Abstract
In the complex developmental period of puberty, adolescents experience biophysical changes and adapt to societal and cultural expectations of adulthood. Development of their sexuality is an important biopsychosocial change during this period that, when neglected, may result in unmet sexual and reproductive health needs. Patterns of behaviour in adolescence have repercussions across the lifespan. HEADSSS (home, education/employment/eating, activities, drugs, sexuality, sleep, suicide/depression and safety) is a systematic clinical screening tool for use with adolescents. Adolescents may view risk-seeking lifestyle patterns as appropriate behaviours, and physicians can help them recognise the risks and develop less harmful alternatives and strategies. Personal biases should not affect healthcare providers’ duty to respect the rights of adolescents and ability to provide developmentally appropriate care. Healthcare professionals should be familiar with the relevant legal statutes in Singapore and refer suspected sexual abuse or violence, risk of self-harm, teenage pregnancy, newly diagnosed sexual transmitted infections or multiple risk-seeking behaviours for further evaluation and help.
Emma, a 17-year-old student, arrived at your clinic with her boyfriend. It was her first visit to your clinic and you sensed that she was feeling anxious and afraid. She did not remember when her last menstrual period was, but was otherwise well. She asked you for emergency oral contraception.
WHAT IS SEXUALITY IN TEENAGERS?
In the complex developmental period of puberty, adolescents experience biophysical changes and adapt themselves to societal and cultural expectations of adulthood. Development of their sexuality is an important biopsychosocial development during this period that, when neglected, may result in unmet sexual and reproductive health needs.
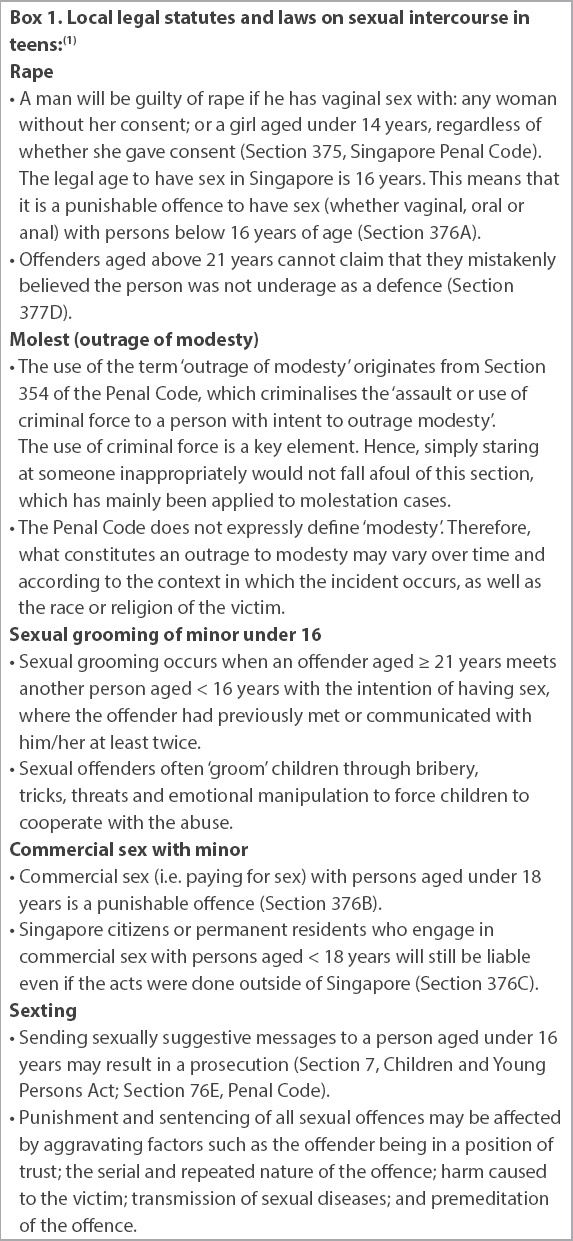
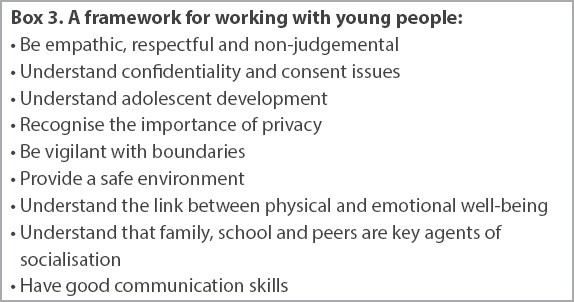
Primary care doctors meet adolescents in the clinic for other acute ailments. Those with a good grasp of the important clinical, legal, social, cultural and educational implications surrounding adolescent sexuality can proactively screen and advise adolescents on their sexual and reproductive health, regardless of sexual activity or marital status. Family doctors can also play an important role as a trusted member of our society in providing adolescents with accurate information about the law, and societal and cultural norms on sexuality. Hence, primary care physicians need to be aware of Singapore’s laws on underage sexual activity and its consequences (
HOW RELEVANT IS THIS TO MY PRACTICE?
