INTRODUCTION
In 2050, a total of 4,758 million people worldwide (49.8% of the world’s population) are expected to be myopic, and 938 million people (9.8%) are expected to suffer from high myopia (myopia worse than −5.00 D).(1) Myopia, commonly known as short-sightedness or near-sightedness, has remained one of the biggest public health challenges in Singapore, which has very high myopia rates. Myopia typically begins in early childhood and progresses during childhood.
Based on unpublished data from routine vision screening done by the School Health Service (SHS) using the Snellen chart, the prevalence of defective vision amounting to unaided visual acuity of 6/12 or worse among Primary 1 students was 33% in the year 2000, prior to the inception of the National Myopia Prevention Programme (NMPP). 65% of Singapore students suffered from myopia by the age of 12 years. Among these 12-year-old students, the prevalence of severe defective vision (i.e. unaided visual acuity worse than 6/60) was 13% (unpublished data).
Age of onset of myopia and duration of myopia progression are the most important predictors of high myopia in later childhood.(2) Children with high myopia in the range of ≤ −5.0 D to −10.0 D(3) have higher risks of complications, such as myopic macular degeneration,(4-6) retinal detachment,(7) glaucoma(8) and blindness.(9) There was concern that if such trends continued, more than 80% of the population would be suffering from myopia by adulthood, and among them, a high proportion would have high myopia.(10-13) Given that Singapore has an ageing population, this would increase the burden on the healthcare system because of the greater need to provide treatment for myopia-related complications. As about 80% of male enlistees are myopic at the time of enlistment for National Service in Singapore, adjustments have to be made to accommodate the occupational demands of military duties, incurring additional costs.(11,14) The pool of candidates for National Service duties and military occupations that require good vision, such as pilots, would also be more limited.(11,14)
NATIONAL MYOPIA PREVENTION PROGRAMME
To address the primary concern of high childhood myopia rates and the downstream public health concerns, the NMPP Steering Committee was formed in 2001. This committee comprised representatives from the Ministry of Education, Singapore Armed Forces, Ministry of Social and Family Development, National University of Singapore, Singapore Eye Research Institute, Optometrists and Opticians Board, Ministry of Health, and Singapore optometric and professional groups.(13) To implement the scaled-up initiatives of the NMPP, the SHS employed a two-pronged approach to delay the onset and progression of myopia, consisting of public education to raise awareness and vision screening for early detection and management of myopia.
Public education
The following public education strategies were adopted: (a) targeted vision care education for children (kindergartens and primary schools) and youths (secondary schools), and for key stakeholders (parents and teachers) to facilitate an environment that promotes good eye care habits; and (b) the use of mass media to propagate the message of good eye care habits among the general public.
For years, vision care education in children and youth focused on reducing the duration of time spent on near work such as reading, writing and use of electronic devices. However, findings from the Singapore Cohort Study of the Risk Factors for Myopia revealed that outdoor activity could be protective against the development of myopia in children.(15) This was further supported by findings from the Sydney Myopia Study presented at the 2006 International Myopia Conference, which found that the only significant difference between myopic seven-year-old Singapore Chinese children and those of Chinese ethnicity in Sydney was the amount of time spent outdoors.(16) Children in Sydney spent about four times as much time outdoors than Singapore children and less or hardly any time on tuition.(16)
Hence, outdoor activities became a key strategy in messages on good eye care habits to delay the onset of and prevent myopia among children, besides the continued efforts on reducing screen time. The promotion of outdoor activities has the secondary benefit of promoting overall health and wellbeing. Various age-appropriate fun activities were developed and conducted for children to help convey these vision care messages: dramas, jingles, dance, and a mobile ‘health lifestyle’ bus. The NMPP even had a mascot called ‘Captain Eye’ whose function was to trigger recall of good eye care messages. Since that time, other studies have been published showing that additional time spent outdoors was associated with a reduced incidence of myopia among certain age groups.(17)
To educate teachers and parents, who play a critical role in creating a supportive environment for good eye care habits in school and at home, several programmes were introduced. In the early years of this initiative, training programmes that provided a more in-depth understanding of myopia were conducted for teachers. Subsequently, activities and resources were customised for children of different age groups, including activity cards for primary school students that could be used as a teaching aid. Teachers were also encouraged to motivate students to come up with their own creative ideas and activities to promote good eye care habits among their peers, which would earn them points towards getting a ‘Captain Eye’ badge for themselves. Teachers could thus save time in creating new activities, while students were empowered to take the lead in taking care of themselves.
