Abstract
INTRODUCTION
This study examined the efficacy and safety of cholangiopancreatoscopy via the SpyGlass™ system in routine clinical practice.
METHODS
The clinical data of endoscopic retrograde cholangiopancreatography (ERCP) performed in a regional hospital from January 2013 to November 2016 was retrieved from an electronic database and reviewed. All patients who had undergone SpyGlass cholangiopancreatoscopy were enrolled. Patient demographics, procedure indication, technical success rates, clinical success rates and complication rates were analysed. A subanalysis of clinical outcomes was performed comparing the SpyGlass legacy (fibreoptic) and digital systems.
RESULTS
Out of 2,050 ERCP procedures performed, 47 patients underwent 50 cholangiopancreatoscopy procedures. Clinical indications were difficult common bile duct (CBD) stones (59.6%, n = 28), indeterminate CBD stricture (36.2%, n = 17), indeterminate pancreatic duct stricture (2.1%, n = 1) and proximally migrated CBD stent (2.1%, n = 1). Complete stone extraction was achieved in 26 (92.9%) out of 28 patients. Among patients with strictures, a correct diagnosis of malignancy based on image visualisation was achieved in all 11 cases. The sensitivity and specificity for SpyBite™ biopsies were 81.8% (95% confidence interval [CI] 48.2%–97.7%) and 100.0% (95% CI 15.8%–100.0%), respectively. The proximally migrated CBD stent was successfully extracted. Complications included pancreatitis (2.1%, n = 1), suspected sealed perforation after laser lithotripsy treated conservatively (2.1%, n = 1) and cholangitis (10.6%, n = 5). There was no difference in clinical outcomes between the SpyGlass legacy (n = 20) and digital (n = 30) systems.
CONCLUSION
SpyGlass cholangiopancreatoscopy is a safe and effective tool in routine clinical practice.
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is a well-established modality for the diagnosis and management of a spectrum of benign and malignant pancreaticobiliary disorders. Common indications include common bile duct (CBD) stones and biliary obstruction from either benign or malignant disorders.(1) In specific situations, ancillary cholangiopancreatoscopy during ERCP is required in order to directly visualise the target lesion for biopsy or definitive therapy.(2) Cholangiopancreatoscopy during ERCP can be performed using a mother-baby scope system, an ultrathin gastroscope and the SpyGlass™ cholangioscopy system (Boston Scientific Corp, Marlboro, MA, USA). Single-operator cholangioscopy via the SpyGlass system is the simplest technique, because it uses a disposable 10-French cholangioscope inserted through the working channel of a standard duodenoscope that can be easily handled by a single endoscopist. In contrast, the mother-baby scope system requires two endoscopists to operate, while using an ultrathin gastroscope to perform ERCP is technically more difficult: as the diameter of the ultrathin gastroscope is larger, ranging from 4.9 mm to 5.8 mm, it cannot be used in non-dilated ducts.(2)
Since the first report of the clinical feasibility of SpyGlass cholangioscopy in 2007, data concerning its clinical utility has been published from multiple referral centres.(3) In the landmark initial multicentre registry study from the United States (US) and Europe with 297 patients, the overall procedure success rate was 89%. Adequate tissue was obtained for histological examination in 88% of 140 patients who underwent biopsy for stricture evaluation. Overall sensitivity was 78% for diagnosis of malignancy by visualisation but only 49% for biopsy. Procedure success, defined by protocol as visualisation and initiation of stone fragmentation and removal, was 92%, although the rate of complete stone clearance during the study’s SpyGlass session was lower, at 71%.(4) In the context of biliary stricture evaluation, Ramchandani et al (5) showed that the accuracy of SpyGlass visualisation was 89%, and in contrast to the study by Chen et al,(4) targeted biopsies achieved a higher accuracy rate of 82%. Comparing SpyGlass targeted biopsies with brush and blind biopsies, Draganov et al showed a significantly higher accuracy rate (84.6% vs. 38.5% vs. 53.8%).(6) Further publications confirmed the clinical utility of SpyGlass cholangioscopy in the management of a spectrum of pancreaticobiliary disorders.(7-20) Most studies have evaluated the first generation SpyGlass system, whose optical view has a somewhat limited resolution due to the analogue design of the optical probe. The new digital SpyGlass system became commercially available in 2015 and has significantly clearer optical images than the legacy (fibreoptic) SpyGlass system. Although the digital system is even easier to use due to the improved optical view and may actually achieve higher diagnostic rates in stricture evaluation, published outcome data from this system is more limited.(21)
The ease of use of SpyGlass cholangioscopy has resulted in its widespread utilisation in routine clinical practice. While excellent outcome data has been published from the pioneering referral centres, it is unclear whether similar excellent outcomes can be consistently replicated in routine clinical practice. This study examined the efficacy and safety of SpyGlass cholangiopancreatoscopy in the management of pancreaticobiliary disorders in a regional hospital in Singapore.
