Abstract
Diagnostic errors can occur when physicians rely solely on computer electrocardiogram interpretation. Cardiologists often receive referrals for computer misdiagnoses of atrial fibrillation. Patients may have been inappropriately anticoagulated for pseudo atrial fibrillation. Anticoagulation carries significant risks, and such errors may carry a high cost. Have we become overreliant on machines and technology? In this article, we illustrate three such cases and briefly discuss how we can reduce these errors.
CASE 1 CLINICAL PRESENTATION
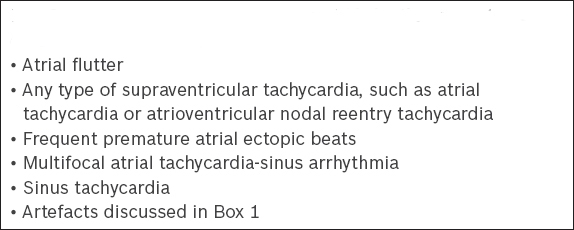
A 67-year-old asymptomatic woman was referred from primary healthcare services following a routine screening. The referral letter stated that she had atrial fibrillation with a CHA2DS2-VASc score of 2 and suggested anticoagulation therapy. During the clinic visit, the patient’s blood pressure was 130/90 mmHg and her heart rate was 60 beats per minute (bpm). Clinical examination was normal. The electrocardiogram (ECG) that had previously been performed (
Fig. 1
Case 1: Outpatient 12-lead ECG.
ECG INTERPRETATION
Computer interpretation of the ECG indicated that the diagnosis was atrial fibrillation with a heart rate of 53 bpm. However, in
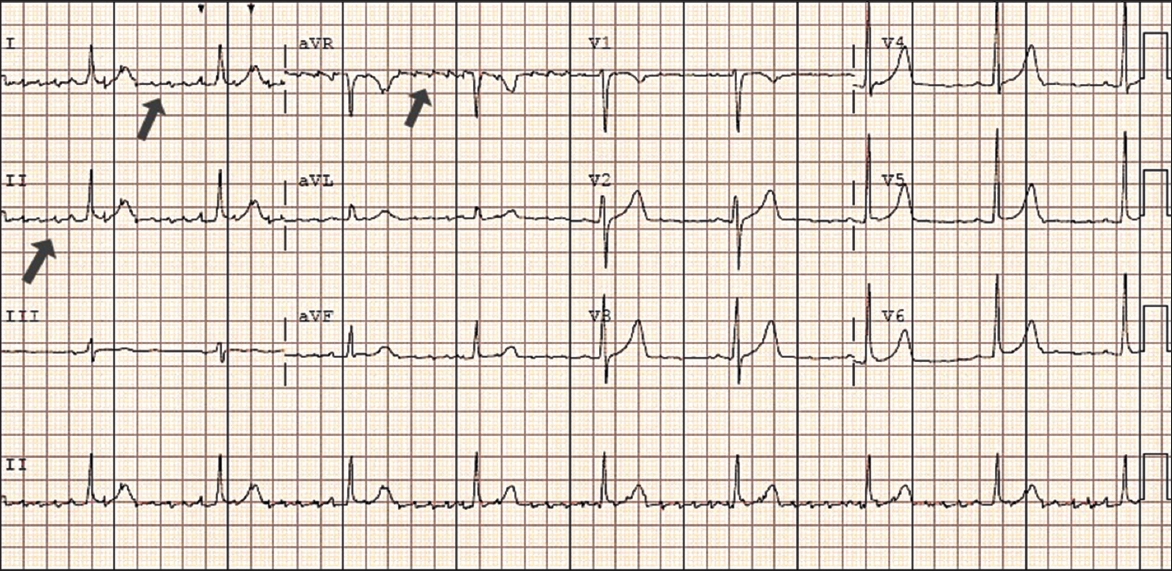
CASE 2 CLINICAL PRESENTATION
An 80-year-old man with dementia, chronic kidney disease and hypertension was admitted following a fall, presenting with an acute right parietal-temporal subdural haematoma. Computer analysis of the ECG done on arrival showed atrial fibrillation (
Fig. 2
Case 2: 12-lead ECG done at the emergency department.

ECG INTERPRETATION
Computer interpretation indicates an abnormal ECG with atrial fibrillation and a heart rate of 72 bpm. However, there are movement artefacts in
CASE 3 CLINICAL PRESENTATION
A 74-year-old woman with hypertension had a routine checkup, during which an ECG was performed and indicated atrial fibrillation. The patient was, however, asymptomatic. The physician started her on beta-blockers, and she subsequently presented to the cardiology clinic for further management of the newly diagnosed atrial fibrillation. She complained of increased lethargy after the initiation of beta-blockers.
Fig. 3
Case 3: Routine 12-lead ECG done at a clinic.