To reach parents and families, school-based group counselling sessions were held. Seminars aimed to promote good eye care habits at home were organised for parents with preschoolers and primary school-going children through a school-cluster approach to reach as many parents as possible. In Singapore, schools within the same vicinity (usually about ten schools) are grouped as a cluster to facilitate sharing of information and programmes, and for support under the Ministry of Education. Public forums were also organised regularly to help parents and families understand myopia, including the risks of complications, and to provide tips on how to inculcate good eye care habits in their children.
The message was widely promoted to the general public through the mass media, including television commercials, the radio and popular parents’ magazines. Information on childhood myopia was also readily available on the website of the Health Promotion Board, Singapore.
Vision screening
Routine vision screening is a key strategy in early myopia detection and intervention. Long before the inception of the NMPP, vision screening was already part of SHS’ school-based services(18) for all primary and secondary students. In the 1950s, primary school entrants were practically free from defective vision.(19) However, in the post-independence years (i.e. after 1965), an increase was seen in the number of children with defective vision. In 1988, 16% of Primary 1 and 50% of Primary 6 children had visual acuity of 6/12 or worse.(20) By 1996, 24.5% of Primary 1 and 60.4% of Primary 6 children had visual acuity of 6/12 or worse.(20)
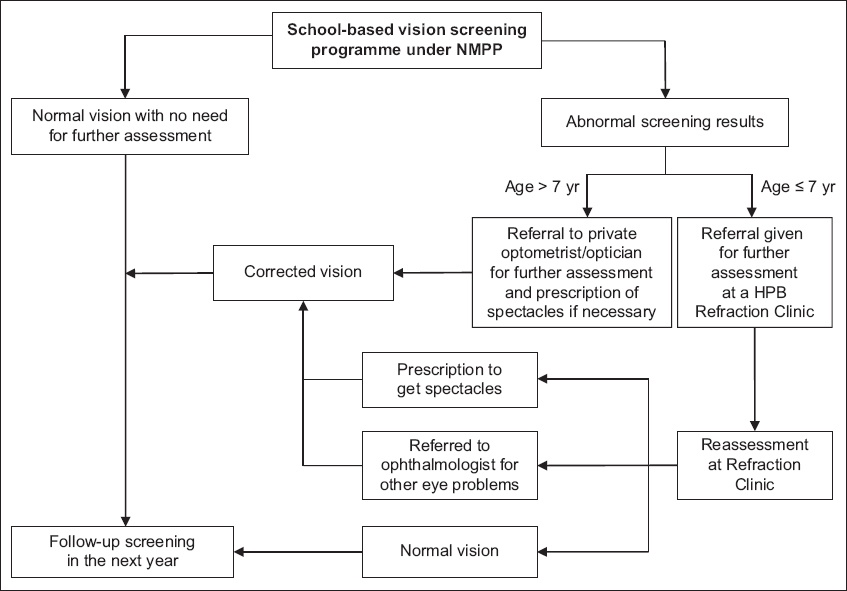
Since that time, vision screening has continued to be conducted annually in all schools. Following the inception of the NMPP, between 2002 and 2003, the scope for vision screening of the SHS was further expanded to include about 80,000 preschool children as young as five years of age. Preschool students and Primary 1 students who were found to have defective vision on routine screening were referred to Refraction Clinics (RCs) at the Student Health Centre, Health Promotion Board, for further assessment. Cycloplegic refraction was also made available for students who required it, for more effective assessment of their vision at the RCs. Following assessment, children who required glasses were given a prescription to purchase spectacles at optical shops in the community. Children detected or suspected to have severe myopia, amblyopia or other eye conditions such as squint and ptosis were referred to paediatric ophthalmologists at one of the public hospitals or to an ophthalmologist in private practice, as chosen by the parents (
Fig. 1
Flowchart shows the selection process for vision screening services for schoolchildren. HPB: Health Promotion Board, Singapore; NMPP: National Myopia Prevention Programme
REVIEW OF NMPP-LED SCHOOL-BASED VISION SCREENING (2004–2015)
To understand how the programme was doing in its goal of reducing childhood myopia rates, myopia prevalence rates were determined for the years 2004 to 2015 for 12 sentinel primary schools and 12 sentinel secondary schools, in which lensometer readings from spectacles were taken during routine school-based vision screening. Lensometer readings were used as a surrogate for myopia, which was defined as a spherical equivalent greater than 0.5 dioptres. Children who were wearing contact lenses in either eye were also included in the analysis. To ensure adequate representation of students across the country, 12 primary and 12 secondary schools were selected according to the school zone to which they belonged (north, south, east or west) and school type (co-ed or single-gender school). De-identified data from approximately 20,000 primary school and 15,000 secondary school students each year between 2004 and 2015 were included in this analysis. Statistical significance of trends was examined by fitting a linear regression line to the natural logarithm of the myopia prevalence, with year as the variable. A p-value < 0.05 was considered statistically significant. Confidence intervals (CIs) were reported for annual percentage change (APC) where relevant. APC was calculated as the exponential of (coefficient − 1) × 100%. Statistical analysis was performed using Stata 13.1 software (StataCorp, College Station, TX, USA).