We need to prioritise adolescent sexual and reproductive health because unplanned pregnancy and sexually transmitted infections (STIs) are an important cause of adolescent morbidity. The burden of sexual ill health is not trivial in the local population. In Singapore, the proportion of young people aged 10–19 years diagnosed with an STI has increased by 8% from 2014 to 2015, with the ages 15–19 years accounting for more than 90% of the cases.(2)
Patterns of behaviour in adolescence have repercussions across the lifespan. Singapore’s efforts in sexual health education have helped to reduce (unplanned) teenage pregnancies and raise educational achievements in women, which have a major impact on future child health outcomes. Teen pregnancy rates in Singapore were reported to be the lowest in 25 years, with only 359 babies born to women aged 19 years and below in 2015.(3) According to the United Nations Convention on the Rights of the Child, ‘child’ refers to anyone below the age of 18 years unless, under the law applicable to the child, majority is attained earlier. This is the same definition used locally for consultations and referrals to different healthcare institutions.
WHAT CAN I DO IN MY PRACTICE?
Taking a teenager’s sexual health history is not routine for a physiologically oriented healthcare provider within a clinical setting and often does not feature in the list of interview skills that healthcare providers learn. Healthcare providers seeing adolescents should be willing to take a developmentally appropriate psychosocial screen and assessment. HEADSSS, a screening tool to screen for and assess risks, can be used for all adolescents (
Box 2
HEADSSS comprehensive adolescent psychosocial screening interview:
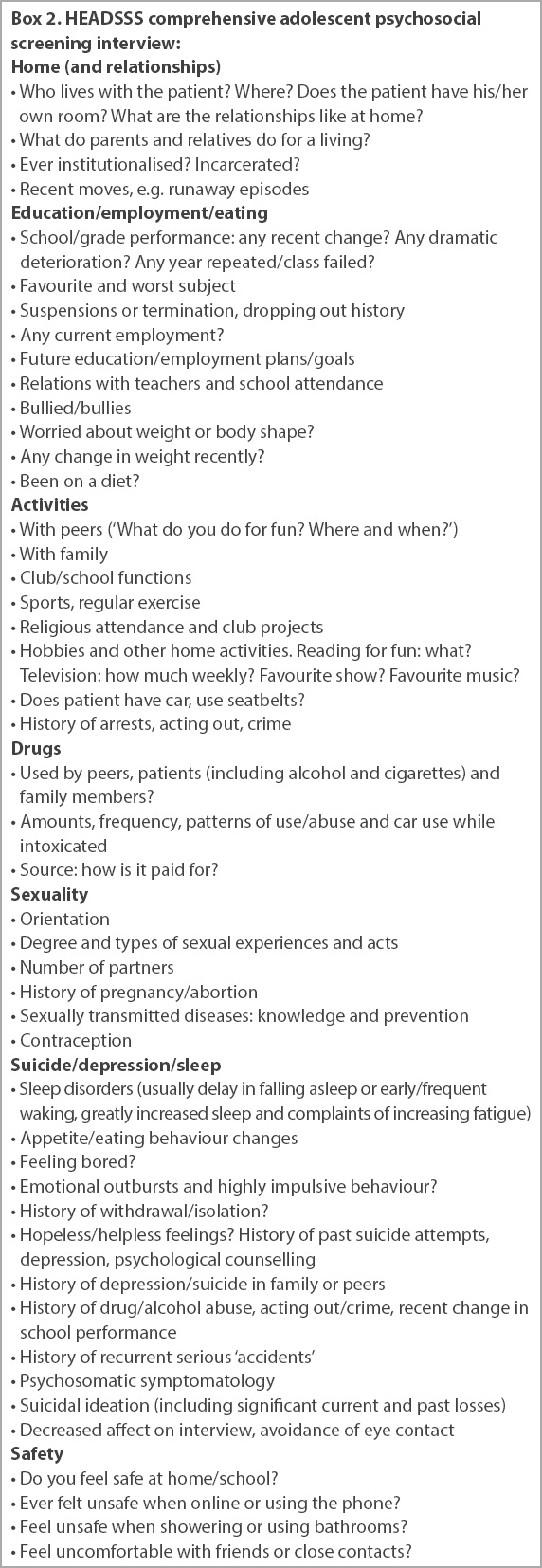
Before the interview
Ensure trust
To engage the young patient in the consultation process, having trust and confidence in the doctor, clinic and the healthcare system is crucial. If the teenagers do not feel that they can confide in doctors or key people in the system, their issues will stay hidden. Providing a safe environment to discuss and confide in the healthcare professional is the first step towards helping them (
Box 3
A framework for working with young people:
Belief systems
It is important to recognise that the healthcare provider’s own set of beliefs, based on one’s knowledge, experience and level of tolerance in dealing with particular situations, will set the standard in providing developmentally appropriate healthcare to youth.(5)
Assumptions
