Abstract
INTRODUCTION
Chest physiotherapy (CPT) may benefit children aged below five years who suffer from lower respiratory tract infection (LRTI). However, its effects depend on the technique used. This study aimed to determine whether mechanical CPT using the LEGA-Kid® mechanical percussion device is superior to manual CPT in children with LRTI.
METHODS
Children aged five months to five years who were admitted and referred for CPT from January to April 2017 were randomised to either manual CPT or mechanical CPT with LEGA-Kid. Outcomes measured before intervention and two hours after intervention were respiratory rate (RR), oxygen saturation and modified Respiratory Distress Assessment Instrument (mRDAI) score.
RESULTS
All 30 enrolled patients showed significant reduction in post-intervention RR and mRDAI scores. There was an 8% reduction in RR for the manual CPT group (p = 0.002) and a 16.5% reduction in the mechanical CPT group (p = 0.0001), with a significantly greater reduction in the latter (p = 0.024). mRDAI scores decreased by 2.96 in the manual group (p = 0.0001) and 3.62 in the mechanical group (p = 0.002), with no significant difference between the groups. There was no significant improvement in oxygen saturation, and no adverse events were observed after CPT.
CONCLUSION
Children receiving both manual and mechanical CPT showed improvements in respiratory distress symptoms, with no adverse effects. A combined strategy of nebulised hypertonic saline followed by CPT for LRTI removes airway secretions and results in improvements in moderately severe respiratory distress. The LEGA-Kid mechanical CPT method is superior to manual CPT in reducing the RR.
INTRODUCTION
Lower respiratory tract infections (LRTIs) are common in children aged below five years and are a leading cause of hospital admissions. LRTIs are associated with increased morbidity and mortality.(1) Most infections are viral in origin and associated with copious thick secretions. As a result, the airway becomes obstructed, resulting in severe respiratory distress and ventilation-perfusion mismatch.(2) The presence of airway oedema also increases airway resistance, thereby worsening hypoxia. The consequences of mechanical obstruction include reduced tidal volume, increased work of breathing and retained secretions, which further exacerbate respiratory distress.
Chest physiotherapy (CPT) assists in mucociliary clearance, which reduces airway resistance and improves ventilation.(3) Newer CPT methods, such as forced exhalation with an open glottis(4) and slow-flow techniques,(5,6) have shown short-term benefits to respiratory symptoms from bronchial obstruction, without impact on duration of hospitalisation. In patients who are hospitalised with acute bronchiolitis, conventional CPT and expiratory acceleration flow techniques have shown short-term improvements in respiratory distress scores and positive parental satisfaction.(7) Conventional CPT and prolonged slow expiration techniques were effective in reducing clinical scores 48 hours after intervention when compared to only upper airway suctioning in patients with respiratory syncytial virus bronchiolitis of moderate severity.(8) However, its use has been limited because CPT requires an experienced therapist to perform.
A Cochrane analysis of 12 randomised controlled trials in 2016 compared physiotherapy with no intervention in patients with mild, moderate and severe acute bronchiolitis.(9) Physiotherapy techniques included conventional percussion with vibration plus postural drainage and passive flow-orientated expiratory techniques. Both techniques failed to improve severity status and time to recovery. However, one trial observed a small improvement in the Wang clinical score immediately after the intervention in patients with moderately severe acute bronchiolitis.(8) The authors of the review concluded that these physiotherapy techniques could not be used as standard clinical practice for hospitalised patients with severe bronchiolitis, and instead recommended exploring the combination of CPT with salbutamol or hypertonic saline in patients with mild to moderate acute bronchiolitis.(9)
Effective CPT techniques require skilled personnel and may be difficult to perform in young children. LEGA, a mechanical device designed by Formedic Technology Sdn Bhd, Malaysia, has been used as an aid for CPT. This machine is a handheld, battery-operated percussor that provides clapping to the chest wall to mimic manual hand percussion. A randomised controlled cross-over study evaluating the efficacy and safety of LEGA compared to conventional CPT in adults with chronic obstructive pulmonary disease showed the device to be effective in generating cough and expectoration of sputum. The device was well tolerated and patients were able to use it independent of a chest physiotherapist.(10)
A similar but smaller device (LEGA-Kid®) has been designed by Formedic Technologies for use in children weighing 5–15 kg. It produces rotational movements with a predetermined frequency that creates percussion and vibration forces when in contact with the chest wall. The generated force travels through the chest wall and helps to loosen secretions. We hypothesised that LEGA-Kid would be as effective as manual CPT for mucus clearance, thereby reducing respiratory distress without causing significant patient distress. This study sought to compare the safety, tolerability and efficacy of LEGA-Kid with that of manual CPT in children with LRTI.