The prevalence of myopia among students from the 12 sentinel primary schools decreased from 37.7% to 31.6% between 2004 and 2015 (p < 0.05; 95% CI −1.7%, −0.6%) (
Fig. 2
Chart shows the prevalence rate of myopia among primary and secondary school students. APC: annual percentage change; CI: confidence interval
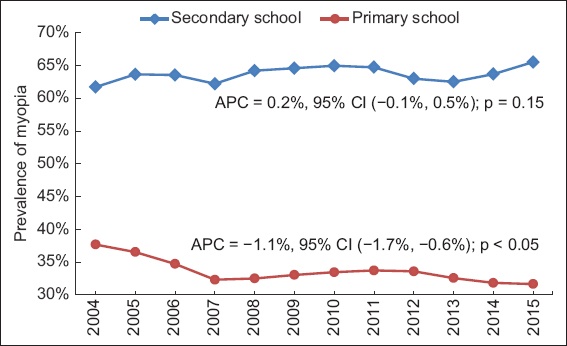
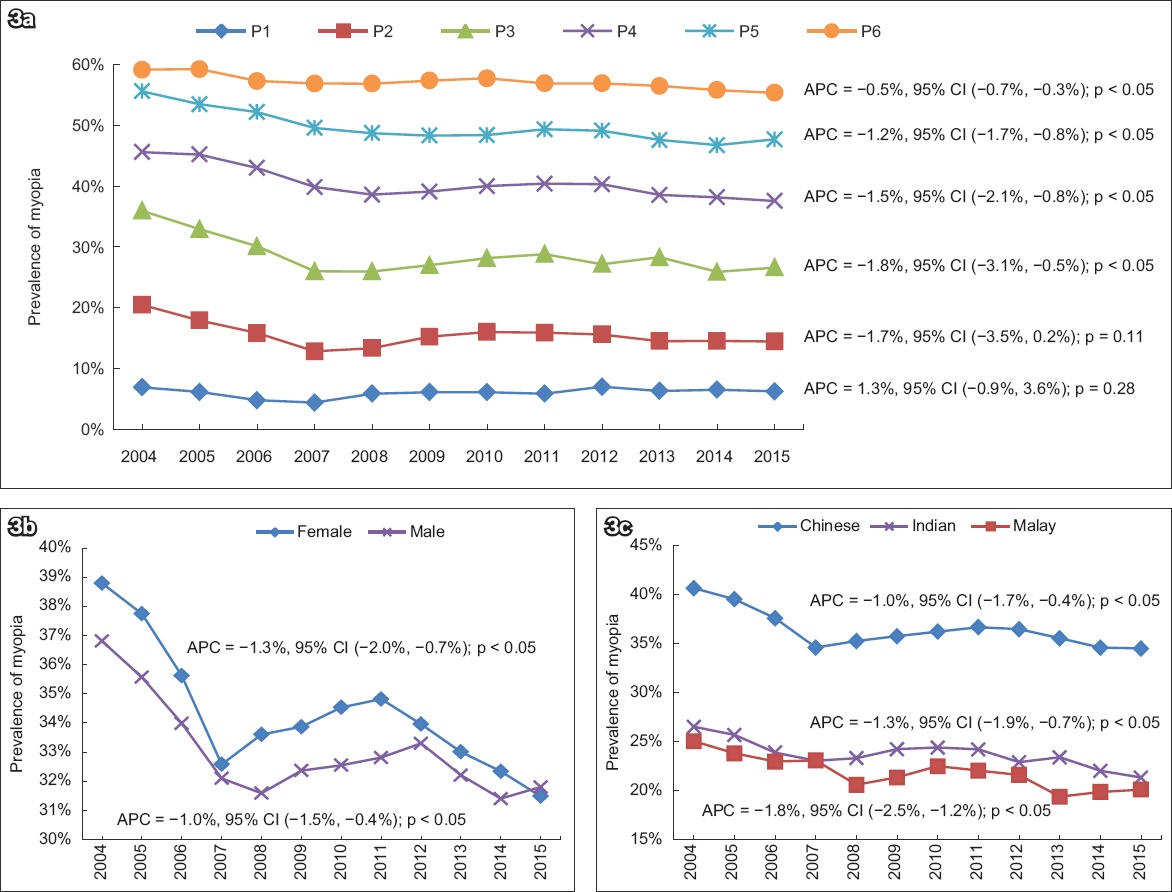
Fig. 3
Charts show the prevalence rate of myopia among primary school students by (a) educational level; (b) gender; and (c) ethnicity. APC: annual percentage change; CI: confidence interval; P: primary
The increase in myopia prevalence from 61.7% to 65.5% among students from the 12 sentinel secondary schools was not statistically significant (p = 0.15; APC 0.2%, 95% CI −0.1%, 0.5%) (
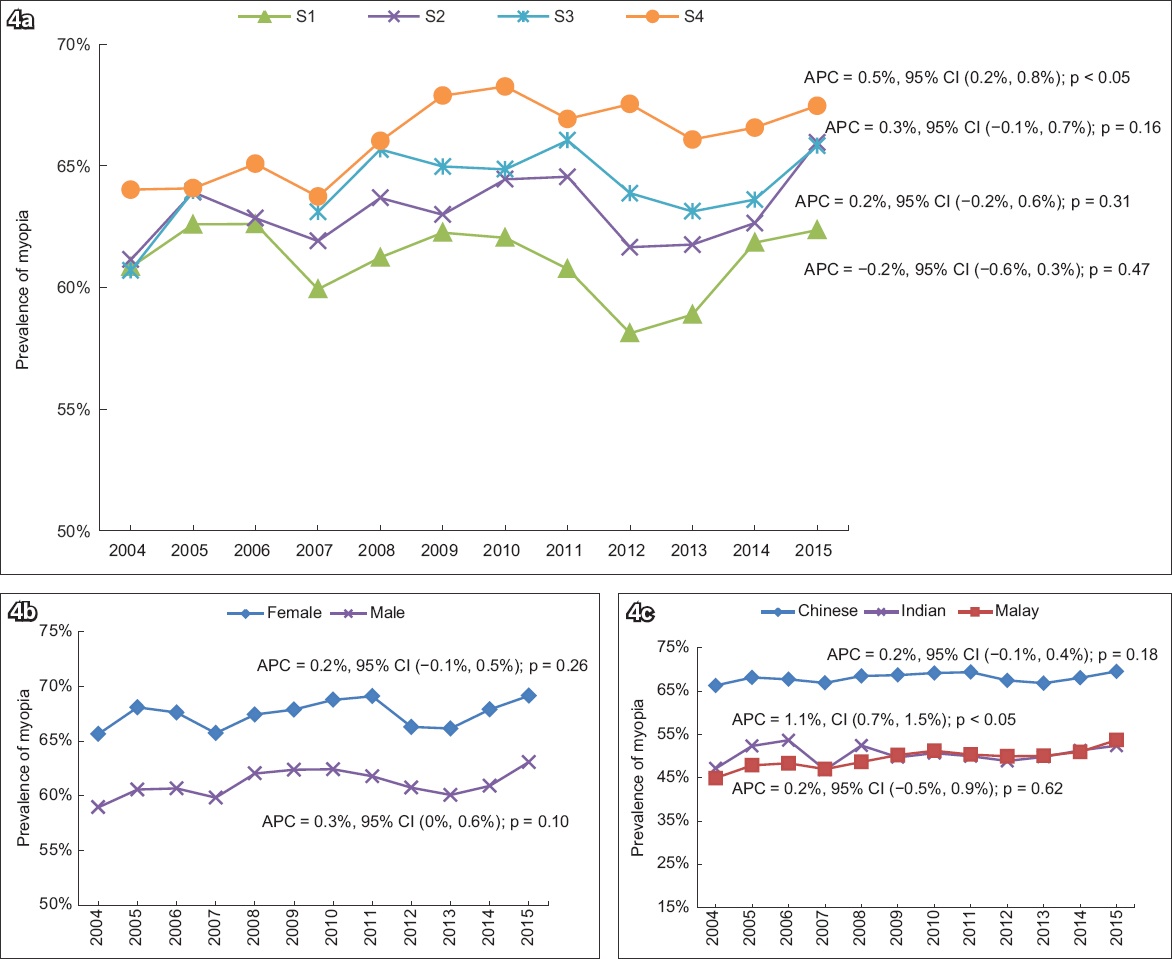
Fig. 4
Charts show the prevalence rate of myopia among secondary school students by (a) educational level; (b) gender; and (c) ethnicity. APC: annual percentage change; CI: confidence interval; S: secondary
DISCUSSION
Among the potential environmental and behavioural risk factors for myopia and myopia progression, the factors most commonly reported to be lacking are exposure to green spaces, exposure to natural daylight, outdoor time and physical activity, together with an excess of near-work activities in children. In a recent meta-analysis, increased time outdoors was shown to be effective in preventing the onset of myopia and in slowing the myopic shift in refractive errors; however, it was not shown to be effective in slowing progression in eyes that were already myopic.(21) More specifically, increase in exposure to green spaces at home, at school and during commuting was associated with a decrease in spectacles use among primary school students in Spain.(22) Increase in playing time in green spaces was associated with a reduction in the risk of spectacles use in longitudinal analysis.(22) Lack of daylight exposure, specifically, has been shown to lead to myopia progression.(23,24) Sporting activity was shown to be preventive against myopia progression, while near work and computer work could be risk factors for myopia progression if children spent at least three hours a day on these outside of school-related work.(22)
