Abstract
INTRODUCTION
Syme amputation has been shown to have value in patients with diabetic foot infections, but it has inherent drawbacks. A potential alternative is the modified Pirogoff amputation. Our objective was to evaluate the outcome of modified Pirogoff amputation using internal fixation with 6.5-mm cannulated screws in the management of diabetic foot.
METHODS
This is a prospective study of 13 patients admitted from January 2012 to June 2015. Inclusion criteria were infection limited to the forefoot, presence of a palpable posterior tibial pulse and an ankle-brachial index of more than 0.7. Internal fixation of the calcaneum to the tibial was performed using two 6.5-mm cannulated screws under image intensifier control.
RESULTS
In ten cases, the wounds were healed at three weeks. Osseous union was observed in ten cases; the time taken for its occurrence was 2–5 months. Removal of screws was performed in five cases. Five cases developed technical complications of screw tract infection, with two cases having distal screw migration. Good results, defined as cases not requiring a below-knee amputation for two years postoperatively, were obtained in 10 (77%) cases. At the three-year follow-up, three additional cases required proximal amputation, leaving 7 (54%) cases with good outcomes.
CONCLUSION
Our prospective study showed that with careful selection of patients, good postoperative results can be obtained. There is a definite role for modified Pirogoff amputation in the management of diabetic foot problems.
INTRODUCTION
Syme amputation has been shown to have value in patients with diabetic foot infections compared to transtibial amputations,(1) with a variable success rate of 50%–88% in wound healing.(2,3) Furthermore, diabetic patients with a positive posterior arterial circulation can also attain a functional level of ambulation with the Syme amputation.(4) However, the Syme amputation still has disadvantages, including instability of the calcaneal flap, leading to poor adherence to the raw tibial surface; devascularisation from the dissection of the calcaneum from the underlying flap; and significant limb length discrepancy of about 4–5 cm, which can make walking difficult.(3-6)
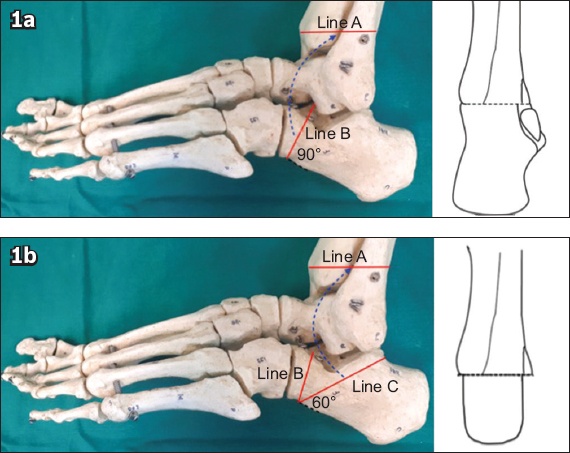
Pirogoff described an amputation of the foot at the level of the malleolus that included partial preservation of the calcaneum, unlike the Syme amputation. In Pirogoff amputation, the calcaneum is cut at an angle of 90° and fused to the raw tibial surface (
Fig. 1
Photographs show (a) original Pirogoff 90° calcaneal osteotomy (Line B) with fusion to the tibia cut (Line A); and (b) modified Pirogoff osteotomy with distal calcaneal cut (Line B) and a 60° oblique cut (Line C). After removal of the wedge, the oblique osteotomised calcaneal surface (Line B) is fused to the raw tibia (Line A), resulting in a smaller stump compared to the original technique.
We have previously described the modified Pirogoff amputation using cannulated screws in a cross configuration, with good outcomes after the initial follow-up period of ten months.(6) The objective of this study was to evaluate the long-term outcomes of our modified Pirogoff amputation cohort at one, two and three years.
METHODS
This is a prospective study of 13 cases that underwent a modified Pirogoff amputation from January 2012 to June 2015. Inclusion criteria for the operation included infections limited to the forefoot, presence of a palpable posterior tibial pulse and an ankle-brachial index (ABI) of more than 0.7.(9) Determination of the zone of infection requires clinical experience and a thorough clinical assessment. Signs of infection, such as cellulitis and swelling, should be limited to the metatarsals. Clinical examination is assisted by radiography and magnetic resonance imaging to ensure clear flap margins.