METHODS
This single-blind, randomised controlled study was conducted in the paediatric wards of University Malaya Medical Centre (UMMC). Eligible children were randomly allocated to manual (control group) or mechanical CPT (study group) after informed consent was obtained. Approval from the UMMC Medical Ethics Committee was obtained prior to the start of the study (ID no. 20166-2502). The study was registered with the National Medical Research Registry (NMRR) of Malaysia (NMRR-16-2803-32022).
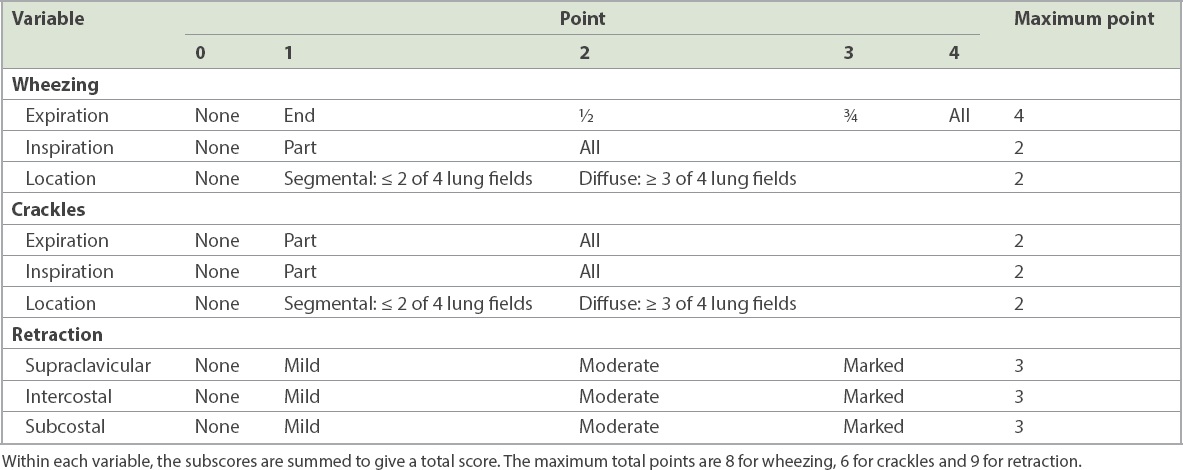
Children aged five months to five years, weighing between 5 kg and 15 kg, who were admitted with symptoms of LRTI and referred for CPT by the managing doctors were included into the study. Children were excluded if they had severe respiratory distress or heart failure, bone disease, thrombocytopenia or a modified Respiratory Distress Assessment Instrument (mRDAI) score ≤ 6 (
Table I
Modified Respiratory Distress Assessment Instrument scale: wheezing, crackles and retractions.
Patients were randomised to either manual or mechanical CPT using an online software, Research Randomizer 4.0,(11) in a ratio of 1:1, using permuted blocks of 4. The number ‘1’ was assigned to the first eligible participant, the number ‘2’ to the second, and so on till number ‘30’. This was a single-blinded study, where the intervention arm was known to the participants and the physiotherapist, but not to the physician performing the pre- and post-intervention evaluations.
Nebulised 3% hypertonic saline (4 mL over 15 minutes) was administered to all patients before the physiotherapy session. CPT, together with postural drainage, was performed by an experienced paediatric chest physiotherapist. The following steps were incorporated: (a) an assessment of the patient’s condition, vital signs and auscultation to identify the involved lung segment; (b) placement of the patient according to the postural drainage positions; (c) chest percussion and vibration manually or with LEGA-Kid device on the chest area; (d) removal or expectoration of mucus by gentle oral/nasal suction and provoked cough; and (e) technique with localised breathing to enhance expansion of the specific lung segment.