Based on particular individual belief systems, many of us have some assumptions about young people; for example, that they live in a home with two parents, that they go to school and get along with peers and teachers, and that they are heterosexual. As healthcare professionals, it is important to ask non-judgemental questions in a respectful manner and not to assume.
Starting the interview
When starting the interview, physicians should (a) set the stage by introducing yourself to the youth and the parents or caregivers (when present). You should also introduce yourself to the young person first. (b) Ask either the teenager and/or parents to explain their understanding of confidentiality or confidential healthcare. (c) After the youth have given their views, acknowledge their responses and add your views accordingly, explaining and listing the exceptions to confidentiality.
Wrapping up the interview
When ending interviews with teenagers, you can:
Ask them to sum up their life in one word or to give the overall ‘weather report’ for their life.
Ask them to tell you whom they can trust and confide in if there are problems in their lives, and why they trust that person. This is especially important if you have not already identified a trusted adult in the family.
Give them an opportunity to express any concerns you have not covered.
For teenagers who demonstrate significant risk factors, relate your concerns. Ask if they are willing to change or are interested in learning more about ways to deal with their problems. This leads to a discussion of potential follow-up and therapeutic interventions. Many adolescents do not recognise dangerous lifestyle patterns because they see their activities as solutions and not problems. Your challenge lies in helping the adolescent to see health risk-taking behaviours as problems and helping to develop better strategies for dealing with them.
If the adolescent’s life is going well, say so. In most cases, you can identify strengths and potential or real weaknesses, and discuss both in order to offer a balanced view.
Ask if there is any information you can provide on any of the topics you have discussed, especially health promotion. Try to provide whatever educational materials young people are interested in.
Ethics in adolescent sexual and reproductive health
Ethical principles of autonomy, beneficence, non-maleficence and justice in adolescent sexual and reproductive health generally deal with confidentiality, consent (i.e. assessment of capacity, Gillick competency and Fraser guidelines), best interest and advocacy (including child protection issues).
Confidentiality
It is not reasonable to expect an adolescent to discuss sensitive and personal information unless confidentiality can be assured. All adolescents and caregivers present (commonly a parent or both parents) should be told about confidentiality at the beginning of the interview.
