Abstract
INTRODUCTION
Physical inactivity is a global challenge and physicians must promote physical activity (PA) among their patients. Nevertheless, PA counselling remains inadequate due to limitations in knowledge, education and information availability. This study evaluates the understanding of PA as a health intervention and knowledge of World Health Organization (WHO) guidelines among Singapore and United Kingdom (UK) medical students, the next generation of physicians.
METHODS
Students from Singapore (Yong Loo Lin School of Medicine and Lee Kong Chian School of Medicine) and the UK (Universities of Cardiff, Leicester, Oxford and Birmingham) were invited to complete a 12-item online survey. Questions assessed knowledge of WHO guidelines, understanding of PA in health and illness, personal PA levels and exposure to PA counselling in clinical practice.
RESULTS
Among 633 Singapore and UK students who completed the questionnaire, 94.8% believed that PA was important in preventing disease, but only 70.9% recognised its importance in treating disease. The majority (85.3%) indicated participation in PA and exercise. General understanding of WHO guidelines for adults was poor, with less than half (46.8%) correctly answering this section. 3 (0.5%) students identified that PA in adults could be accumulated in multiple ways. Understanding of PA in health and familiarity with guidelines did not differ significantly between Singapore and UK students.
CONCLUSION
There is considerable room for improvement in the knowledge of WHO guidelines and the role of PA in health. Education should begin during the undergraduate phase so that future doctors are better equipped to counsel their patients.
INTRODUCTION
Physical activity (PA) is essential in maintaining good health. There is substantial evidence that regular PA is effective in the primary and secondary management of chronic conditions such as obesity,(1) hypertension,(2) diabetes mellitus,(3,4) osteoporosis(5,6) and mental illnesses.(7) Conversely, physical inactivity and low fitness have been identified as a significant risk factor for premature mortality.(8) Given the importance of PA, it is worrying that one in five adults globally are reported to be physically inactive, with higher prevalence among wealthier countries as well as women and the elderly.(9) Physical inactivity has thus become a major health problem and was identified by the World Health Organization (WHO) as one of the top five risk factors for global mortality.(10)
In Singapore, a National Health Survey conducted by the Ministry of Health revealed that 60.9% of Singapore residents (aged 18-69 years) engaged in sufficient PA.(11) To combat the problem of physical inactivity among Singaporeans, the Health Promotion Board established generic PA guidelines as well as those aimed at preventing weight gain and obesity among two specific population groups: adults (aged 19-49 years) and older adults (aged ≥ 50 years old).(12) These guidelines were formulated to support various stakeholders involved in health and PA promotion, one category of which includes healthcare providers. In particular, it was recommended that they “talk routinely to… patients about incorporating [PA] into their lives”.
Meanwhile, self-reported data from the United Kingdom (UK) shows that less than half of adults met the recommended levels of PA in 2011; this ranged from 23% (Welsh women) to 43% (Scottish men) depending on the gender and home country of the individual.(13) Across the country, approaches to increasing PA are similar and draw on the influence of primary care professionals. Examples of these include screening tools such as the general practice physical activity questionnaire, or GPPAQ;(14) a behavioural change intervention programme known as ‘Let’s Get Moving’;(15) and public health guidelines by the National Institute for Health and Care Excellence.(16)
The healthcare setting provides an ideal platform for promoting PA and professionals such as physicians are in a unique position to do so, mainly because they are considered experts in this field and are privy to a patient’s background and social setting. Large numbers of doctor visits are made annually within Singapore and the UK,(17,18) allowing for opportune PA promotion to the public. Indeed, a 2012 review that examined trials of PA promotion in primary care showed promising results, where at 12 months after the intervention, PA levels of sedentary adults were found to be significantly increased.(19)
However, various obstacles within the healthcare system continue to hinder PA promotion. One study found that practitioners, despite believing in its importance, were “uncertain about the effectiveness of their counselling and [felt] uncomfortable in providing detailed advice”.(20) Other barriers reported in the same study included a lack of knowledge, training, education and information, as well as the perception of PA advising as a secondary task. Another study examining factors that optimise the delivery and impact of PA counselling found that data on counselling training for practitioners was sparse, with many saying that they lack knowledge and skill for PA counselling.(21) Therefore, training medical professionals is an essential component of the broader strategy in PA promotion. This problem, however, appears to stem from an early stage in a doctor’s training – several studies highlight the paucity of sports and exercise medicine teaching in the official curriculum,(22,23) as well as limited knowledge about PA and its role in health among medical students.(24) In line with the current challenges of PA promotion in healthcare and the lack of information regarding the level of sports and exercise medicine training at medical schools, it is necessary to establish how much teaching in undergraduate curricula focuses on PA.
Hence, this study aimed to: (a) evaluate medical students’ knowledge of PA as an intervention for managing various health conditions; (b) determine if medical students are given any formal teaching in discussing exercise with patients; and (c) investigate factors influencing medical students’ confidence levels in PA counselling.
