Abstract
The anterior cruciate ligament (ACL) is an important stabiliser of the knee and is commonly torn in sports injuries. Common indications for imaging after ACL reconstruction include persistent symptoms, limitation of motion and re-injury. Important postoperative complications include graft failure, impingement, arthrofibrosis and graft degeneration. This article aimed to familiarise the radiologist with magnetic resonance (MR) imaging appearances of properly positioned intact ACL grafts and to provide a comprehensive review of MR imaging features of complications following ACL reconstruction.
SURGICAL ASPECTS OF ACL RECONSTRUCTION
The goal of anterior cruciate ligament (ACL) reconstruction is to restore knee function that is identical to that of the native ligament and prevent long-term irreversible damage. ACL reconstruction remains the gold standard of care, particularly in active patients in whom non-operative management has been shown to result in poorer functional outcome.(1) The timing of surgery and type of graft utilised continue to be the subject of debate. For most patients, early reconstruction (within 21 days) is preferred over delayed surgery.(2)
Graft types
Autografts are considered the gold standard. Allograft constructs are occasionally used, but they are comparatively more prone to mechanical failure and are associated with increased synovitis and osteolysis.(3) The two autografts commonly used for ACL reconstruction are patellar tendon and hamstring grafts.
Patellar tendon graft
Patellar tendon grafts (
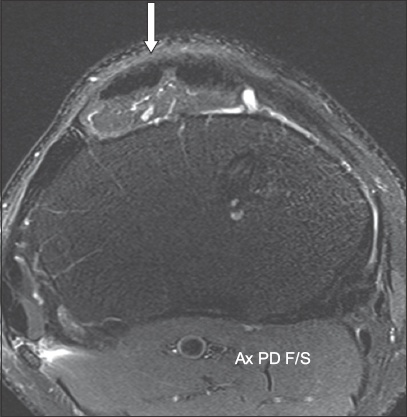
Fig. 1
Axial proton density fat-saturated MR image following anterior cruciate ligament reconstruction using a patellar tendon graft shows scarring (arrow) in the central third of the patellar tendon, where the graft was harvested.
Hamstring tendon graft
Hamstring grafts (
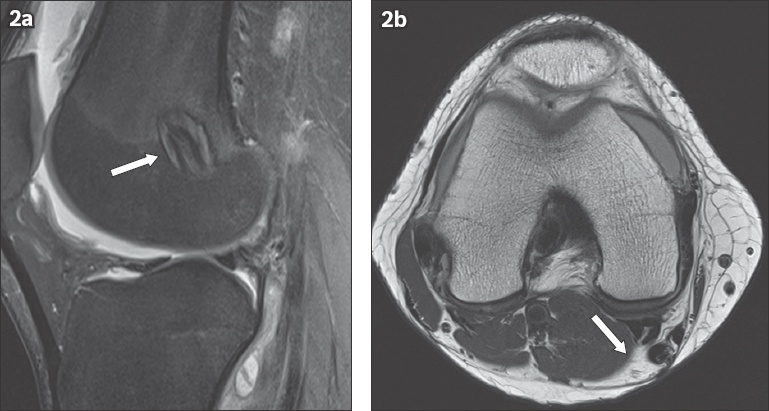
Fig. 2
A patient with anterior cruciate ligament reconstruction using a hamstring graft. (a) Sagittal proton density (PD) fat-saturated MR image shows a looped appearance of the grafts (arrow) within the femoral tunnel, differentiating them from patellar grafts. (b) Axial PD MR image shows the regenerated tendons (arrow) one year post surgery. Regeneration makes identification of prior graft harvesting difficult.
