Dear Sir,
A 73-year-old woman with a past medical history of diabetes mellitus, hypertension and dyslipidaemia presented to an ophthalmologist with a painless decrease in left eye vision. She also had triple vessel coronary artery disease that was treated with medical therapy, as she had declined percutaneous coronary intervention and coronary artery bypass graft surgery. Her long-term medications were: aspirin, valsartan, amlodipine, spironolactone, empaglifloxin, vildagliptin, metformin, NovoMix (long-acting insulin) and rosuvastatin. She was free of cardiac symptoms and was otherwise well prior to the current presentation.
Her unaided visual acuity was 6/45, correctable with pinhole to 6/21, in her left eye. She had a mid-dilated and poorly reactive pupil in the left eye. Slit-lamp examination revealed fine vessels coursing along the left iris surface in an irregular path directed radially towards the anterior chamber angle (
Fig. 1
(a) Photograph of the left iris shows fine vessels (arrows) coursing along the surface in an irregular path directed radially towards the anterior chamber angle. (b) Angiogram shows a severe (90%) non-calcified stenosis (arrow) of the left internal carotid artery. Note that the artery is non-tortuous.
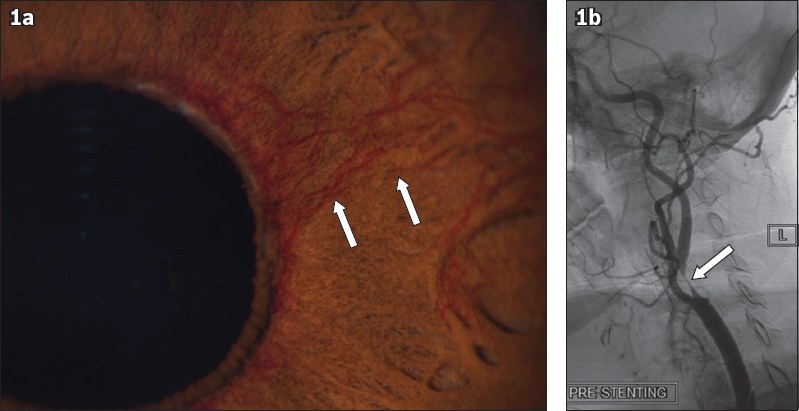
Because of the marked asymmetry of the retinal haemorrhages, the treating ophthalmologist felt that carotid stenosis should be excluded. Thus, the patient was referred to a cardiology clinic for assessment of carotid arteries. Carotid Doppler ultrasonography demonstrated a severe (75%) left internal carotid artery stenosis based on the European Carotid Surgery Trial criteria, suggesting that her presentation was very likely due to ocular ischaemic syndrome. The need for carotid artery revascularisation (carotid endarterectomy vs. carotid artery angioplasty and stenting) and other ophthalmic therapies were discussed with the patient. She decided to undergo carotid revascularisation after being counselled on the risks (including stroke or death) and benefits, as she wanted all potential therapies to preserve vision and prevent unilateral permanent blindness and ocular pain. Owing to her elevated surgical risk (known borderline left main and triple vessel coronary artery disease, short neck and significant obesity), an endovascular approach using carotid angioplasty and stenting was chosen as the revascularisation option.
The procedure was performed in the cardiac catheterisation suite under local anaesthesia via a right femoral arterial access route. Carotid angiography confirmed a severe (90%) non-calcified stenosis of the left internal carotid artery just distal to the carotid bifurcation (
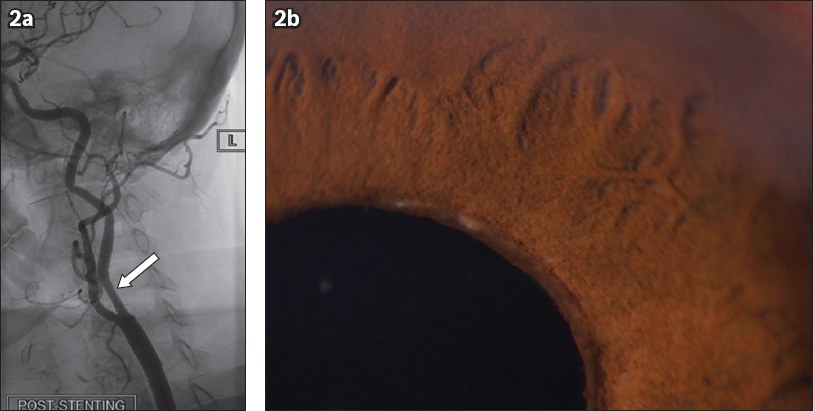
Fig. 2
(a) Angiogram after stenting shows the left internal carotid artery (arrow). (b) Photograph of the left iris after stenting shows resolution of the fine vessels on the surface.