METHODS
A scoping review was conducted to answer the question: ‘What is the current evidence on medical students’ knowledge of WHO guidelines, their skills and confidence in PA as an intervention, and preventative strategy when managing various health conditions?’ To ensure that the search was comprehensive, a Boolean search was conducted using the keywords and synonyms ‘medical students’ OR ‘medical undergraduate’ OR ‘student doctor’ AND ‘physical activity guidelines’ OR ‘exercise prescription’ OR ‘exercise counselling’ using the following online databases: MEDLINE®, PubMed® and Web of Science. The following inclusion criteria for studies were applied during the screening process: (a) the target population was medical students only regardless of study location; (b) PA or exercise prescriptions were examined; and (c) participants’ appreciation, knowledge and formal education teaching of PA were assessed. Articles that were excluded were: (a) not written in English; (b) review articles; and (c) written before 2010, as this was prior to the publication of the WHO guidelines.(10)
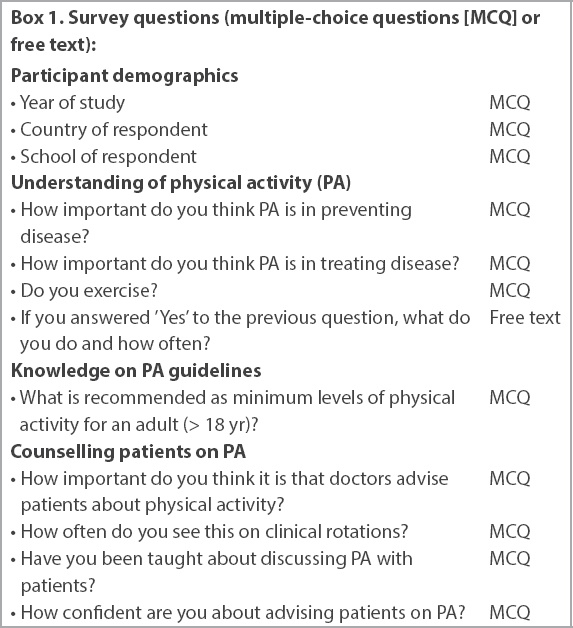
For the survey of students, a 12-item anonymised Google Forms survey was constructed based on previous studies,(22,23,25,26) consisting of two parts (Box 1). The first section collected demographic information about the participants, including the medical school that they were based at and their year of study. The second part focused on whether the medical students exercised, how well they understood international PA guidelines,(10) whether they received any formal teaching in discussing exercise with patients and their confidence levels in counselling patients on PA. Questions were MCQ (multiple-choice questions) or in free text format. All questions needed to be completed for the survey to be considered successfully submitted.
Box 1
Survey questions (multiple-choice questions [MCQ] or free text):
A minimum sample size of 354 was calculated using an online sample size calculator (Raosoft Inc)(27) with the parameters of 5% margin of error, 95% confidence interval, 4,420 population size and 50% response distribution. The survey was sent through email to 4,420 medical students in the mailing lists of two undergraduate medical schools in Singapore and four undergraduate medical schools in the UK from February 2017 to June 2017. Those in Singapore included Yong Loo Lin School of Medicine, National University of Singapore, and Lee Kong Chian School of Medicine, Nanyang Technological University. The four medical schools in the UK included the universities of Cardiff, Leicester, Oxford and Birmingham. The email contained information regarding the purpose of the study and the need for consent to participate. It was made explicit that the survey was not part of any formal assessment for participants and it was reiterated that anonymity would be upheld.
The following inclusion criteria were applied: (a) respondents had to be classified as current undergraduate students in their respective medical schools; and (b) they were fluent in English. Students could be from any year of study. No exclusion criterion was applied as the survey was only shared with medical students. To minimise the risk of selection bias, all students from the respective medical schools were informed in the same email about the purpose of the study, anonymisation, consent information and the link to the Google survey form.
Statistical analysis of the responses was performed using IBM SPSS Statistics version 22.0 (IBM Corp, Armonk, NY, USA). The statistical significance of student beliefs in PA as a primary compared to secondary intervention in health was assessed with McNemar’s test. Chi-square test of independence was used to determine any differences between the responses of Singapore and UK students, and if there was any association between identified contributing factors and confidence in PA counselling. Statistical significance was set at p-value < 0.05.
RESULTS
A total of 180 articles were identified from the online searches (four from MEDLINE, 84 from PubMed and 92 from Web of Science). After 29 duplicates were excluded, titles and abstracts were screened and 19 full-text articles remained for further evaluation. Among these, eight articles focused on PA levels among students to evaluate the link between self-reported PA and knowledge of PA, five examined only PA teaching in medical schools but not the students’ knowledge, and two had an unrelated focus. Hence, only four articles(22,23,25,26) were deemed suitable as background material for the study proposal (
Fig. 1
Flowchart shows the search process for the scoping review.