Parameters studied included demographic data (age, gender and ethnicity), duration of diabetes mellitus, glycated haemoglobin level and the presenting diabetic foot problem. Clinical parameters recorded included the presence of a palpable dorsalis pedis and posterior tibial pulse, pulp capillary refill time, ABI and Semmes-Weinstein monofilament test (SWMT) score. Haematological parameters evaluated included total white blood cell (WBC) count, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and haemoglobin (Hb), albumin and creatinine levels. Time of wound healing and time taken for osseous union to occur were studied. Complications of the modified Pirogoff amputation were documented, and subsequent surgery required was described.
All patients were started on intravenous co-amoxiclav after tissue culture was taken during the operation. They were subsequently administered the antibiotic of choice based on the antibiotic sensitivity of the intraoperative cultures taken. All 13 cases were internally fixed with two 6.5-mm cannulated screws inserted from the calcaneum into the talus (
Fig. 2
(a) Radiographs and (b) clinical photo show tibio-calcaneal fusion and a healed modified Pirogoff stump.

RESULTS
The age of our cohort ranged from 46 to 67 years (average 54.6 years). Seven patients were male and six were female. There were four Chinese, four Malay and five Indian patients. All cases were admitted due to diabetic foot infections, ranging from abscesses to osteomyelitis, that were confined to the forefoot (
Table I
Patient demographics of the cannulated screw group (n = 13).
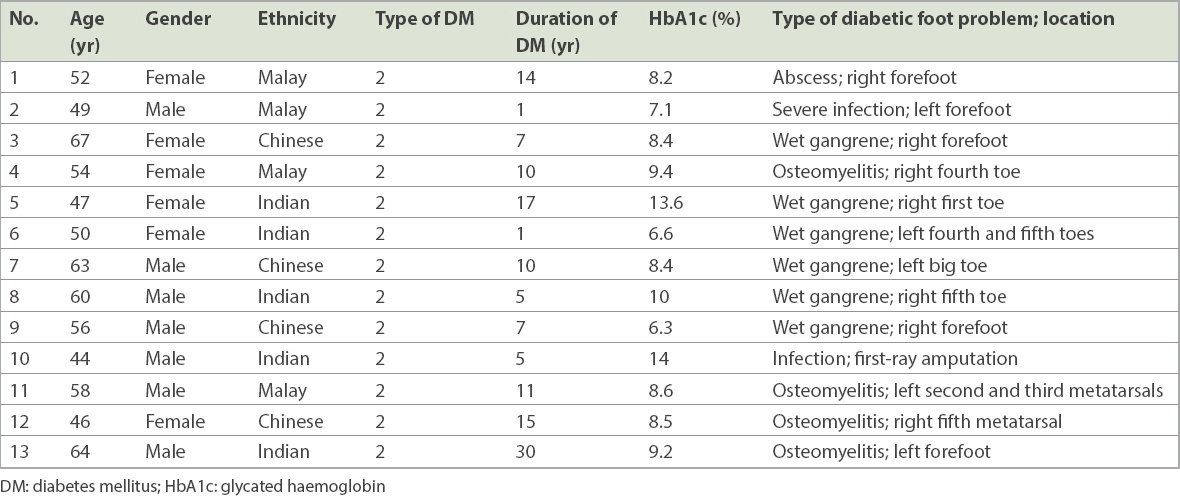
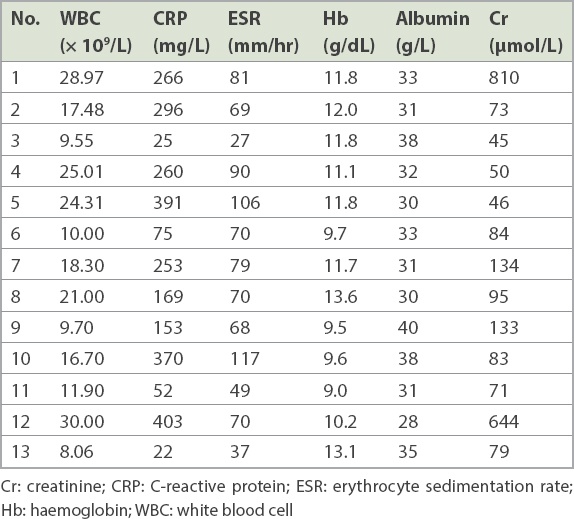
All cases had palpable posterior tibial pulses and an ABI of more than 0.7. Pulp capillary refill time was less than two seconds in all patients. Nine patients had an SWMT score of < 8 (loss of protective sensation). This is further illustrated in
Table II
Clinical vascular examination.