METHODS
This was a retrospective single-centre study conducted at Changi General Hospital, a regional hospital located in the eastern part of Singapore. This study was approved by the SingHealth Centralised Institutional Review Board.
Patients who underwent ERCP from January 2013 to November 2016 were identified from an electronic database and reviewed retrospectively. All patients who underwent SpyGlass cholangioscopy or pancreatoscopy (with or without further interventions such as targeted biopsies or laser lithotripsy) were enrolled in the study, and their clinical data was reviewed. Two groups of patients were excluded: those who underwent ERCP without the need for SpyGlass examination, and those who were initially scheduled for SpyGlass examination but did not undergo it, as the procedure was later judged to be unnecessary or technically not feasible due to anatomical abnormalities. Data such as patient demographics, procedure indication, type of SpyGlass system used, size of CBD stone, type and location of stricture, technical success, clinical success, and procedure-related complications was recorded and analysed.
ERCP with SpyGlass cholangioscopy or pancreatoscopy was performed on patients under sedation using a combination of intravenous midazolam and fentanyl administered by the endoscopist, except for one case that required anaesthetic support with intravenous propofol, as the patient could not be adequately sedated using midazolam and fentanyl. Prophylactic intravenous antibiotics were administered in all cases and continued post procedure, intravenously or orally, for at least three days. If postprocedure sepsis occurred, antibiotic treatment was extended. Selective cannulation was achieved using a papillotome and guidewire, and papillotomy was performed prior to insertion of the SpyScope™ catheter. In the context of difficult CBD stones that could not be extracted by conventional ERCP techniques such as papillotomy and mechanical lithotripsy, or balloon sphincteroplasty and extraction, stone fragmentation was achieved using Holmium-yttrium aluminium garnet laser lithotripsy. In cases of indeterminate strictures with mucosal abnormalities requiring targeted biopsies, at least six biopsies were routinely obtained using the SpyBite™ biopsy forceps.
Technical success was defined as successful insertion of the SpyGlass system to visualise the target and initiate interventions when required, such as performing targeted biopsies or initiating stone fragmentation using laser lithotripsy. A definitive diagnosis of a benign stricture was based on (a) the endoscopic appearance of a smooth surface and outline with no visible abnormal vessels; (b) benign histology if biopsies were taken and there was no progression on repeat imaging at 12-month follow-up; or (c) histology confirming its benign nature if surgery was performed. A definitive diagnosis of a malignant stricture was based on the endoscopic appearance of villous mucosal projections; irregular mucosal nodularity; mass-forming lesions; or prominent vascularisation/neo-angiogenesis and malignant histology from biopsies; surgical pathology; or, if histology was negative or unavailable, disease progression and mortality within a year of follow-up. Successful CBD stone clearance was defined as stone fragmentation and complete extraction of all stone fragments. Complications were defined using criteria previously described by Cotton et al.(22) Serum amylase or lipase was not measured routinely after ERCP in asymptomatic patients.
The primary outcome measures were clinically successful interventions such as complete clearance of CBD stones or extraction of a migrated stent, clinical utility for the diagnosis of an indeterminate stricture, and complication rates. Secondary outcome measures were the factors associated with clinical failure and differences in clinical outcomes between the legacy and digital SpyGlass systems. The differences in clinical outcomes were analysed using chi-square or Fisher’s exact test for categorical variables and Student’s t-test for continuous variables. The sensitivity, specificity, positive predictive value and negative predictive value for the diagnosis of an indeterminate stricture were evaluated. A p-value < 0.05 was considered as statistically significant. All statistical analysis was performed with IBM SPSS Statistics for Windows version 19.0 (IBM Corp, Armonk, NY, USA). All authors had access to study data and approved the final manuscript.