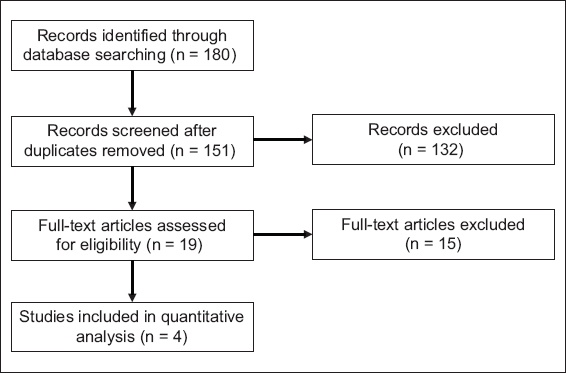
All four articles had been produced after the WHO guidelines(10) on recommended PA levels had been published and all focused on medical undergraduates (
Table I
Findings from the scoping review.
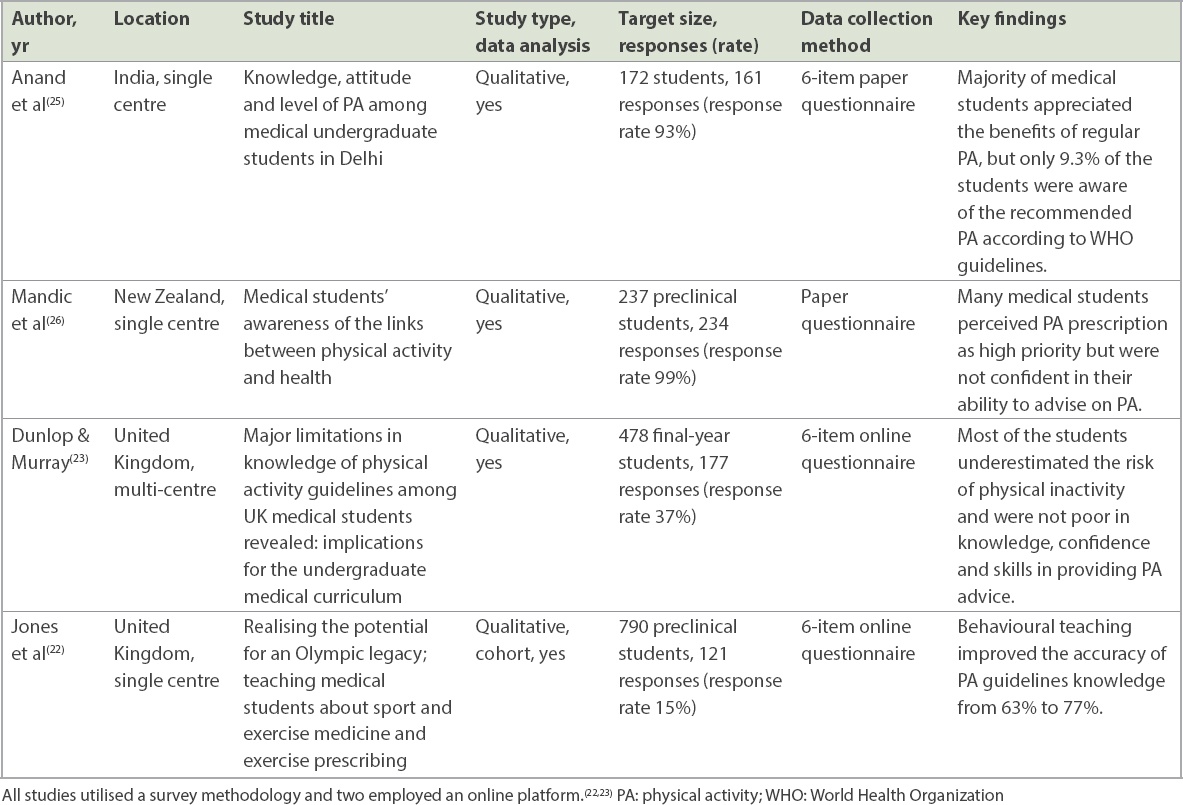
Anand et al(25) reported that while students appreciated why PA is important in health, their knowledge of the WHO guidelines and exercise prescription was low. Yet this was unexpected, as the students were approximately midway through their course and were therefore likely to have received training in this area. Additionally, this question on the WHO guidelines and exercise prescription was one among others that examined different aspects of PA, and thus the students may have overlooked its true meaning. The authors did not discuss why this disparity between appreciation and knowledge existed, but other authors have speculated that it is due to inadequate formal education on this subject.
In contrast to the earlier study, Jones et al(22) and Dunlop and Murray(23) highlighted that despite a paucity of knowledge about PA as a significant risk factor for health, over 60% of UK students were able to recall the WHO guidelines. In the latter study, questions about PA were included alongside those asking about other chronic conditions, while in the former, the questions focused on PA. The participation rate of both studies presents a challenge when drawing conclusions: the generalisability of their findings can be questioned given the response rate of 37% from two Scottish medical schools(23) and an even lower rate of 15% from one UK medical school.(22) Nevertheless, both had a clear methodology of data collection and analysis that we could draw upon for the present study.