Mechanical CPT involved application of the percussor firmly and at right angles to the chest wall to make the voice quiver. The selected frequency was indicated by the numbers 1 to 10; the lower numbers signified percussions and higher numbers signified vibrations. Each physiotherapy session lasted for 15–20 minutes, during which the patients were shown their favourite videos and toys. Post CPT, positioning was performed to improve chest expansion. Oxygen therapy was continued as at T0, pre-intervention. Bronchodilator therapy was avoided during the intervention period, which was about three hours.
All patients underwent a baseline evaluation at enrolment, and pre-intervention (T0) and two-hour post-intervention (T120) evaluations by a trained physician who was blinded to the method of CPT. The primary outcome measures evaluated were temperature, heart rate, RR, pulse oximetry with a Nellcor oximeter after being in room air for five minutes and modified Respiratory Distress Assessment Instrument (mRDAI). The mRDAI is a modification of the RDAI, which rates wheezing and respiratory distress on a scale of 0 to 17. The addition of assessment of crackles gives a total score of 23 (
During the intervention, a research assistant monitored the heart rate and oxygen saturation and also looked out for any adverse events such as bradycardia, desaturation and vomiting. The secondary outcome measures were length of hospital stay and FLACC (Face, Legs, Activity, Cry, Consolability) scale to assess the level of distress(15) at T0, during intervention (TCPT) and at T120. The FLACC scale evaluates pain and discomfort in the paediatric age group. It has a score of 0 to 10, where 0 indicates relaxed and comfortable, 1–3 indicates mild distress, 4–6 indicates moderate pain and 7–10 indicates severe distress.
CPT was carried out daily until the mRDAI score was ≤ 6 or until discharge from hospital. Typical care involving the type of respiratory support and oxygen supplementation was determined by the ward clinicians, who were blinded to the method of CPT. Oxygen therapy was delivered via nasal cannula or high flow nasal cannula. Target oxygen saturation was 95%, while the choice of oxygen delivery was tailored to the patient’s RR and the presence of retractions.
Data was entered using IBM SPSS Statistics version 23.0 (IBM Corp, Armonk, NY, USA). To reach the statistical effect of 80% power and 5% significance, a sample size of 30 was required – 15 in the manual CPT arm and 15 in the mechanical arm (LEGA-Kid). Non-parametric data was analysed using the Mann-Whitney U test, and parametric data was analysed using paired and Student’s t-tests. Paired t-test was used to compare pre- and post-intervention observations in each group, while Student’s t-test was used to compare the difference between the groups. Chi-square test was used for nominal data. One-way analysis of variance for repeated measures was used to compare the daily evolution of the Wang scores. A p-value < 0.05 was considered statistically significant.