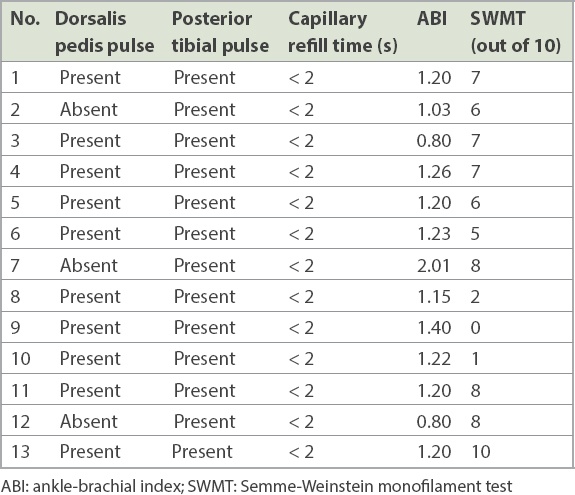
The results of the initial investigations on admission are detailed in
Table III
Initial investigations on admission.
Wounds were healed at three weeks in ten patients (
Table IV
Outcome and long-term follow-up.
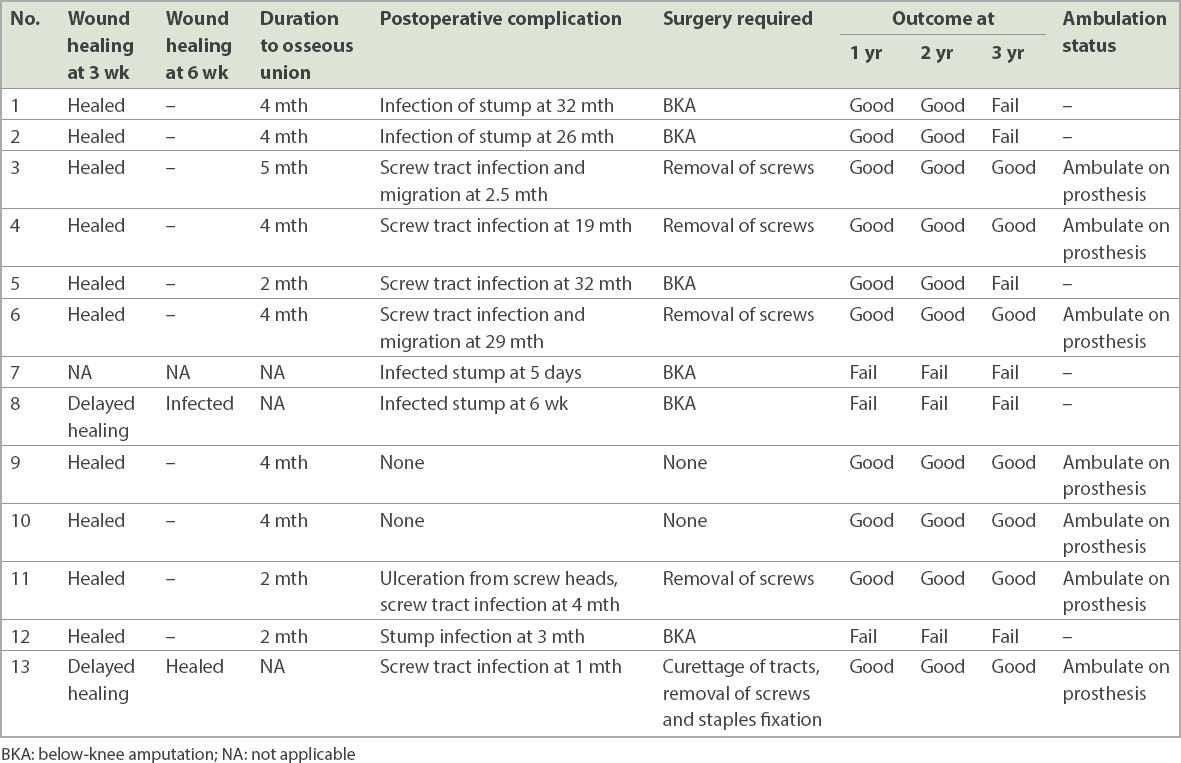
Good results (i.e. not requiring a below-knee amputation) were seen in 10 (77%) out of the 13 cases at one year. At two years, good results continued to be seen in all ten cases. At three years, an additional three cases required a BKA, leaving good results in only 7 (54%) cases.