Mandic et al’s study,(26) which examined PA among medical undergraduates in New Zealand, had considerably more participants with 234 third-year students and a 99% response rate. Most students (79%) recognised PA as an important intervention, yet only 37% felt confident discussing this with patients; however, confidence was greater among students who exercised regularly. While the larger population provides more reliable information about this cohort, little is known about other year-groups or universities in New Zealand. Attributes such as knowledge, attitude and competence may also vary based on the stage of medical training. Moreover, curricula and teaching may differ across universities. Thus, while methods are adaptable, results are limited without another institution or students from different year-groups for comparison.
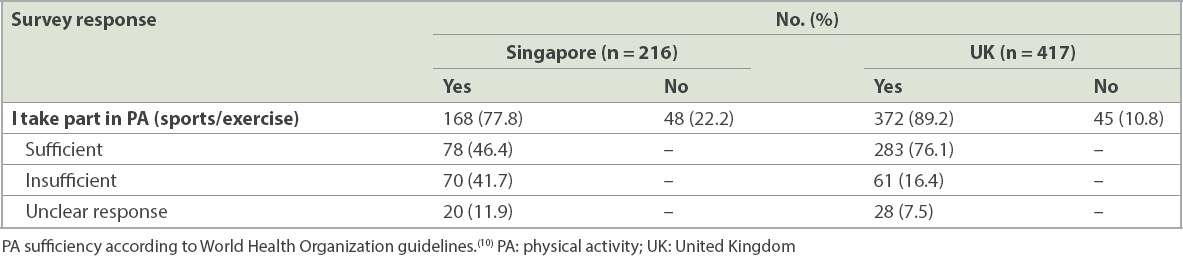
Our survey was sent to 4,420 medical students, 633 (14.3%) of whom responded over the eight-month data collection period. Percentages of first, second, third, fourth and fifth year students were 23.1%, 24.3%, 22.0%, 18.2% and 12.5%, respectively. 34.1% of the respondents were from Singapore, while the other 65.9% were from the UK. Most respondents said that they participated in PA, comprising 168 (77.8%) out of 216 students in Singapore and 372 (89.2%) out of 417 students in the UK. Among these, the proportion with sufficient levels of reported PA according to WHO guidelines(10) varied from 46.4% among Singapore students to 76.1% among UK students (