Optimal graft placement
The current surgical practice is to place the femoral tunnel within the femoral footprint of the native ACL.(2) In order to achieve optimal function, the femoral tunnel should not be placed anterior to the lateral intercondylar ridge, an anatomical landmark that can be found during surgery.(2)
The ideal tibial insertion site of the graft is the posterior aspect of the tibial footprint, located close to where the posterolateral band of the native ACL would be inserted. A tunnel placed too anteriorly predisposes the graft to impingement against the roof of the intercondylar notch during extension.(4)
MR APPEARANCES OF NORMAL ACL GRAFTS
In the first three months following ACL surgery, the grafts are avascular and demonstrate a similar magnetic resonance (MR) signal to the native harvest site (
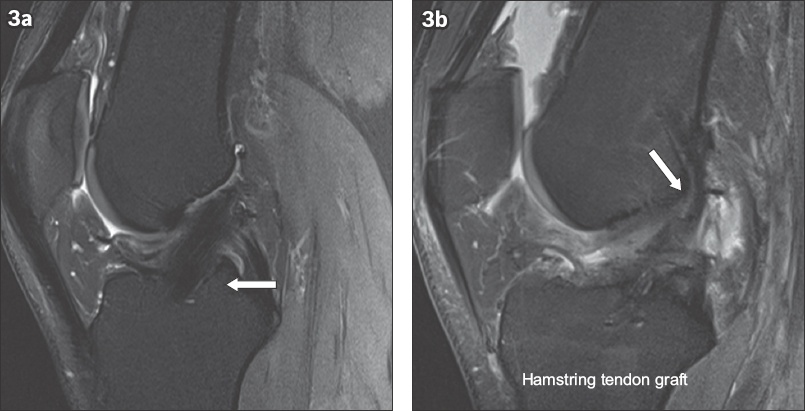
Fig. 3
Sagittal proton density fat-saturated MR images show (a) the homogeneous low signal of a patellar tendon graft (arrow) and (b) normal linear striations (arrow) of separate bundles in the hamstring graft.
Optimal femoral tunnel position
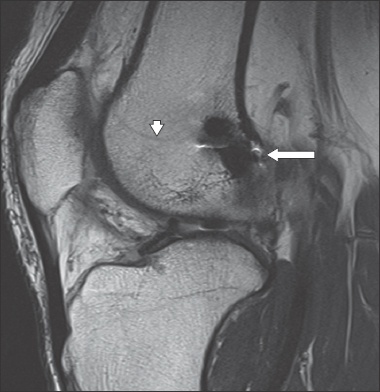
The optimal position of the femoral tunnel is along the posterior femoral intercondylar notch, immediately at the intersection of the posterior femoral cortex and the posterior physeal scar (
Fig. 4
Sagittal proton density MR image shows a satisfactory femoral tunnel (arrow) at the intersection of the posterior femoral cortex and the posterior physeal scar (arrowhead).
Optimal tibial tunnel position
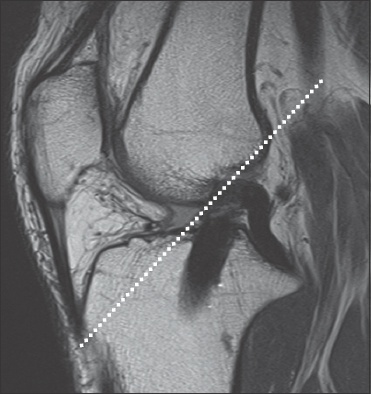
The tibial tunnel is optimally positioned when the anterior margin of the tunnel lies just posterior to the roof of the intercondylar notch, as represented by Blumensaat’s line (
Fig. 5
Sagittal proton density MR image shows a Blumensaat’s line (dotted line), which parallels the roof of the intercondylar notch. A satisfactory tibial tunnel is also seen posterior to the Blumensaat’s line.
