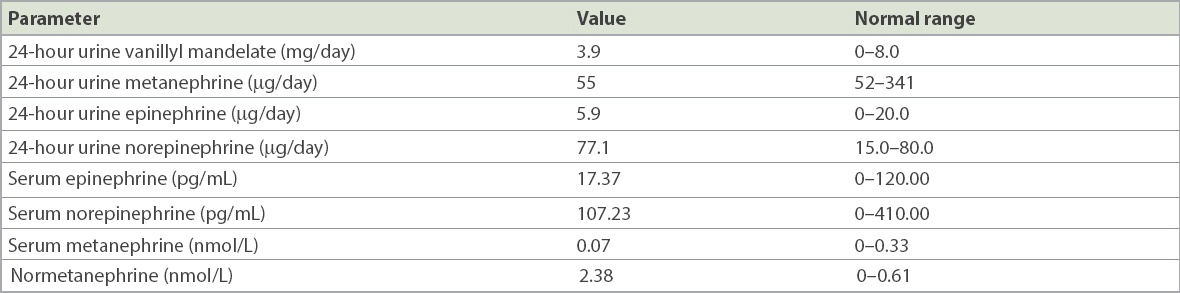
Table I
Test results of the patient.
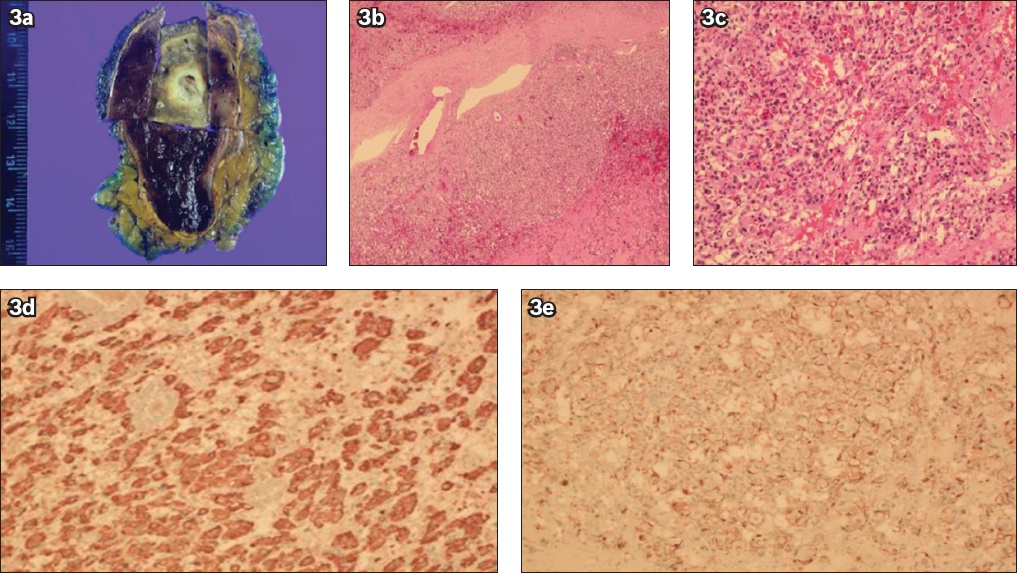
The patient underwent a laparoscopic adrenalectomy because his elevated normetanephrine levels could have resulted from a pheochromocytoma. A remnant of the adrenal cortex was seen in cross-sections of the adrenal gland, with a 5.5-cm mass showing a solid grey/white surface with haemorrhage and degenerative changes. Microscopy showed polygonal tumour cells with abundant granular cytoplasm arranged in a Zellballen pattern. After staining, chromogranin A and S100 protein tests were positive, the Ki-67 score was 1%, and the Pheochromocytoma of the Adrenal Gland Scaled Score was less than 4 (
Fig. 3
(a) Cross-sectional photograph shows a remnant of the adrenal cortex with a tumour mass that has a solid grey/white surface with haemorrhage and degenerative changes. Photomicrographs show (b) a well-demarcated capsule and tumour cells with a Zellballen pattern (Haematoxylin & eosin [H&E], × 40) and (c) the syncytial architecture of the tumour cells with abundant granular cytoplasm (H&E, × 200). (d & e) Photomicrographs with immunohistochemical staining show chromogranin-positive tumour cells (H&E, × 200) and S100-protein-positive sustentacular cells (H&E, × 200).
Our case demonstrates rapid progression of skin sclerosis precipitated by a pheochromocytoma in a middle-aged male SSc patient. The patient had RP, one of the most important characteristics of SSc, that was aggravated by vasospasm due to the adrenergic effects of the pheochromocytoma. In such patients, RP can be prolonged and result in ischaemic ulceration or infarction. Although pheochromocytoma rarely presents with acute limb ischaemia, significant negative correlations between plasma concentrations of catecholamine and dermal blood flow have been demonstrated in patients with pheochromocytoma.(4,6) The very high levels of catecholamine production may explain the persistent arterial vasospasm and critical peripheral ischaemia.(6,7) Our patient showed rapid progression of known SSc when incidentally diagnosed with pheochromocytoma, and this may have contributed to the progression of his disease.
Yours sincerely,
Acknowledgement
This study was supported by funding from Soonchunhyang University, Republic of Korea.