Among primary school students, female students were found to have higher rates of myopia in each year except for 2015, when rates among male students were higher for the first time (
We found that Chinese students in Singapore had the highest rates of myopia. Similarly, Rudnicka et al reported in 2016 that East Asians had the highest prevalence of myopia, reaching 69.0% at 15 years of age (vs. 86.2% among Singaporean Chinese). Blacks in Africa had the lowest prevalence of 5.5% at 15 years of age.(27) Time trends in myopia prevalence over the last decade were weak in whites but increased by 23% in East Asians, with a smaller increase among South Asians.(27)
An overall downward trend in myopia prevalence was observed between 2004 and 2015 among primary school students from the 12 sentinel schools; however, no decrease in prevalence rates was seen among the corresponding secondary school students (
Nevertheless, because age of myopia onset and duration of myopia progression are the most important predictors of high myopia in later childhood in myopic children,(2) it is encouraging that myopia prevalence has decreased among primary school students. Furthermore, the students from the 12 sentinel primary schools had the same routine school-based vision screening and NMPP-driven targeted vision care education, and received the same interventions when needed as students at other primary schools, making it reasonable to generalise that myopia prevalence has decreased among primary school students in Singapore. The additional step of obtaining lensometer readings for children wearing spectacles is not expected to change the behaviour of primary school students during routine screening in a way that affects the degree of myopia.