RESULTS
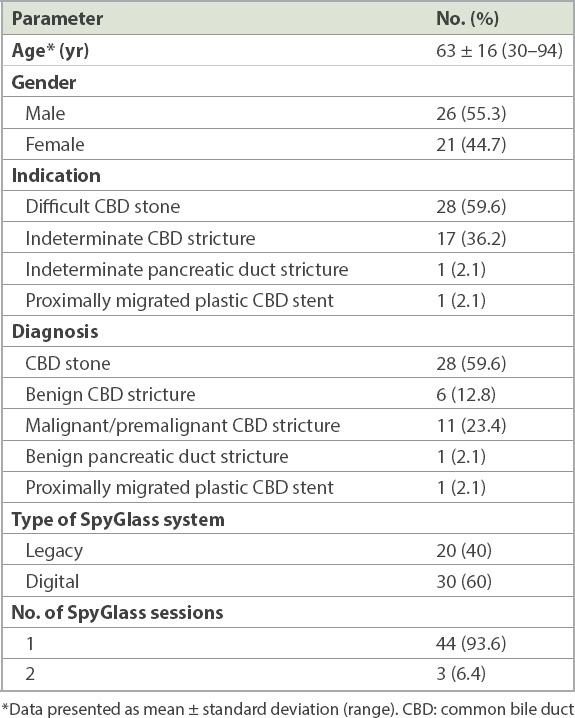
During the study period, a total of 2,050 ERCP procedures were performed. A total of 47 patients (mean age 63 ± 16 years [range 30–94 years], 55.3% male) underwent a total of 50 SpyGlass procedures, with 44 patients undergoing one procedure and three patients undergoing two procedures. The majority (49 out of 50) of the procedures were cholangioscopy and one was pancreatoscopy. The first 20 procedures were performed using the legacy SpyGlass system and the subsequent 30 using the digital SpyGlass system when it became available. Clinical indications were: difficult CBD stones (n = 28), indeterminate CBD stricture (n = 17), indeterminate pancreatic duct stricture (n = 1) and proximally migrated CBD stent (n = 1). SpyGlass cholangiopancreatoscopy was technically successful in all cases, achieving visualisation of the target. Patient demographics and clinical data are summarised in
Table I
Demographics and clinical data of patients who underwent SpyGlass cholangiopancreatography (n = 47).
Among the 28 patients with CBD stones (mean size 16 mm [range 10–35 mm]), successful initiation of stone fragmentation by laser lithotripsy was achieved in all cases and complete stone extraction (Figs.
Fig. 1
Initial cholangiogram shows large bile duct stones.

Fig. 2
Cholangioscopic image shows digital SpyGlass-directed laser lithotripsy of a bile duct stone.

Fig. 3
Final balloon cholangiogram shows no remnant bile duct stones.

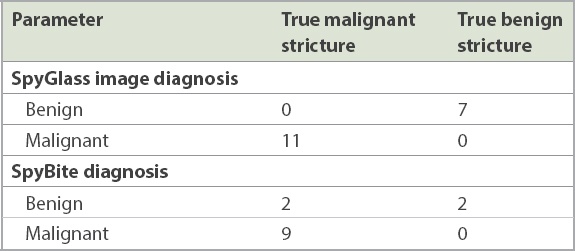
Among the 11 patients with biliary strictures, a correct diagnosis of malignancy based on visualisation (Figs.
Fig. 4
Cholangiogram shows proximal bile duct stricture and dilated intrahepatic ducts.

Fig. 5
Digital SpyGlass image shows cholangiocarcinoma.
Table II
Diagnostic yield of cholangiopancreatoscopy.