Table II
Self-reported participation in PA among Singapore and UK medical students.
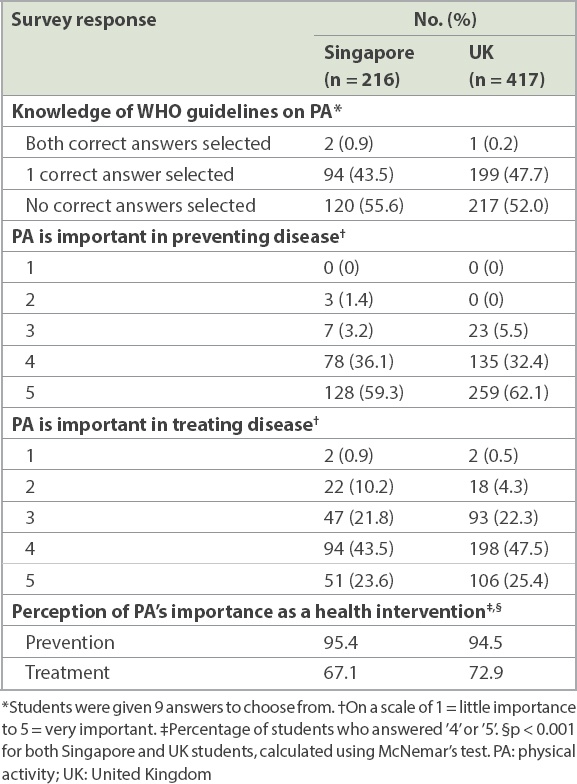
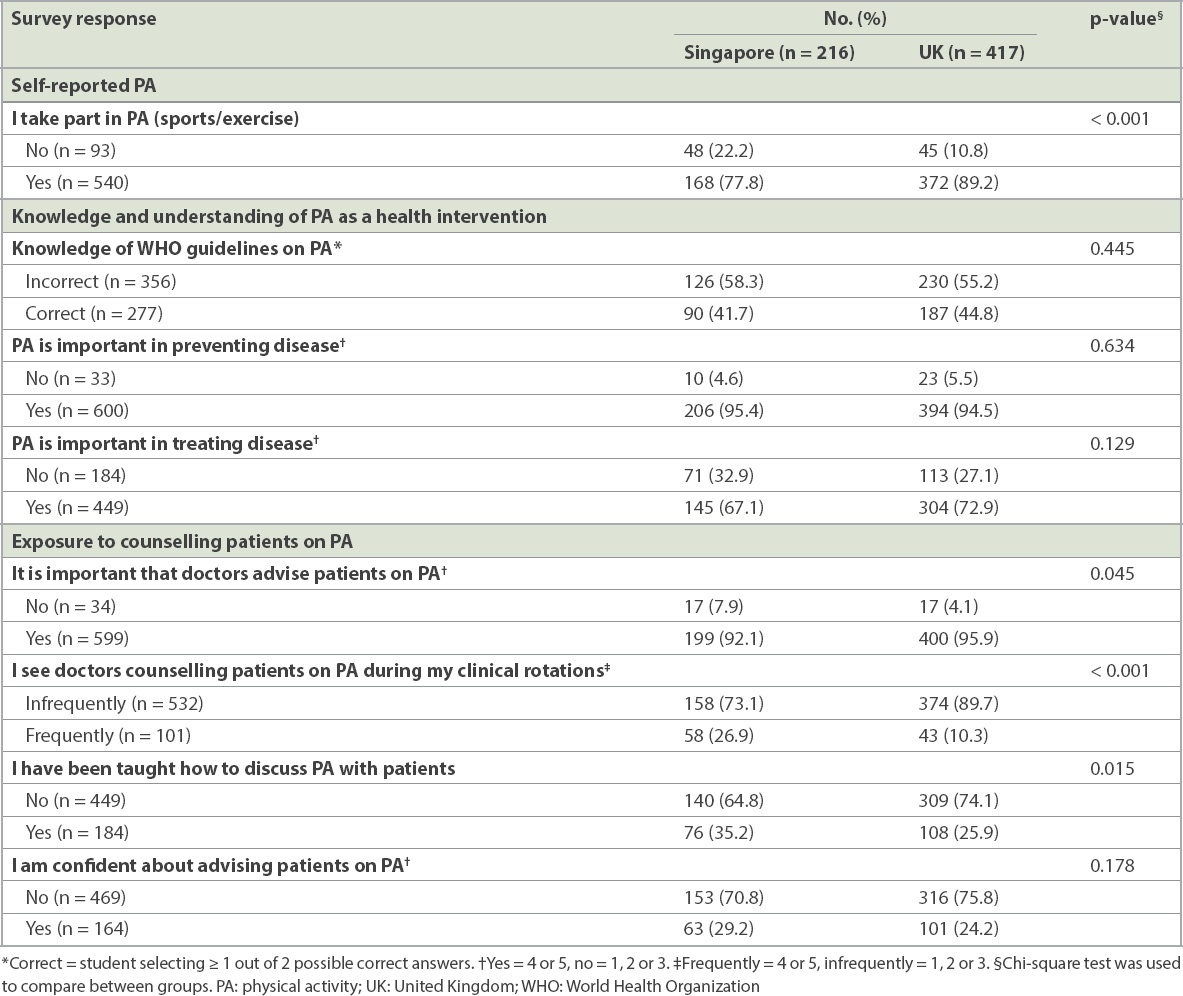
When students were surveyed on their knowledge of WHO guidelines, over 50% of students in both countries (Singapore 55.6%, UK 52.0%) were unable to provide correct responses. Only a small proportion (Singapore 0.9%, UK 0.2%) could identify both correct options (’30 minutes/day, 5 times/week’ and ‘75 minutes/day, 2 times/week’), while the remainder had at least one answer correct (Singapore 43.5%, UK 47.7%). Significantly more students recognised the importance of PA in preventing disease (Singapore 95.4%, UK 94.5%) than in treating disease (Singapore 67.1%, UK 72.9%; p < 0.001 for both countries) (
Fig. 2
Bar chart shows medical students’ knowledge and understanding of physical activity (PA) as a health intervention. *Correct is defined as the student selecting ≥ 1 out of two possible correct answers. Yes = selected 4 or 5, no = selected 1, 2 or 3, where 1 = little importance and 5 = very important.
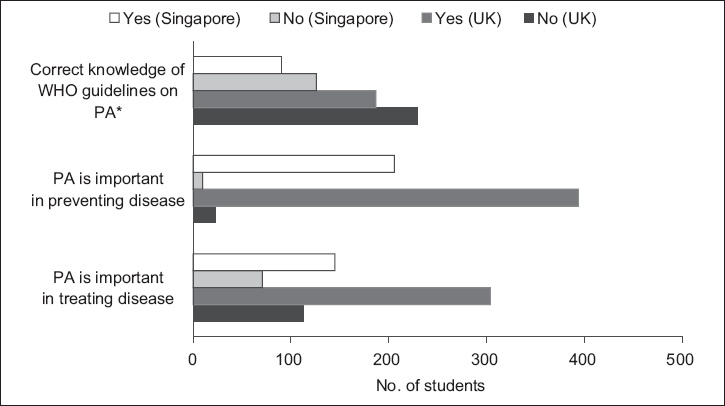
Table III
Understanding of PA and knowledge of PA guidelines among Singapore and UK students.