As with similar analyses involving data obtained during routine screening without a control group, the improvement in myopia prevalence cannot be definitively attributed to the SHS initiatives alone. Yet the pervasive nature of the school programmes and public education using mass media did not made it practically possible to have a control group. It would also have been unethical to exclude young children from vision screening, which is a basic component of child health programmes across most middle-income and higher-income countries. Data from this sentinel population of students remains critically useful for reliable quantification of the prevalence of the problem of myopia among children and youths, and allows for ongoing and new public health interventions to be fine-tuned and introduced, respectively.
In conjunction with public health programmes, a locally developed mobile application called ‘Plano’ has been established to manage the use of smartphones and tablets among children, and can be another fun and innovative way to institute good eye care habits. The application can be installed in a handheld device and runs in the background, tracking face-to-screen distance, screen time, device-free activities and even poor posture. All these basic functions are available for free, with additional plans available for a fee. The child is incentivised to adopt the right habits through points and rewarded with outdoor activity, which has been shown to be protective against myopia. With the rapidly growing reliance on smartphones and tablets in learning and day-to-day living in Singapore, this is an especially practical additional approach.
CONCLUSION
Myopia is a complex, multifactorial condition influenced by both genetic and environmental factors. By 2050, almost half of the world’s population is expected to be myopic. This paper aimed to elucidate the public health steps taken in Singapore to combat this problem, report on the myopia prevalence rates between 2004 and 2015 among students in Singapore, and discuss the environmental factors that can potentially be modified through public health programmes. More studies are necessary to further our understanding of the causes of myopia.
ACKNOWLEDGEMENTS
We would like to acknowledge Prof Saw Seang Mei and her research fellow, Carla Lanca, from the Saw Swee Hock School of Public Health, National University of Singapore, Singapore, for assisting in the literature search.