RESULTS
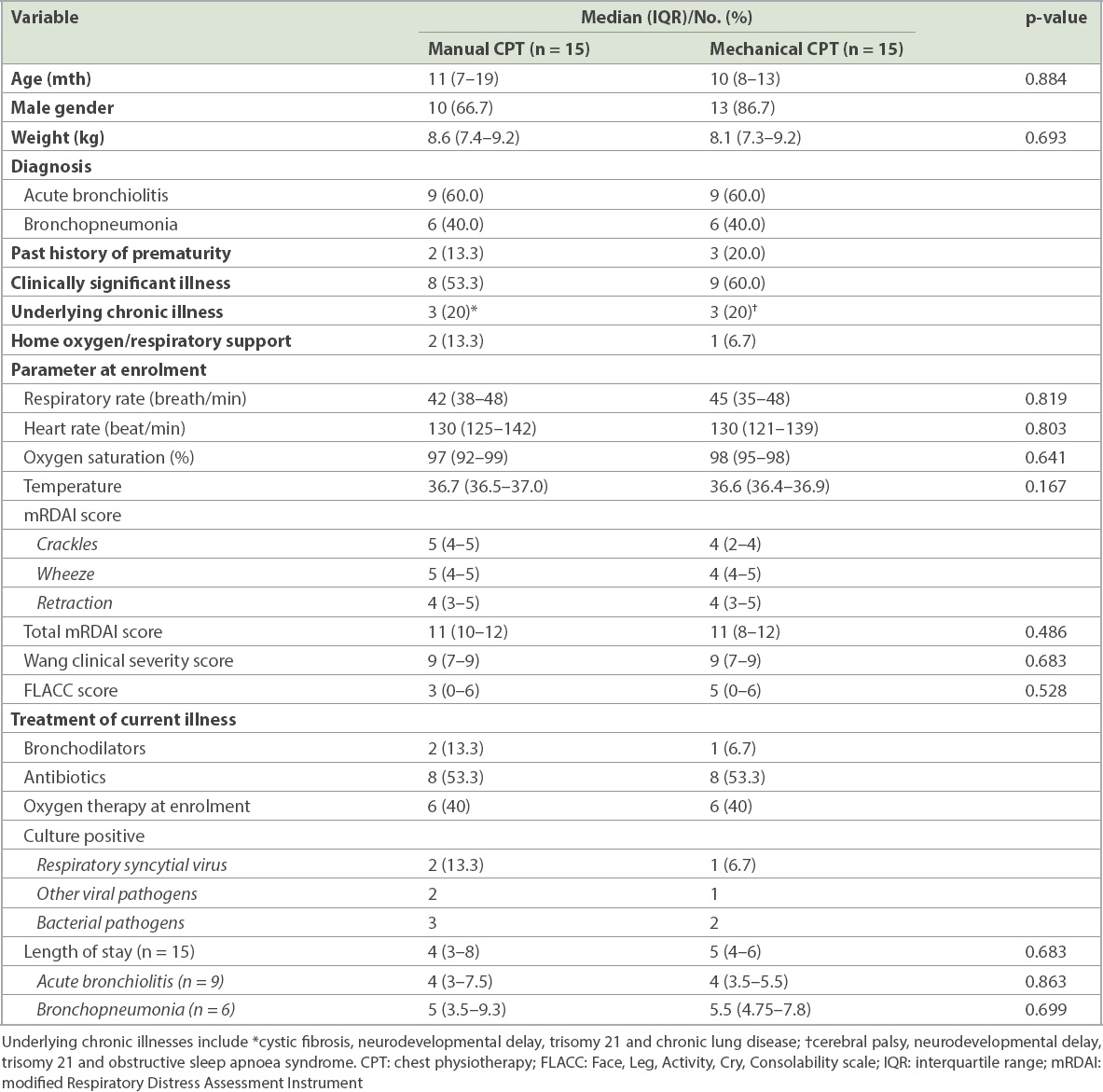
A total of 30 patients were enrolled and randomised to receive either manual or mechanical CPT between 9 January 2017 and 30 April 2017. The patients completed 45 sessions in the manual group and 42 sessions in the mechanical group for a total of 87 physiotherapy sessions. The demographic data and baseline clinical characteristics of the patients are shown in
Table II
Demographic data and parameters at enrolment.
Patients in both the manual and mechanical groups showed significant reductions in RR and mRDAI score at T120 compared to T0 (
Table III
Changes in clinical characteristics of patients before (T0) and after intervention (T120).