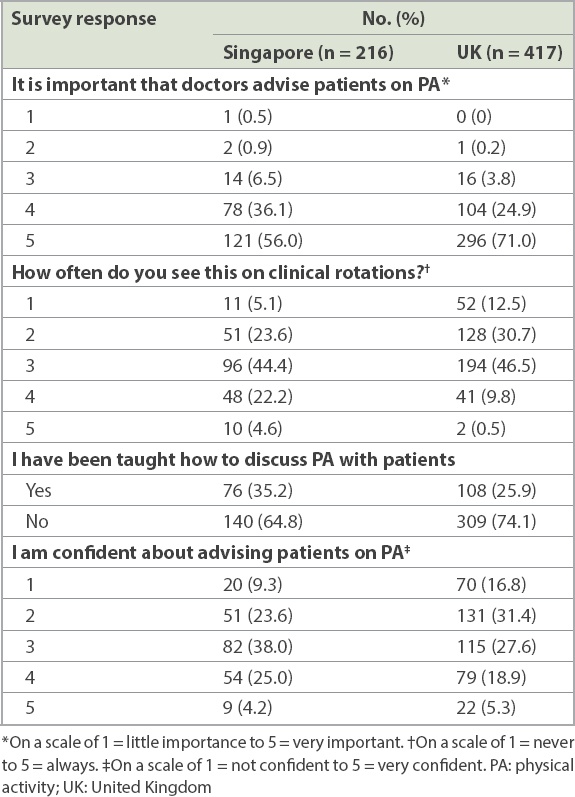
Almost all (Singapore 92.1%, UK 95.9%) medical students believed in the importance of doctors giving patients PA advice, but when it came to observing this during clinical rotations, only 26.8% of Singapore students and 10.3% of UK students witnessed it. In both countries, more than half of students had not been taught about discussing PA with patients (Singapore 64.8%, UK 74.1%). Additionally, most were not confident in their ability to do so (Singapore 70.9%, UK 75.8%) (
Fig. 3
Bar chart shows students’ exposure to counselling patients on physical activity (PA). *Yes = 4 or 5, no = 1, 2 or 3. †Yes = 4 or 5, no = 1, 2 or 3. ‡Yes = 4 or 5, no = 1, 2 or 3. UK: United Kingdom
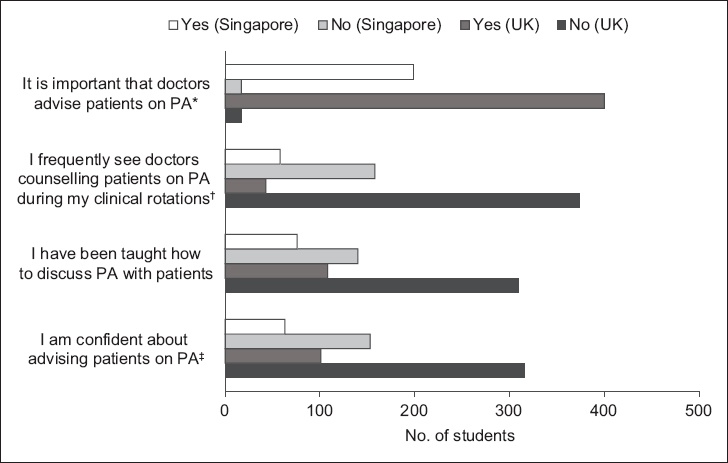
Table IV
Exposure to PA counselling among Singapore and UK students.
When Singapore and UK medical students were compared across various dimensions of PA (
Table V
Comparison between Singapore and UK medical students.
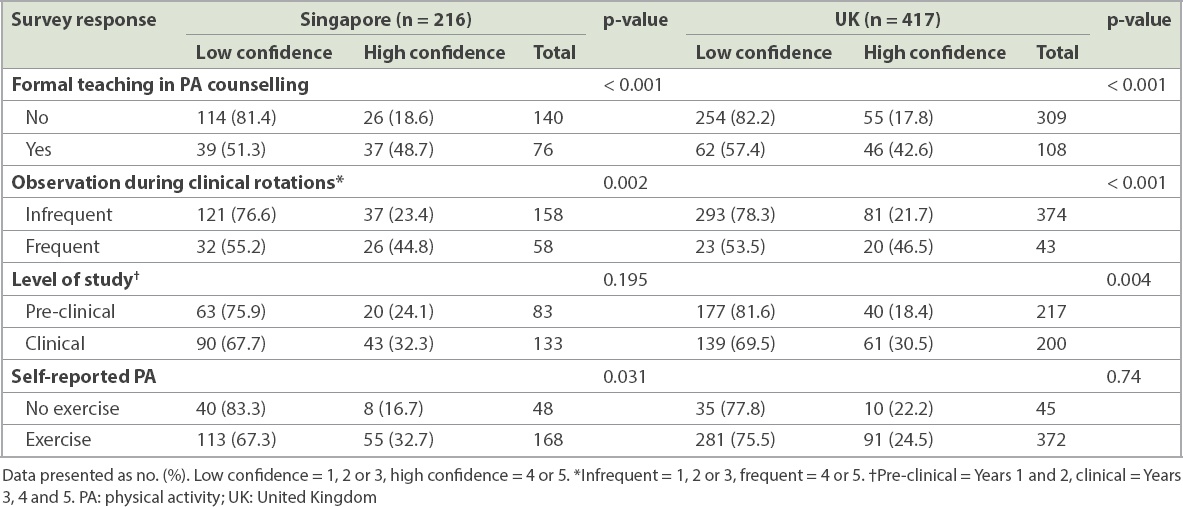
In all, the prevalence of formal teaching about PA was low, and this was more so for UK students compared to Singapore students (25.9% vs. 35.2%, p = 0.015), but confidence in giving patients PA advice was not significantly different for students from both countries (p = 0.178). As shown in
Table VI
Factors influencing confidence levels in PA counselling among Singapore and UK students.