DISCUSSION
In 1854, Russian surgeon Nikolai Ivanovich Pirogoff first described the surgical technique for an amputation that was subsequently named after him.(10) His initial technique involved amputation of the foot at the level of the malleolus, with preservation of the calcaneum and a posterior skin flap. Calcaneal osteotomy perpendicular to the calcaneal axis was then performed, and the flap was folded upward and forward to create a weight-bearing stump. Stabilisation of the bony interface was originally achieved using an external cast. The lack of suitable options for tibiocalcaneal osteosynthesis partially contributed to its relatively limited early use.(10)
Recently, the modified Pirogoff amputation has started to regain popularity with internal fixation techniques for a variety of indications. In 1995, Rijken described successful use of a modified Pirogoff amputation with the calcaneum cut parallel to the posterior talocalcaneal facet (approximately 50°) in six patients with severe traumatic foot injuries, with a good outcome in all cases.(11) In 2003, Taniguchi et al reported a case series of modified Pirogoff amputations for 11 patients (for 12 ankles) for a variety of indications (including osteomyelitis, metastatic tumour and traumatic cases). He obtained good results in patients without peripheral vascular disease, with 73% having a good outcome.(5) Langeveld et al and den Bakker et al reported similarly successful results for infective/ischaemic necrosis and trauma, respectively, in their case reports.(12,13) In a subsequent paper in 2011, Langeveld et al recommended a modified 60° calcaneal cut to improve the weight-bearing axis of the stump.(7) Most recently in 2014, Nather published a case series with six patients describing the surgical technique of the modified Pirogoff amputation with cannulated screws with good results in all patients at ten months of follow-up.(6)
We performed the modified Pirogoff amputation for diabetic foot infections with strict inclusion criteria of infections limited to the forefoot, presence of a palpable posterior tibial pulse and an ABI of more than 0.7. With such carefully selected patients, a good outcome was seen in ten out of 13 cases at the one- and two-year follow-up. This outcome is superior to that of the Syme amputation. Frykberg et al, in a study of 26 cases of the Syme amputation in 2007, reported that good outcomes were seen in 12 (46.2%) cases. However, ten out of the 26 cases subsequently required BKA, at an average of 27.7 weeks postoperatively. They also reported three mortalities in their series.(14) On the other hand, Pinzur et al performed a retrospective study of 97 patients with diabetic foot infections who underwent Syme amputation, with a minimum of two years’ follow-up. They observed good outcomes in 80 (82.5%) patients, but there was a mortality of 30 (30.9%) out of 97 patients at an average of 57.1 months following surgery.(2) In our cohort, at the three-year follow-up, there were no mortalities and good results were still obtained in seven out of 13 cases.
However, we did noted a high incidence of technical complications with a two-screw technique. Five cases developed screw tract infection, with two cases having distal screw migration in addition to the infection. The senior author proposes that in the future, cannulated screws be used in conjunction with surgical staples (size 18, Smith and Nephew, Memphis, TN, USA) for internal fixation. He further recommends that the cannulated screws be removed at six months, following successful osseous union, to reduce the problem of pin tract infections and distal screw migration.
The limitations of our study are its small sample size and a relatively short follow-up. Furthermore, this was a single series study that did not have a control arm.
In conclusion, our prospective study showed that with careful patient selection, good results can be obtained with the modified Pirogoff amputation for diabetic foot infections. At the one- and two-year follow-up, we had ten cases with good outcomes; at the three-year follow-up, we had seven cases with good outcomes. There is a role for the modified Pirogoff amputation in the management of diabetic foot problems. Our modified Pirogoff amputation had a 54% overall success rate at three years.


