Dear Sir,
Marantic endocarditis is found in approximately 1%–1.5% of adults during autopsy.(1) There are few cases of marantic endocarditis associated with mucin-producing adenocarcinomas of any primary origin.(2) Malignancy causes a rise in tumour necrosis factor and interleukin-1, leading to thrombi formation in marantic endocarditis, as reported in a patient with adenocarcinoma of an unknown primary site by Schlittler et al.(3)
A 68-year-old woman with underlying Stage IV epidermal growth factor receptor (EGFR) mutant adenocarcinoma of the right lung presented with one-week history of visual blurring in her right eye. On examination, she had right homonymous hemianopia. Magnetic resonance (MR) imaging of the brain showed infarction in the left occipital territory. The patient was started on oral aspirin 100 mg (Cardiprin®) once daily. Five months later, the patient had diplopia and right-sided horizontal nystagmus on looking to the right. T2-weighted MR imaging of the brain showed a new hyperintense area in the right cerebellum. MR angiography was normal. Transthoracic echocardiography did not show any vegetation. Oral aspirin was substituted with oral clopidogrel 75 mg (Plavix®) once daily. Three weeks later, the patient developed new symptoms, including intermittent visual blurring. She had perception to light with her left eye and ability to read large letters of the alphabet with her right eye. The patient was afebrile. There was no peripheral stigmata of infective endocarditis or audible cardiac murmur. Blood cultures were normal.
Transoesophageal echocardiography (TOE) performed on the same day revealed a sessile vegetation measuring 7 cm × 6 cm on the non-coronary cusp of the aortic valve (
Fig. 1
Transoesophageal echocardiograph shows a sessile vegetation (arrow), measuring 7 cm × 6 cm, attached to the non-coronary cusp of the aortic valve.
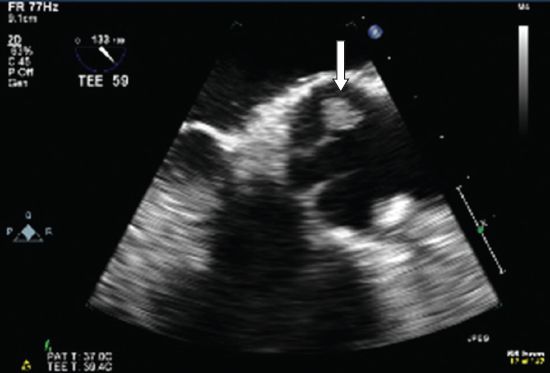
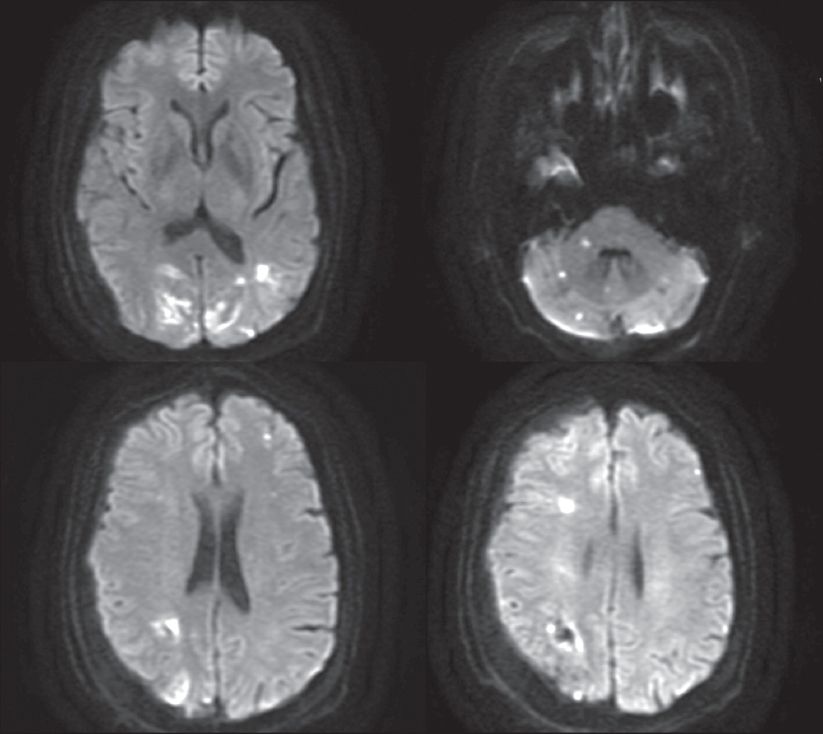
Fig. 2
Diffusion-weighted MR images show multiple variable-sized acute infarcts (restricted diffusion) in the anterior circulation and posterior circulation territories.
To our knowledge, this is the first case of recurrent infarcts secondary to embolism due to marantic endocarditis in a patient with EGFR mutant adenocarcinoma of the lung. Thus far, there have been only 11 cases of marantic endocarditis in patients with lung cancer in the literature.(1-3) Heart murmurs are frequently absent in marantic endocarditis and the diagnosis is usually missed; TOE is therefore necessary.(2) In a previous study, 18% of patients with cerebral infarcts and malignancy had marantic endocarditis on TOE.(4) The presence of vegetation on the coaptation surface, normal valvular tissue and negative blood cultures are strongly indicative of marantic endocarditis.(5) Vegetation in marantic endocarditis appears small, irregular and has a broad base.(1) Marantic endocarditis does not cause bacteraemia.(1,4)
The likelihood of systemic embolism secondary to marantic endocarditis is high (42%–50%).(1,3) The incidence of stroke due to marantic endocarditis (33%) is higher compared to infective endocarditis (19%).(1,3) Infarcts due to marantic endocarditis tend to be multiple and variable-sized, with different characteristics from infarcts due to intracranial stenosis; the latter are commonly encountered in Asians and follow particular arterial territories.(1,3,5) In addition, Pons et al reported that anticoagulation with intravenous heparin does not play a role in the prevention of strokes in marantic endocarditis.(6)
In conclusion, the diagnosis of marantic endocarditis should be suspected in patients with underlying lung adenocarcinoma who have recurrent embolic infarcts in the anterior and posterior circulation territories.