DISCUSSION
PA represents a cornerstone in the management of chronic disease, having been reported to prevent up to 35 chronic conditions(28) and potentially treating at least 26 others.(29) Against a backdrop of the rising non-communicable disease (NCD) burden, the focus on diabetes mellitus in Singapore and global efforts at tackling it,(30) PA’s relevance in modern medicine is likely to increase. To our knowledge, this is the first multi-centre study investigating the teaching, knowledge and beliefs of PA as a health intervention among medical students in Singapore and the UK. In total, there were 633 (14.3%) responses across Singapore and UK medical schools, with medical students from all five years of study being represented. It therefore is indicative of the skills that future doctors will possess in terms of knowledge and skills in PA management.
In all, students from both countries displayed an appreciation of the impact of PA on health. A key finding was the significant difference between students’ perception of PA in prevention and treatment of disease; while more than 90% of students from both countries deemed PA to be essential in primary prevention, fewer in Singapore than the UK (67.1% vs. 72.9%) believed in its importance as a medical treatment. This is perhaps unsurprising because exercise is fundamentally viewed as an activity for healthy people, rather than the chronically ill. More importantly, there remains a limited understanding of exercise prescription, not only in terms of optimising it for specific conditions but also when considering the interaction between exercise physiology and disease pathophysiology.(31)
Nevertheless, PA remains valuable in the management of more commonly encountered diseases in primary care, such as diabetes mellitus(32) and hypertension.(33) Therefore, it is important that students understand and appreciate the role of PA in treating disease so that they are more likely to advocate for it in future. In particular, research by Cho et al(34) demonstrated a positive association between physician perception of exercise as an essential health factor and subsequent advice provision. With this in mind, an approach to educating students about PA in both disease prevention and treatment is a key element to improving rates of PA counselling uptake.
Although students recognised the importance of PA in preventing disease, they displayed limited knowledge of the subject matter with over 50% unable to recall the WHO guidelines. A contributing factor may be the nature of undergraduate medical training, in which a greater focus is often placed on conventional (medical or surgical) treatment as compared to lifestyle modification (such as increasing PA). To illustrate this, Strong et al(35) reported that although 88% of Australian medical schools provided PA education, the time allocated to it over a six-year period averaged only 12.3 hours. Moreover, students are trained to recognise broad principles of management rather than specific details, such as frequency and duration of exercise in this context. With similar responses from both Singapore and UK students, it seems worthwhile to strengthen the emphasis on PA education in both student populations.
Another aim of this study was to determine if medical students are given any formal teaching in discussing PA with patients. In both countries, we found that more than half of students had not been taught to do so (Singapore 64.8%, UK 74.1%). While these numbers are worrying, of greater concern is the suggestion that there is a lack of standardisation in teaching across the schools and that learning about PA was likely to have been opportunistic. By capitalising on the belief that PA is important and by teaching students in a more standardised manner, rates of PA counselling may improve in future clinical practice. Indeed, this was demonstrated by Jones et al,(22) who found that being formally taught had a positive association with a student’s confidence in PA counselling.
Observing the presence of PA counselling during clinical rotations was similarly associated with higher confidence levels for students of both countries. However, once again, few students had the opportunity to see doctors advising patients on PA during their clinical rotations (Singapore 26.9%, UK 10.3%). Not only does this reflect low rates of PA counselling in everyday practice, it could also leave an unfulfilled gap in terms of observational learning. Bandura(36) described five capabilities that all human beings innately possess, among them an ability to learn through observation; this occurs when we watch others’ actions and their consequences and, through that process, learn behaviours. Considering this, a positive feedback cycle could be put into motion whereby observational learning shapes confidence in PA counselling, positively impacting future practice, therefore providing more opportunities for observational learning. Ultimately, this could raise standards of care for patients who require PA as part of the management of their chronic disease, again highlighting the need for students to be familiar with giving patients advice on PA.