There was no difference in clinical outcome between legacy (n = 20) and digital SpyGlass™ cholangiopancreatoscopy (n = 30), with correct diagnosis of strictures being obtained in 5 (83.3%) out of six cases and 8 (88.9%) out of nine cases, respectively (p = 0.756), and complete stone extraction being achieved in 8 (88.9%) out of nine cases and 18 (94.7%) out of 19 cases, respectively (p = 0.575).
Postprocedure complications included 1 (2.1%) case of pancreatitis, 1 (2.1%) case of suspected sealed perforation after laser lithotripsy and 5 (10.6%) cases of cholangitis that were successfully treated with antibiotics. The patient with suspected sealed perforation recovered and was discharged well after conservative treatment. There was no procedure-related mortality.
DISCUSSION
The introduction of the SpyGlass system revolutionised the approach towards cholangioscopy and cholangioscopic interventions. As the SpyGlass system is much easier to use compared to other cholangioscopy systems, it is more frequently utilised in routine clinical practice. Even though the system was designed as a cholangioscopy system, it can also be inserted into a sufficiently dilated pancreatic duct for interventions such as lithotripsy or biopsy.(2,7,10,13,23) Our study was conducted in the setting of routine clinical care in a regional hospital, where SpyGlass-guided interventions were required in 2.4% of cases. Although the use of the newer digital SpyGlass system provided an improved optical view and thus made the procedure technically easier and faster, the eventual clinical outcomes of the legacy and digital systems were similar.
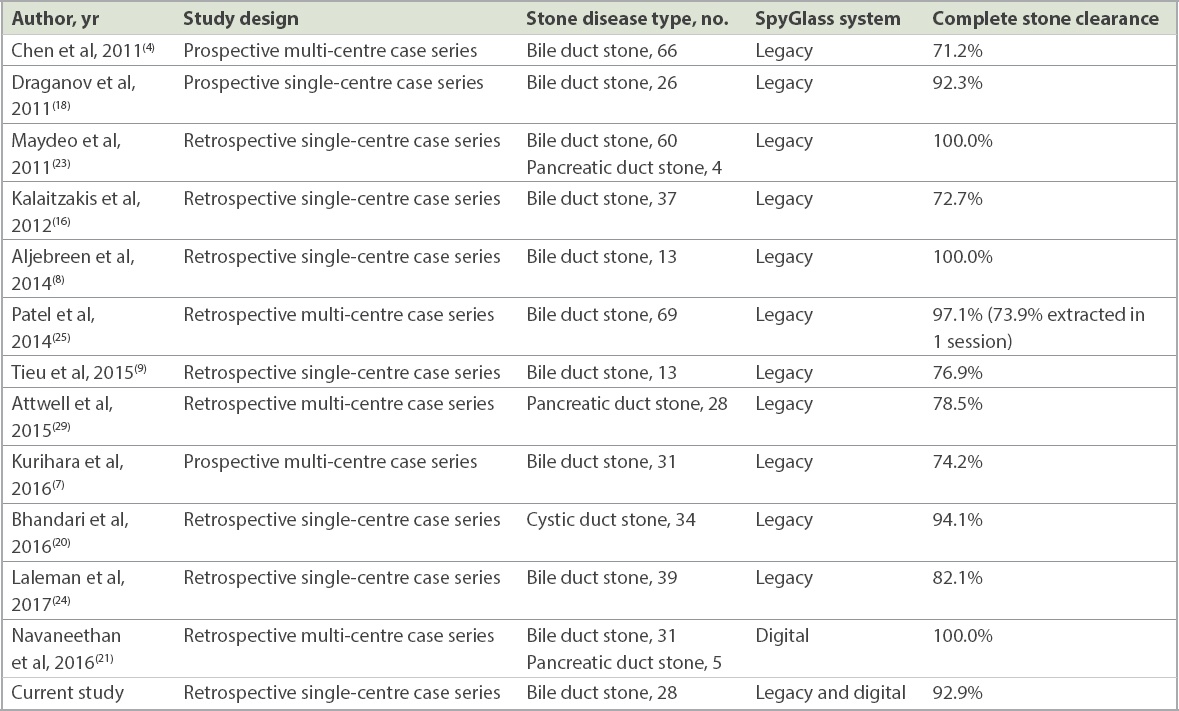
In the management of difficult CBD stones, complete stone clearance was achieved in 92.9% of our cases. Although some studies reported success rates of complete extraction that were somewhat lower at 71%–82.1%,(4,7,9,16,24) very high success rates of 94%–100% have also been reported.(8,18,23,25) The results of larger case series with at least ten cases are summarised in
Table III
Outcome of SpyGlass-guided electrohydraulic or laser lithotripsy in selected series of common bile duct stone disease with more than ten cases.