The right to confidentiality exists independently of the competence to consent to treatment and encourages mutual trust. Exceptions can only be made when there is further risk of harm. For the competent young person, confidentiality should not be kept when there is (a) disclosure of a history of or current sexual abuse; (b) disclosure of current or recent suicidal thoughts or significant self-harming behaviour; and (c) disclosure of homicidal intent. For the incompetent young person, this is any situation in which there is a significant risk of harm to the adolescent or to others.
Confidentiality matters to young people. One-quarter of young people do not trust health professionals to keep their information confidential from their parents, while one-fifth report not sharing important information with doctors because of fear that their parents would find out.(6) Young people (and their parents) would like to discuss more sensitive topics with their doctor, and this exists independently of their competence to consent to treatment.
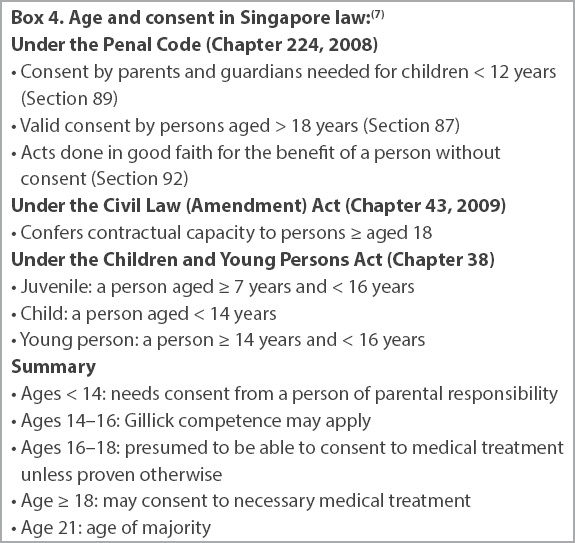
Consent
Autonomy is the ‘capacity to think, decide and act on one’s free initiative’. Every adult has the capacity and competence to decide whether to consent to, or refuse, proposed medical intervention unless it is shown that they cannot understand information presented in a clear way.
Adolescents’ right to make decisions for themselves depends on their ability to do so and is legally defined by their capacity to perform the task in question. Some tasks are age-defined, such as driving a car or buying liquor or cigarettes. The age of consent is termed the age of majority and competence is assumed from persons above this age (21 years in Singapore, 18 years in England). In Singapore, the legal age to enter into a contract is 21 years and to consent to procedures is 18 years. For those aged 16 years and below, Gillick competency (i.e. capacity to consent) can be applied.
Gillick competency and the Fraser guidelines arose from a legal case that looked specifically at whether doctors should be able to give contraceptive advice or treatment to those aged under 16 years without parental consent. Since then, they have been more widely used to help assess whether a child has the maturity to make their own decisions and understand the implications of those decisions. Gillick competency is an objective test of competence that identifies adolescents under the age of 16 years who have the capacity to consent to medical examination and treatment. This is provided that they can demonstrate sufficient maturity and intelligence to understand and appraise the nature and implications of the proposed treatment, including the risks and alternative courses of action. The Fraser guidelines apply specifically to contraceptive advice. They include the necessity of ensuring that the girl understands the advice given to her with respect to contraception, and also concentrate on the desirability of parental involvement and the enhanced risks of unprotected sex.
The general criteria for testing competence is a young person’s ability to: (a) understand simple terms and the nature, purpose and necessity for proposed treatment; (b) understand benefits, risks and alternatives, and the effect of non-treatment; (c) believe that the information applies to them; (d) retain information long enough to make a choice; and (e) make a choice free from pressure.
Best interest and advocacy
Ethically, health professionals have a duty to respect the rights of adolescents provided that the consequence does not result in harm to the adolescent or to others, and the patient’s best interest is paramount. If young people lack the competence to make decisions, a person with parental responsibility has legal power to consent on their behalf, which is in the minor’s best interest. The physician should always respond to their concerns about bullying, abuse, harassment or violence. However, education on violence and abuse prevention issues requires special attention to safe environments, as it may trigger memories of personal abuse or elicit strong emotions of previous loved ones.