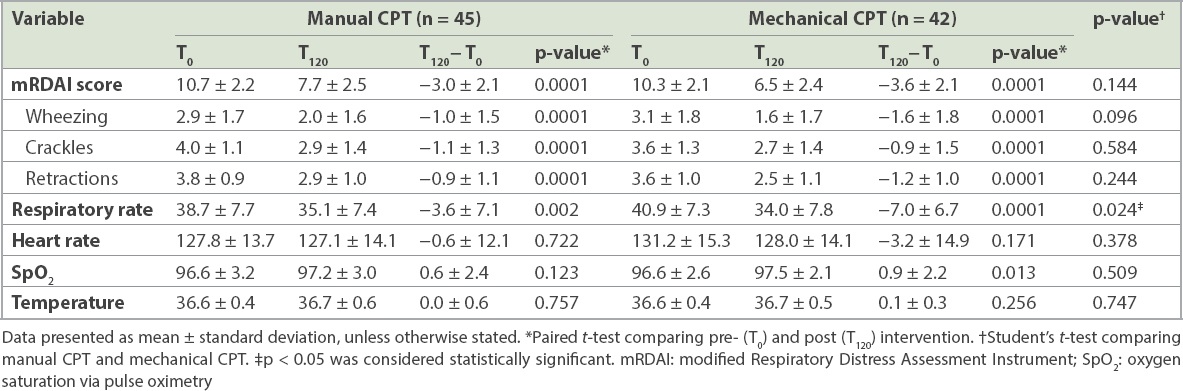
Similarly, there was a significant decrease in mRDAI scores between T0 and T120: 2.96 points (27.2% reduction, p = 0.0001) in the manual group and 3.62 points (34.5% reduction, p = 0.0001) in the mechanical group. Similar improvements were observed in all three components of the mRDAI score at T120 compared to T0. However, the reduction in mRDAI scores in the mechanical and manual groups was not significant (p = 0.144). Children in the mechanical group showed significant improvement in oxygen saturation at T120 (p = 0.013) compared to the manual group (p = 0.123). However, the improvement in oxygen saturation in the mechanical and manual groups was not significant (p = 0509).
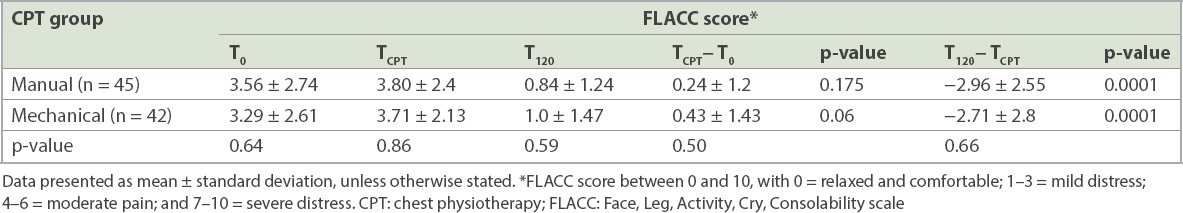
Table IV
FLACC score before (T0), during (TCPT) and after (T120) intervention.
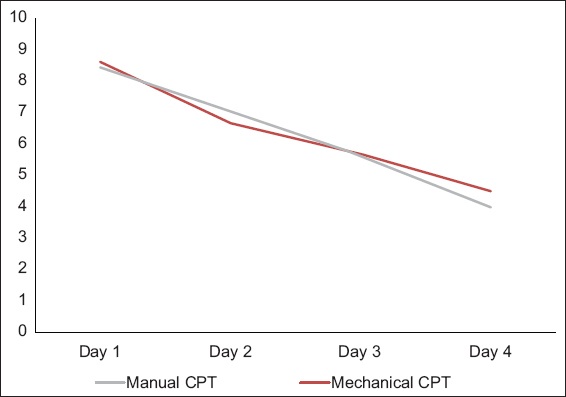
The daily mean Wang scores decreased significantly day by day from enrolment till Day 4 in both groups, from 8.4 to 4 (p < 0.001) in the manual group and from 8.6 to 4.5 (p < 0.001) in the mechanical group (
Fig. 1
Graph shows daily pre-intervention (T0) Wang clinical severity scores.
DISCUSSION
In this study, we observed significant improvements in RR, oxygen saturation and mRDAI in patients who underwent either manual or mechanical CPT. Children using mechanical CPT had greater reduction in their RR and more improvement in oxygen saturation after intervention. No side effects were noted, and improvements in the FLACC score were observed after both interventions.