POSTOPERATIVE COMPLICATIONS
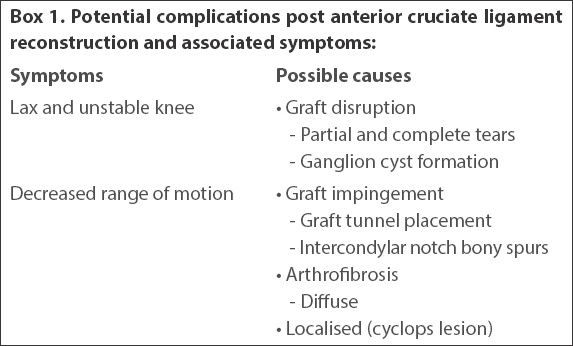
Complications following ACL reconstruction can be broadly categorised into two groups based on the presenting symptoms (
Box 1
Potential complications post anterior cruciate ligament reconstruction and associated symptoms:
Graft disruption
Complete and partial tears of ACL grafts can result in lax and unstable knees. Disruption of the posterolateral bundle is more common than that of the anteromedial bundle. A study by Amin et al(5) demonstrated partial tears of the posterolateral bundle in 27% of post-ACL knees and complete tears in 24% of them. The MR appearances of a complete tear of an ACL graft is similar to that of a complete tear of a native ACL, with abnormal orientation of the fibres and complete discontinuity (
Fig. 6
(a) Sagittal proton density (PD) fat-saturated and (b) coronal PD MR images show complete loss of continuity of the anterior cruciate ligament (ACL) graft fibres with a remnant graft stump (arrows in a & b). Complete graft rupture was confirmed on arthroscopy and the patient underwent ACL revision surgery.
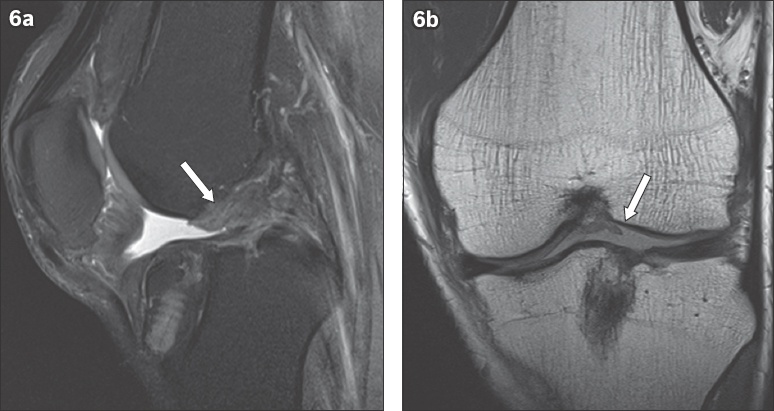
Fig. 7
(a) Sagittal proton density and (b) T2-W fat-saturated MR images show a partial tear with discontinuity and increased signal (arrows in a & b) in the anterior cruciate ligament graft.
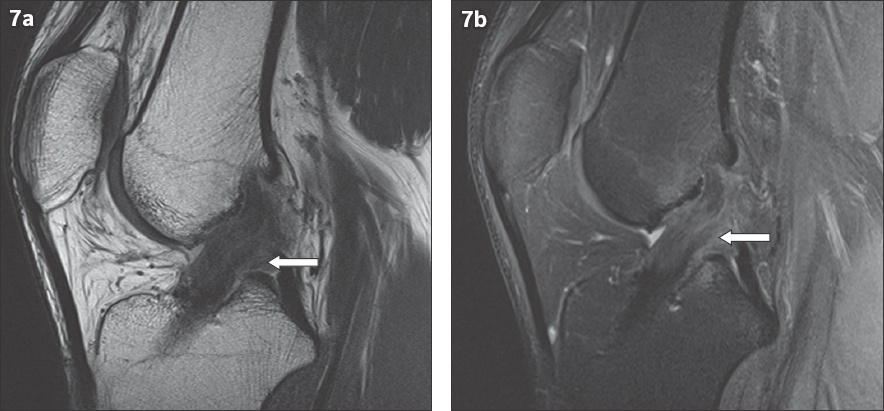
The ACL graft, particularly the patellar bone tendon graft, often shows an intermediate signal for up to two years post surgery, and this should not be mistaken for a tear. In such cases, the fibres remain intact, unlike in a partial tear.