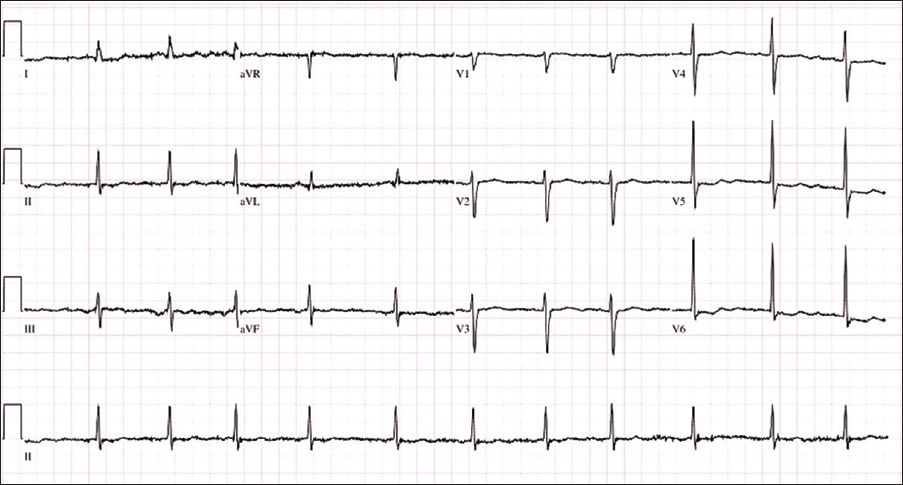
ECG INTERPRETATION
Computer interpretation of the ECG indicated atrial fibrillation, nonspecific ST and T wave morphology, and an abnormal ECG with a heart rate of 69 bpm. However, the P wave amplitude is small and can be easily missed. There is also a slight variation in the P-P interval due to physiological variation in the heart rate with respiration. Thus, the correct interpretation should be sinus arrhythmia.
DISCUSSION
With advances in medicine and computer technologies, it is inevitable that technology and clinical decision support systems (CDSSs) have infiltrated our healthcare system. Indeed, health information technology can aid physicians and allied health workers in making various clinical decisions. Multiple studies have suggested that CDSS helps to reduce medical errors and enhances patient safety.(1,2) An example of CDSS is the computer interpretation of ECGs. Various studies have shown that computer programs are able to identify non-arrhythmia-related ECG abnormalities as accurately as cardiologists.(3,4) However, their accuracy is reduced when it comes to the interpretation of arrhythmias such as atrial fibrillation.(5)
Diagnostic errors of ‘pseudo-arrhythmias’ appear to be increasing in frequency, despite the rapid advancement of technology and ECG detection algorithms. Quite frequently, cardiologists receive referrals for arrhythmias based on computer interpretation. Questions arise: Have we become overreliant on machines and technology? Have physicians even looked at the ECG tracing, or have they abandoned their ECG interpretation skills? Some have even advocated that we should do away with computer interpretations, lest the newer generations of doctors lose the art of ECG interpretation.
The cases discussed in this paper illustrate that computer interpretations can be inaccurate and may result in incorrect, and even harmful, management. A person who is misdiagnosed with atrial fibrillation could end up receiving cardioversion and anticoagulation treatments, which could lead to life-threatening bleeding complications. There are also monetary, psychological and social costs involved, as patients (and their accompanying relatives) may have to return for years of follow-up and unnecessary tests. The decision to anticoagulate for stroke prevention is based on the CHA2DS2-VASc score, which supersedes the CHADS2 score. The newer CHA2DS2-VASc score takes into account gender, a lower age group of 65–74 years and the presence of vascular disease, which was not reflected in the older CHADS2 score.(6)
Rather than allowing a computer program to be the ‘doctor’, physicians should use it to enhance their own performance. Computer interpretations can be used as a daily self-training tool to improve one’s accuracy and speed in ECG interpretation.(7,8) In order to prevent misdiagnoses such as those discussed in this paper, it is important to consider the patient’s clinical presentation and the findings of the physical examination. Alarm bells should ring when clinical findings are incongruent with computer interpretations.
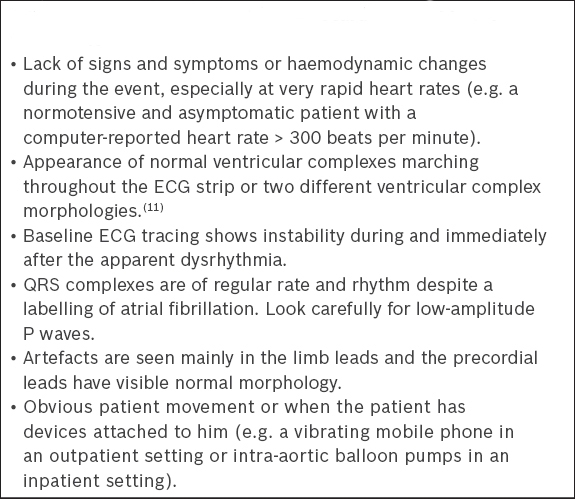
Furthermore, familiarity with common artefacts may enhance recognition of false arrhythmias. ECGs are often contaminated by artefacts that are of similar amplitude and frequency as P-QRS complex morphologies, and the machine has difficulty differentiating between them. Artefacts can be categorised into those that result from patient factors and those that result from environmental factors. Any issues along the chain – from the patient to the electrodes, cables and machine – can result in artefacts. The most common artefacts are electromyographic noise from the patient’s movement. These include voluntary movements of the limbs or involuntary movements such as hiccups, coughs or subtle tremors of Parkinsonism. Limb movement principally affects the limb leads, while deep respiration and chest wall movements can cause a drifting baseline of the chest leads. Environmental factors, such as electrical equipment interferences, can also lead to an abnormal ECG baseline, which may often look like fibrillation or flutter waves.(9)
Box 1
Features suggestive of electrocardiography artefacts that mimic atrial fibrillation and other arrhythmias
In conclusion, the ECG, like all other investigations, should always be interpreted in relation to the patient and the clinical scenarios. The computer is not, and should not be, a surrogate for a physician’s knowledge and clinical acumen but, when utilised appropriately, can certainly be a useful aid in clinical management.
SMJ-58-520.pdf