The baseline demographics in both groups were comparable for age, weight and severity of respiratory distress. While there was a male preponderance in the mechanical group, this is unlikely to have influenced the results. The median mRDAI score of 11 at enrolment indicated moderately severe respiratory distress and a need for CPT. The efficacy of the LEGA-Kid machine was comparable to that of manual CPT performed by an experienced chest physiotherapist. The main drawbacks to performing effective manual CPT include the need for trained personnel, variability in techniques and skills among personnel, time constraints and familial burden. The combination of percussion and vibrations provided by the LEGA-Kid machine could mimic manual CPT, which helps to dislodge loosened secretions. Maximal intrathoracic pressure was achieved when the percussor was pressed firmly and at right angles to the chest wall to make the voice quiver. The percussor was shown to maintain a higher and more constant intrathoracic pressure, comparable to the performance of three physiotherapists.(16)
Our results differ from those of previous studies that compared CPT versus no CPT in children less than two years of age with severe bronchiolitis; no significant improvement in clinical severity was reported in children who received CPT compared to those who did not.(17-19) These studies, however, did not incorporate prior nebulisation with hypertonic saline. Of the 12 randomised controlled trials reviewed in the 2016 Cochrane review,(9) only one study(8) included the use of nebulised 3% saline with albuterol with or without CPT in patients with moderately severe respiratory syncytial virus bronchiolitis. An immediate reduction in wheezing and retractions was observed in patients who received CPT, with no impact on duration of hospitalisation.(8)
Despite the heterogeneity of the patients in our study, all of them retained airway secretions, which contributed to their respiratory distress. Nebulised hypertonic saline induces an osmotic flow of water in the inspissated mucous, thus reducing the viscosity of the mucous and oedema in the submucosal tissue.(20) Subsequent CPT assists in the clearance of the loosened secretions, resulting in improved tidal volume, a more effective cough and further removal of secretions, which immediately helps to make breathing easier for the young child. This sequence of events explains the improvement in RR and better scores for the three components of mRDAI at T120 as compared to those at T0. Our combined strategy of nebulised hypertonic saline followed by CPT differs from that of studies that investigated the efficacy of nebulised hypertonic saline alone in the management of LRTI.(21-23)
Both the manual and mechanical CPT procedures used in our study were well tolerated by the patients, as measured by the FLACC scale. Our patients’ acceptance of CPT could be partially explained by the distraction methods used. The FLACC score was further reduced at T120, indicating an improvement in overall condition after intervention. No adverse events were reported. The median length of stay in patients with acute bronchiolitis and bronchopneumonia was similar to those reported in the literature.(17,24)
The strengths of our study lie in the standardisation of CPT methods with the use of one trained physiotherapist to perform both the mechanical and manual CPT, and two physicians throughout the study – one to evaluate safety and tolerability, and the other to assess the efficacy of CPT. Furthermore, the latter physician was blinded to the method of CPT. However, our study was not without its limitations. First, it was limited by the lack of a control group with no CPT, which may have affected the interpretation of our results. We were unable to have a control group, as our hospital’s policy requires children with LRTI who are aged below two years to be managed with regular CPT when needed. Second, we did not conduct subsequent evaluations beyond two hours to determine whether the improvements observed were sustained; nonetheless, no child in the study deteriorated during or after CPT. Third, our study also did not set out to investigate the ease of the percussor versus conventional physiotherapy. Finally, our sample size was small but sufficient for a pilot study.
In summary, as an adjunct treatment for LRTI, CPT is safe and beneficial for mucociliary clearance and improves moderately severe respiratory distress. The LEGA-Kid percussor is better than manual CPT performed by experienced personnel. However, further studies are needed to confirm these preliminary results.
ACKNOWLEDGEMENTS
We thank the following individuals for their contribution to the study: A/Prof Thavagnanam Surendran, A/Prof de Bruyne Jessie Anne, A/Prof Gan Chin Seng, Dr Chuah Soo Lin and Dr Abdul Aziz Fadzlina; the medical and nursing staff of Paediatric Respiratory Ward, Department of Paediatrics; and Manjit Singh Anmol Kaur and Haron Norazah, Physiotherapy Division, Department of Rehabilitation Medicine, UMMC, Kuala Lumpur, Malaysia. The study was funded by PlaTCOM Ventures Sdn Bhd via a grant to Formedic Technology (grant PlaTCOM-HIP-2015/013). Neither PlaTCOM Ventures Sdn Bhd nor Formedic Technology had any role in the study design, data collection and analysis, manuscript preparation or the decision to publish the manuscript.