In our series, the sensitivity and specificity of SpyBite biopsies for indeterminate CBD stricture were 81.8% and 100.0%, respectively, while SpyGlass image-based diagnosis was correct in all cases. Hence, even though at least six biopsies were obtained in all cases in our study, there was still the problem of false negative biopsies. Nonetheless, these procedures still had higher sensitivity as compared to brush cytology and non-cholangioscopy-guided intraductal biopsies. In a recent meta-analysis, the pooled sensitivity and specificity of brush cytology for the diagnosis of malignant biliary strictures were 45% and 99%, respectively, while the pooled sensitivity and specificity for non-cholangioscopy-guided intraductal biopsies were 48.1% and 99.2%, respectively. A combination of both modalities only modestly increased the sensitivity to 59.4%.(26) In a systematic review that specifically examined the diagnostic performance of SpyGlass cholangioscopy with SpyBite biopsies, the pooled sensitivity and specificity of cholangioscopy-guided biopsies in the diagnosis of malignant biliary strictures were 60.1% and 98.0%, respectively. In four studies that included patients who had previous negative imaging and brushings and/or intraductal biopsies, the pooled sensitivity and specificity for diagnosis of malignant biliary strictures were 74.7% and 93.3%, respectively.(27) SpyBite biopsies had a significantly higher sensitivity (76.5%) than brush cytology (5.8%) and non-cholangioscopy-guided intraductal biopsies (29.4%) in a direct comparative study.(6) A recent study explored the utility of rapid onsite evaluation of touch imprint cytology (ROSE-TIC) in patients undergoing SpyGlass-directed biopsies. The overall sensitivity of ROSE-TIC for diagnosing malignancy was 100.0%, with a specificity of 88.9%, positive predictive value of 86.7%, negative predictive value of 100.0% and diagnostic accuracy of 93.5%.(28) This preliminary data suggested that ROSE-TIC could potentially further improve the diagnostic yield of cholangioscopy-guided biopsies.
The SpyGlass system has been successfully used for pancreatic duct interventions when the duct is sufficiently dilated to permit probe insertion. In the context of symptomatic pancreatic duct calculi, Maydeo et al successfully treated four cases using laser lithotripsy and achieved complete duct clearance;(23) a larger US multicentre series with 28 patients reported a treatment success rate of 79%.(29) Arnelo et al explored the use of SpyGlass pancreatoscopy in suspected intraductal papillary mucinous neoplasms (IPMN). Using pancreatoscopy, 76% out of 17 patients with a final diagnosis of main duct IPMN were correctly identified, while 78% out of nine patients with a final diagnosis of branch duct IPMN were correctly identified. Pancreatoscopy was found to have provided additional diagnostic information in the vast majority of the cases and to affect clinical decision-making in 76% of them.(10)
There is a reasonable concern that cholangioscopic or pancreatoscopic interventions may result in a higher complication rate compared to standard ERCP. Reports from studies that examined the role of cholangioscopy in indeterminate biliary strictures and difficult bile duct stones suggest that its complication rates, from complications such as pancreatitis and perforation, are similar to those of routine ERCP. In the case of pancreatic duct interventions, Arnelo et al reported that the incidence of post-ERCP pancreatitis was 17% in their cohort of patients who underwent pancreatoscopy to evaluate suspected IPMN.(10) In the US multicentre series that evaluated laser lithotripsy for pancreatic duct stones, 8 (29%) out of 28 patients had mild adverse effects, comprising 1 (4%) patient with mild post-ERCP pancreatitis and 7 (25%) patients with a transient increase in abdominal pain.(29) As vigorous irrigation is required to obtain a clear view and remove debris during lithotripsy, there is the concern of increased risk of cholangitis, such that prophylactic antibiotics are routinely used during cholangioscopy. One study prospectively evaluated the risk of bacteraemia and infectious complications in 72 patients undergoing SpyGlass cholangioscopy.