ACL graft ganglion
Ganglions may form along ACL grafts and, if large enough, may lead to expansion or even lysis of the femoral or tibial tunnel and consequently pain and/or instability of the knee (
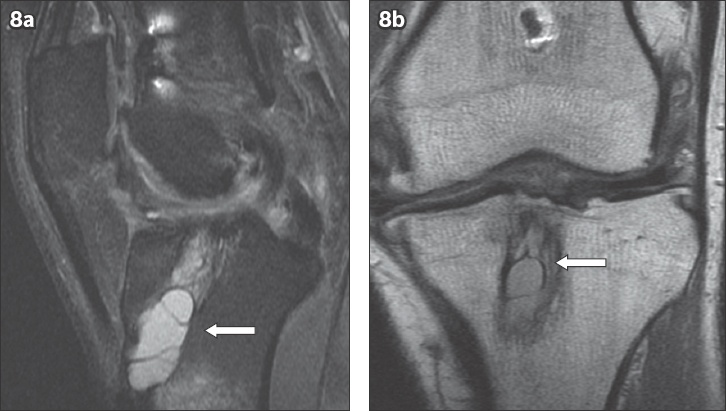
Fig. 8
(a) Sagittal proton density (PD) fat-saturated and (b) coronal PD MR images show a lobulated septated cystic lesion (arrows in a & b) within the tibial tunnel. Tunnel expansion is seen.
Graft impingement
If the tibial tunnel is placed too far anteriorly, it leads to chronic mechanical stress and impingement of the graft, which in turn leads to degeneration and tear. Intercondylar roof impingement usually affects the anterior surface of the graft before extension to involve the posterior fibres. Another cause of impingement is osseous spurs in the intercondylar notch (
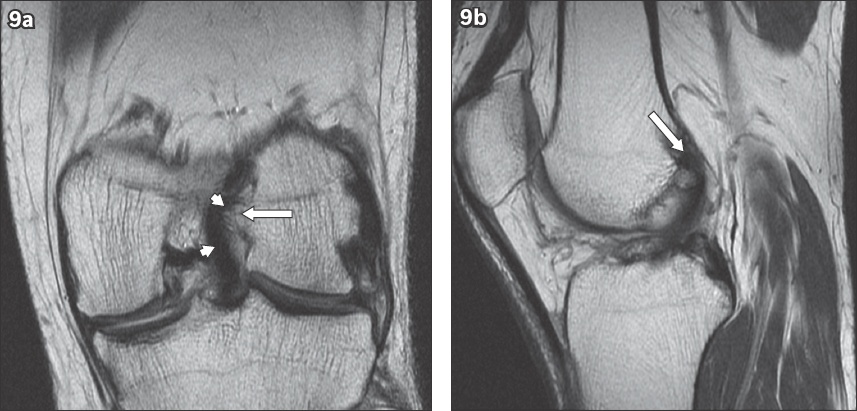
Fig. 9
(a) Coronal proton density (PD) and (b) sagittal PD MR images show an osseous spur (arrows in a & b) arising from the medial aspect of the lateral femoral condyle, causing bowing of the anterior cruciate ligament graft (arrowheads), although no abnormal graft signal is shown.
Arthrofibrosis
Arthrofibrosis refers to scar tissue within the knee and is a common cause of decreased range of motion of the knee following ACL reconstruction. It can either be diffuse, involving multiple compartments of the knee (
Fig. 10
(a) Sagittal proton density, (b) Sagittal T2-W and (c) axial gradient-recalled echo MR images show both forms of arthrofibrosis. A spiculated area of low signal intensity within the Hoffa’s fat pad represents diffuse arthrofibrosis (arrowheads in a–c). A cyclops lesion (arrows in a–c) is also present.