The commonly known presentations of a symptomatic carotid stenosis include clinical stroke, transient ischaemic attack and amaurosis fugax.(1) Carotid revascularisation of a symptomatic severe (> 70%) carotid stenosis has been shown to significantly reduce the likelihood of recurrent cerebrovascular events after the index episode.(2) The data in support of carotid revascularisation of an asymptomatic severe carotid stenosis is less compelling, although the Asymptomatic Carotid Atherosclerosis Study trial suggested modest benefit if the perioperative stroke or death rate is < 3%.(3)
Rubeosis iridis occurs when abnormal new blood vessels develop on the anterior surface of the iris in response to retinal ischaemia, and is associated with conditions such as proliferative diabetic retinopathy, central retinal vein occlusion, ocular ischaemic syndrome (OIS) and chronic retinal detachment.(4) In a small minority (5%) of patients with carotid stenosis, rubeosis iridis from OIS can occur,(4-6) and may be the first and only clinical manifestation of a severe carotid artery stenosis.(7-9) Because many of these patients also have underlying diabetes mellitus with diabetic retinopathy, their OIS may be attributed entirely to diabetic retinopathy and the severe carotid stenosis could be missed. Furthermore, as the vast majority (90%) of patients with OIS present with reduced vision, visual disturbance or eye pain,(4,5) without the usual signs of a symptomatic carotid stenosis (i.e. stroke, transient ischaemic attack or amaurosis fugax), they may also be mistakenly labelled as having asymptomatic carotid stenosis.
A 90% or greater stenosis of the ipsilateral carotid artery is usually found in eyes with OIS,(4,10) and in about half of all cases, the artery is 100% occluded.(4) It has been shown that a 90% carotid stenosis reduces the ipsilateral central retinal artery perfusion pressure by about 50%.(4) Atherosclerosis of the carotid artery is by far the commonest cause of OIS; rarely, carotid artery dissection and other inflammatory disorders such as giant cell arteritis may also lead to OIS.(4,10)
OIS occurs more frequently in patients with poor collateral circulation between the internal and external carotid arteries or between both internal carotid arteries.(11) It is encountered more often in men over the age of 50 years with underlying atherosclerosis, and can be bilateral in up to 20% of patients.(8,9)
The optimal treatment of OIS is still uncertain.(12) Carotid endarterectomy may stabilise or improve vision, usually prior to the development of rubeosis iridis (a sign of greater ocular ischaemia), which reduces the likelihood of visual recovery.(4,5) Although visual results after carotid endarterectomy are modest, most authorities recommend that carotid revascularisation be considered for OIS due to severe carotid stenosis.(4,5) Hence, treatment of OIS usually entails a combination of carotid revascularisation, pan-retinal photocoagulation and intravitreal injections of anti-VEGF, although the individual response is variable.(4,5,12) No randomised data is available to determine the importance of each of these therapies. It has been reported that pan-retinal photocoagulation causes regression of rubeosis iridis in only 36% of patients and may not improve vision.(4,5,12) Evidence for intravitreal anti-VEGF is even more sparse,(4,5) and neither targets the underlying carotid stenosis causing OIS. Despite these limitations, data suggests that if OIS is detected and treated early, improvement in vision is possible.(4,5)
In patients with symptomatic (and asymptomatic) carotid stenosis, surgical revascularisation with carotid endarterectomy is currently considered the treatment of choice.(13,14) For patients at high surgical risk (owing to cardiac, pulmonary or anatomic factors), however, revascularisation with carotid artery angioplasty and stenting has been shown to be safer than endarterectomy.(15) Our patient had a fairly discrete, non-calcified severe stenosis in a non-tortuous carotid artery, indicating a low-risk anatomy for carotid stenting.(16,17) Even in elderly patients, with appropriate case selection and facile technique, a < 3% periprocedural stroke or death rate can be achieved.(16,17) Based on these considerations, carotid angioplasty and stenting was selected as the method of revascularisation for our patient. Carotid artery stenting has been shown to normalise disturbed ophthalmic artery flow and improve OIS-related symptoms and signs, although visual improvement occurred only in those without rubeosis iridis;(18,19) however, the studies were small and lacked long-term follow-up.(5)
To the best of our knowledge, this is the first reported case in Singapore in which a patient with OIS due to a severe carotid stenosis was successfully treated with carotid angioplasty and stenting. Together with retinal photocoagulation and intravitreal injections of ranibizumab, complete resolution of the OIS and improvement in visual acuity were achieved despite the presence of rubeosis iridis. This may be one of the few cases reported in the literature where carotid artery stenting improved visual acuity in a patient with rubeosis iridis. Early recognition of rubeosis iridis as a sign of ipsilateral severe carotid stenosis increases the likelihood of an early diagnosis and treatment, which improves the outcome for such patients. Patients with OIS should also be considered for cardiac evaluation, as cardiovascular disease and stroke have been documented to be the leading causes of mortality in these patients.(4,5)
In conclusion, this case serves to illustrate that although the traditionally defined symptomatic carotid stenosis manifests as stroke, transient ischaemic attack or amaurosis fugax, patients can infrequently present with only symptoms and signs due to rubeosis iridis (i.e. OIS). Ophthalmologists recognise the need for carotid screening in such patients. Conversely, physicians managing patients with a severe carotid stenosis should also consider an ophthalmic assessment for them.