(30) Blood cultures were obtained immediately before ERCP, after completion of the ERCP portion of the procedure (to determine ERCP-related bacteraemia), and 15 minutes after completion of cholangioscopy. True positive blood cultures were noted in 20 (27.8%) patients, of whom 6 (8.3%) patients had transient bacteraemia following ERCP. Of 14 (19.4%) patients with sustained bacteraemia following ERCP or cholangioscopy, 10 (13.9%) had sustained bacteraemia related to cholangioscopy. Despite the administration of postprocedure intravenous antibiotic, 7 (9.7%) patients required further antibiotic treatment for infectious complications, 3 (4.2%) of whom were hospitalised in order to receive intravenous antibiotic therapy. The authors concluded that the bacteraemia linked to ERCP with cholangioscopy and the subsequent risk of hospitalisation for infectious complications suggested that preprocedure antibiotic prophylaxis should be considered for patients undergoing cholangioscopy. In our study, cholangitis was the most common (10.6%) complication despite the use of prophylactic antibiotics. A multicentre retrospective study of 282 SpyGlass cholangiopancreatoscopy procedures reported mild post-ERCP pancreatitis in 3.9%, post-ERCP cholangitis in 1.4%, bleeding in 1.1% and perforation in 0.7% of patients. This data was similar to that seen in large studies of ERCP performed without cholangiopancreatoscopy.(31)
The digital SpyGlass system is now available and early non-comparative data is being published.(21) The setup is simpler and the image resolution better compared to the legacy system, making it easier and faster to visualise the target lesion. The insertion of the SpyBite forceps is also easier. The digital system further simplifies the cholangioscopy procedure and may potentially improve the diagnostic yield in stricture evaluation. Although treatment success rates for CBD stones are already very high with the legacy system, and hence the additional therapeutic advantage may be less, the digital system makes the process easier. In addition to the management of difficult CBD stones and indeterminate strictures, for which its utility has been established, the legacy SpyGlass system has also been successfully used in a myriad of other indications, such as to direct guidewire placement to navigate and traverse tight strictures or access the cystic duct, and to extract migrated stents; this will probably be even easier with the new digital system.(32-36)
Given the costs of the SpyGlass system, it is important to clarify how to utilise it in a cost-effective manner. It is important to decide a priori when the SpyGlass system should be used at the index ERCP, because its use can save the cost of an additional ERCP. In the case of CBD stones, the use of the SpyGlass system is clearly indicated in specific situations where the stone is too big to be captured by the mechanical lithotripsy basket or extracted by large balloon sphincteroplasty. In the context of indeterminate CBD strictures, a recent study compared the cost-effectiveness of five ERCP-based techniques for diagnosing cholangiocarcinoma in patients with primary sclerosing cholangitis-induced biliary strictures, using a Monte Carlo simulation to assess outcomes. It concluded that compared to ERCP with brush cytology; ERCP with brushing cytology and fluorescence in situ hybridisation (FISH)-trisomy; ERCP with brush cytology and FISH-polysomy; and ERCP with intraductal biopsy sampling, SpyGlass cholangioscopy with targeted biopsy was the most cost-effective diagnostic modality.(37)
We acknowledge the limitations of our study. This was a single-centre retrospective study with a limited study population. Data on procedure time and length of stay was obtained retrospectively and may not accurately reflect the time attributed to the procedure. Therefore, we did not report this data but focused on more robust outcome data such as treatment success and complication rates. In addition, most of the procedures were performed by a single endoscopist (Ang TL). Nonetheless, this data is still important, because local data has not been published and our results are consistent with the outcomes from high-volume referral centres around the world.(8,18,21,23,25,27)
In conclusion, our study demonstrated that SpyGlass cholangiopancreatoscopy was a safe and effective tool in routine clinical practice. It was effective in the treatment of difficult CBD stones and the evaluation of indeterminate pancreaticobiliary strictures.