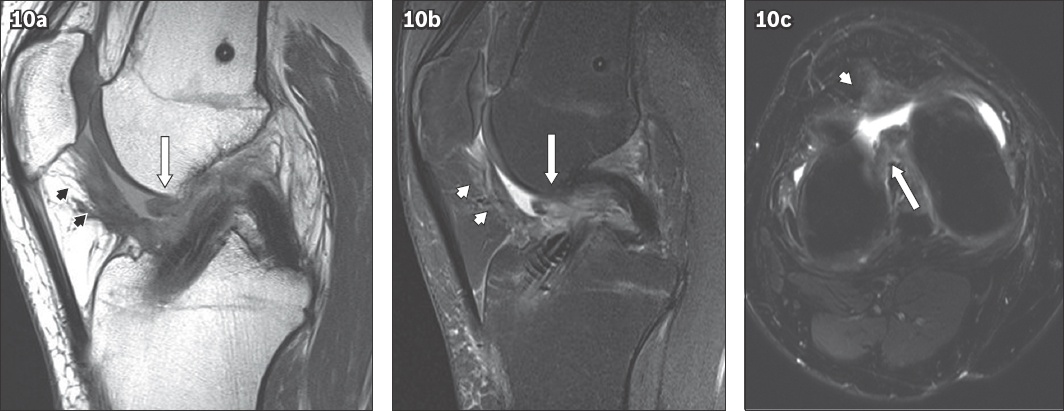
Fig. 11
(a) Sagittal proton density (PD) fat-saturated, (b) coronal PD and (c) axial PD MR images show a focal nodular low signal area anterior to the intra-articular portion of the anterior cruciate ligament graft, in keeping with a cyclops lesion (arrows in a–c).
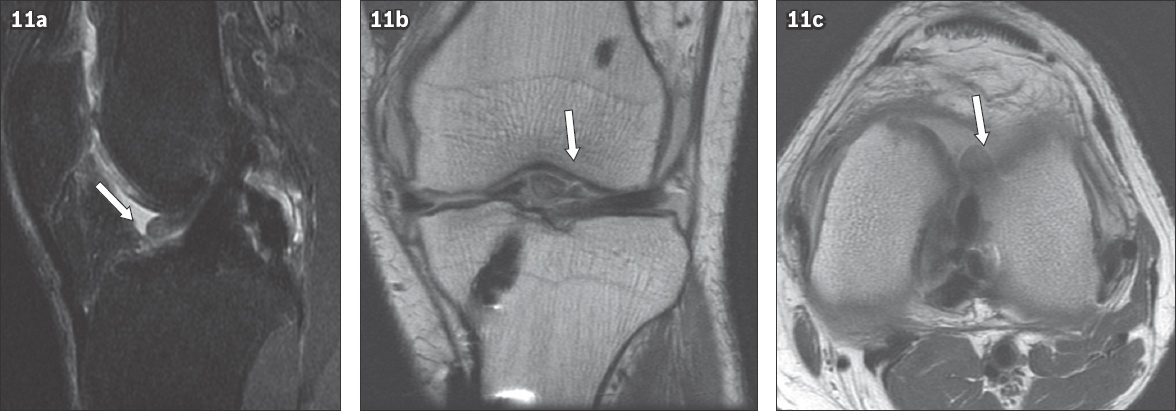
Cyclops lesions are seen in approximately 1%–10% of post-ACL reconstruction patients.(7) The key finding is soft tissue thickening anterior to the distal ACL, usually seen as low to intermediate signal on T1-weighted and T2-weighted MR imaging.
Donor site complications
Donor site complications are more common with patellar tendon grafts and include fractures of the patella, and partial or complete tears of the patellar tendon, bursitis and haematoma.(8) Following harvesting, it is normal to see tendon thickening and a central gap within the patellar tendon corresponding to the site of tendon harvesting, which usually fills in with reparative tissue by two years.(9) Donor site complications of hamstring tendon grafts are relatively rare, with the most common complication being a fluid collection at the donor site.
CONCLUSION
Postoperative complications can be evaluated accurately with MR imaging. Eliciting a clinical history of either an unstable knee or loss of normal range of motion is helpful in the assessment of associated complications. Knowing the normal appearance of the ACL graft and its changes over time can help to avoid potential pitfalls in imaging interpretation.
SMJ-60-68.pdf