Furthermore, past research has highlighted that physicians who are physically active are more likely to provide this form of information to their patients.(37) Among the students surveyed, 77.8% in Singapore and 89.2% in the UK reported that they were physically active, although only 41.7% and 44.8%, respectively, achieved the level in the WHO guidelines. This disparity may be due to lack of knowledge about the requirements for activity to be considered PA. If the issue was poor recall, this is even more concerning, as there is a tendency to overestimate rather than underestimate. Thus, PA in physicians is an issue that must be addressed by medical schools, as it has been well documented that PA levels decline as clinicians progress through their careers.(38,39)
An interesting observation was made regarding self-reported PA: although Singapore students who reportedly exercised regularly had higher confidence levels when advising patients about PA (p = 0.031), there was no significant difference in confidence levels among UK students who took part in PA and those who did not (p = 0.74). This was despite the significantly higher proportion of UK students with self-reported PA that was sufficient according to WHO guidelines (Singapore 46.4%, UK 76.1%). While these findings do not support a consistent link between the PA habits of students and their confidence in giving PA advice, the following observations instead suggest a relationship between personal PA habits and attitudes towards PA counselling. First, significantly more UK students said they took part in PA compared to Singapore students (Singapore 77.8%, UK 89.2%). Concordantly, a significantly higher proportion of UK students held the belief that it was important for doctors to advise patients on PA (Singapore 92.1%, UK 95.9%). Second, a study from the United States found evidence indicating that doctors and medical students who were physically active were also more likely to counsel their patients about the benefits of PA.(40) Third, while Singapore students displayed a positive association between PA habits and confidence in giving PA advice, this may be confounded by the fact that a significantly higher proportion had formal training (Singapore 35.2%, UK 25.9%) and observational learning opportunities (Singapore 26.9%, UK 10.3%). Considering that confidence in PA counselling requires knowledge in the subject matter,(41) this could explain why formal teaching and observational learning had a more consistent influence on confidence levels compared to personal PA habits. Nevertheless, interventions that encourage students to adopt PA are equally important, since the act of giving PA advice reasonably arises from both a positive attitude and confidence in one’s ability to do so.
To the best of our knowledge, this is the first study of its kind in Singapore and the only one to involve students on different continents. While there are some differences in knowledge of WHO guidelines(10) and PA as a tool for health, there are some worrying trends in the lack of formal education and training in PA and exercise. With the epidemic of NCDs internationally as well as in Singapore, future doctors must be empowered when discussing PA with patients. As such, this study is a call to medical educators, practising physicians and future doctors to regard PA as an essential component of medical education rather than a peripheral part of our practice.
While this is the first international multi-centre study comparing PA education in Singapore and the UK, some limitations have been noted that affect the generalisability of our findings. Despite achieving the minimum sample size required, our sample had low response rates and hence might not be representative of the study population, limiting the interpretation of this study.(42) Thus, if this study is repeated, it would be beneficial to try to increase the participation of students and other stakeholders; this may include repeated email reminders to the student cohort and finding opportunities for students to complete paper versions of the questionnaire (e.g. during centralised teaching sessions). A different approach may be required, as the low response rate was also in keeping with previous studies that used online questionnaires.(22,23) Equally, there may have been a self-selection bias among participants, with those who were physically active themselves being more interested in participating in the study. In the future, repeated emails and information dissemination may encourage greater participation from all students and limit this bias.
Another limitation arises from the mode of data collection. Although the online tool increased ease of completion and accessibility to students, it introduces participation bias since respondents may have checked the WHO guidelines while completing the survey. Hence, the study may not have challenged what they already knew. To avoid this, students must be reminded that their participation is voluntary and that results are anonymously evaluated. Although this could not be avoided using our chosen methodology, it may be seen as a positive outcome if students were educated on the current guidelines as a result of participating in the study.
Finally, recall bias may limit the assessment of whether medical students are given formal teaching in PA; as the survey is completed retrospectively, medical students may incorrectly recall whether their learning experiences (and thus knowledge on PA) came from formal teaching sessions. These could be confused with various other encounters, such as informal bedside tutorials, participation in clinics or, most importantly, as a tangential issue during lectures on chronic diseases. Nevertheless, the results demonstrate a lack of teaching throughout undergraduate medical education as well as the potential benefits of learning opportunities. Moreover, this limitation does not impact other aspects of the study, including respondent understanding of PA and factors influencing confidence towards patient counselling.
In conclusion, this is the first international multi-centre study to examine whether medical students have a robust understanding of the role of PA in illness and health as well as their knowledge of WHO guidelines. It highlights a worrying paucity of knowledge in Singapore and the UK, despite the growing burden of NCDs and the need for improved strategies in treatment and prevention of these conditions. These findings should serve as a call to arms for educators, medical schools and policymakers to review our teaching curricula and evaluate our emphasis on preventative medicine, without which this lack of knowledge and understanding is likely to continue. If we do not equip our future generation of doctors with the necessary skills to prevent and optimise NCD management, we would only maintain the status quo of downstream interventions.
ACKNOWLEDGEMENTS
We would like to thank Dr Wang Jiexun, Clinical Research Unit, Khoo Teck Puat Hospital, Singapore, for her statistical advice; Ms Dilys Lee and Ms Eunice Kok (Yong Loo Lin School of Medicine, National University of Singapore, Singapore), Mr Steffan Griffin (Birmingham University, UK), Mr Sam Pickles (Cardiff University, UK), Ms Florence Pickles (Oxford University, UK), and Mr Harry Wilson (Leicester University, UK) for their assistance with distributing the online questionnaire; and all medical students who participated in the survey.


