Abstract
A 47-year-old man presented with a scrotal swelling. Ultrasonography of the testes showed that it was an extratesticular swelling. However, the swelling was intraoperatively found to be intratesticular. Histology showed an intratesticular leiomyoma, which is extremely rare.
INTRODUCTION
Leiomyomas are benign tumours that arise from smooth muscle cells. In the urinary tract, they may arise from the renal pelvis, bladder, spermatic cord, epididymis, prostate, glans penis or the scrotum. Intratesticular leiomyoma is extremely rare and only five cases have been reported in the literature thus far.(1) We herein present a case of intratesticular leiomyoma that was recently encountered in our institution.
CASE REPORT
A 47-year-old Chinese man presented with an asymptomatic left scrotal mass of three years’ duration. He had sought treatment only recently as the mass felt firmer. He did not report tenderness or any urinary symptoms such as haematuria or dysuria. There were no constitutional symptoms such as night sweats and loss of appetite or weight. He had no past surgical history or medical history of note.
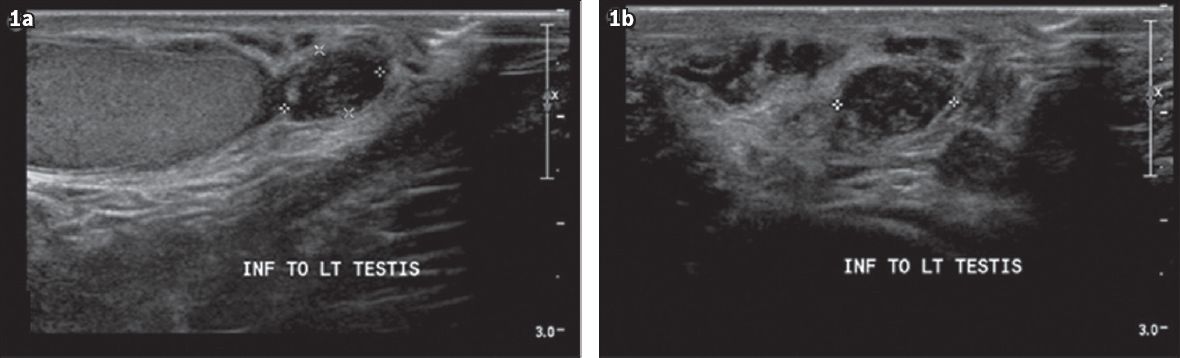
On physical examination, he had a firm nodule measuring 1 cm × 1 cm on the lower pole of his left testis, while his right testis was normal. Serum tumour markers showed a slightly raised serum lactate dehydrogenase (581 U/L) while alpha fetoprotein and beta human chronic gonadotropin levels were not elevated. Ultrasonography (US) of the testes showed a hypoechoic lesion measuring 1.1 cm in diameter adjacent to the lower pole of the left testes (
Fig. 1
Scrotal US images show (a) anteroposterior view and (b) lateral view of the left testis (3.3 cm × 2.7 cm × 1.2 cm) with the hypoechoic lesion adjacent to the lower pole of the left testis (1.1 cm × 1.0 cm × 0.7 cm). No significant internal vascularity was demonstrated and the lesion was reported as extratesticular.
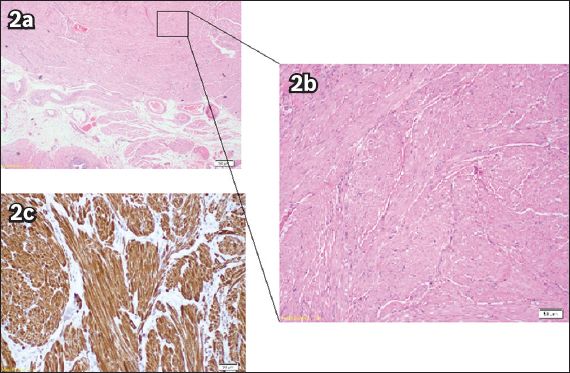
Histology showed a whitish nodule that measured 1.5 cm in dimension macroscopically. Microscopically, the sections revealed a circumscribed tumour adjacent to the epididymis. The tumour was composed of interlacing bundles of smooth muscle that did not reveal any cytologic atypia or coagulative necrosis. Mitosis was inconspicuous and there was no evidence of malignancy. Immunohistochemical studies showed that the smooth muscle cells were diffusely positive for smooth muscle and desmin (
Fig. 2
(a & b) Photomicrographs show a circumscribed tumour adjacent to the epididymis. [Haematoxylin & eosin (a) × 40; (b) × 100]. (c) Immunohistochemical studies show that the smooth muscle cells are diffusely positive for smooth muscle and desmin. The features of the tumour are thus in keeping with those of a leiomyoma.
DISCUSSION
Most solid intratesticular masses are malignant, including germ cell and non-germ cell tumours, metastatic lesions, lymphoma and leiomyosarcoma, which is a rare malignant primary testicular tumour that presents with painless testicular enlargement and normal tumour markers, especially in the elderly. Other benign differential diagnoses include rare solid tumours such as epidermoid cyst, Leydig cell hyperplasia, fibroma of gonadal stromal origin, testicular haemangioma, leiomyoma and testicular haemorrhage (which can be spontaneous) as well as sarcoidosis and tuberculosis. Genitourinary tuberculosis is believed to be spread haematogenously; the primary landing sites are usually the kidney, epididymis, prostate and fallopian tubes in women. In the epididymis, there is typically a nodular lesion that is adherent to the overlying skin. It may ulcerate through and form a sinus, usually on the posterior surface of the scrotum. The infection can also spread to the vas deferens, leading to a classical beaded vas, and into the testis, causing a mass that is clinically similar to a malignant lesion.
In the case of this patient, the lesion was stable in size on serial US and reported to be extratesticular. Physical examination on several occasions revealed a small benign tumour with no overlying skin changes. We considered the diagnosis of a benign lesion; hence, an excision biopsy rather than radical orchidectomy was performed.
Leiomyomas are benign tumours that arise from smooth muscle cells. In the urinary tract, they may arise from the renal pelvis, bladder, spermatic cord, epididymis, prostate, glans penis or scrotum. Intratesticular leiomyoma is extremely rare and only five cases have been reported in the literature thus far,(1) with our case being the sixth such case. Intratesticular leiomyoma most commonly presents in the fifth decade of life and as a nontender scrotal swelling.(2)
Leiomyomas may arise from any structure containing smooth muscle cells, including those found in the tunica propria of the seminiferous tubules or the tunica albuginea of the testis.(2) They are diagnosed on histology and are commonly described as well-circumscribed lesions with a whorled cut surface on gross inspection.(3) Microscopically, they stain positively for desmin and smooth muscle actin.(2) Diagnosing leiomyomas preoperatively on US remains a challenge. Some cases have reported a whirling pattern with multiple narrow areas of shadowing and no obvious calcifications.(4,5)
In conclusion, intratesticular leiomyoma is an extremely rare benign neoplasm. As solid testicular masses are often malignant, given the difficulty of diagnosing testicular leiomyoma preoperatively and the rarity of this entity,(1,3) radical orchidectomy remains the surgical option of choice.