Protection and contraception
Among young teenagers and adolescents, some of the perceived barriers towards using contraceptives may include concerns about confidentiality and parental notification, cost of medications and misguided ideas about the risk of getting pregnant and contraindication or effectiveness of contraceptive pills. They may also have certain knowledge deficits on what to do regarding sexual matters and fear of confronting these matters with their parents and healthcare providers.(8,9) Establishing trust and respect with your young teenaged patient, while reassuring her about the confidentiality of the matter is the start of a good doctor-patient relationship. Boundaries and limits of patient confidentiality should be discussed with the patient as well, especially if potential harm may come to her.
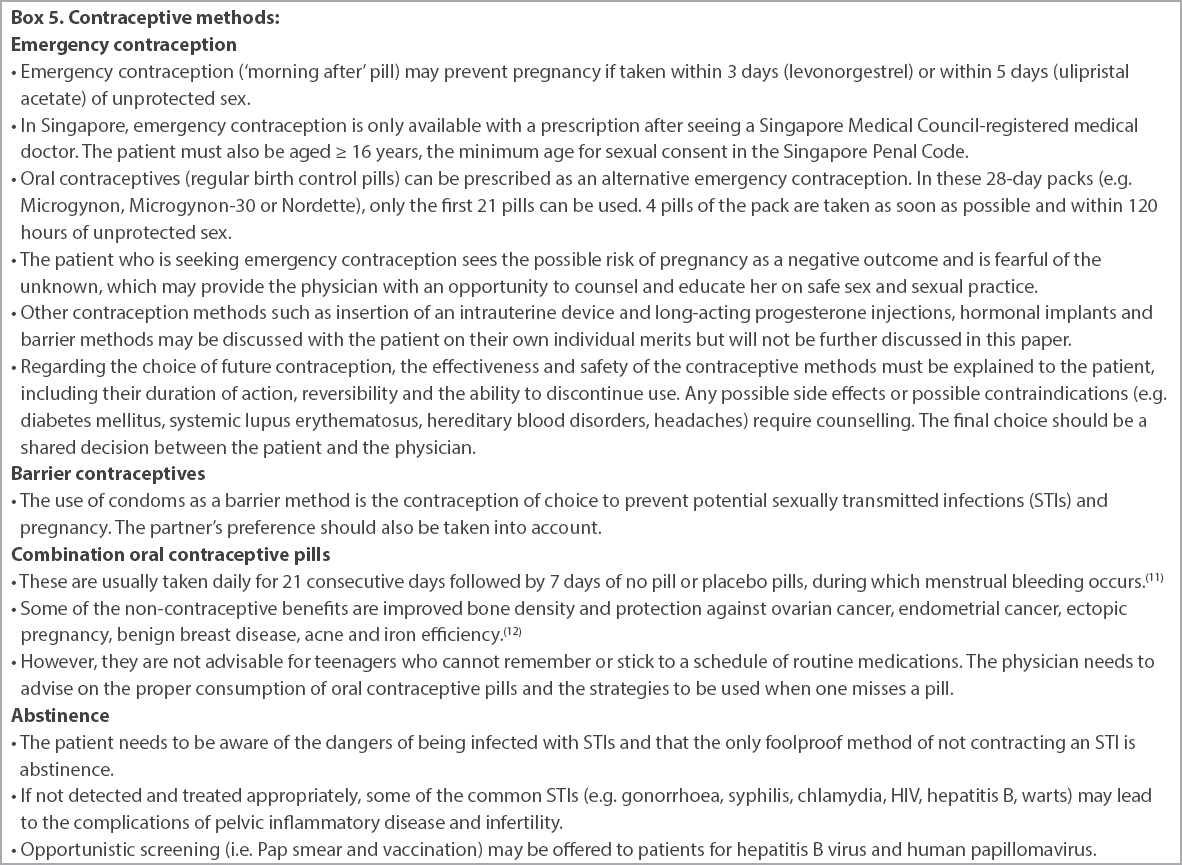
Different types of contraceptive methods are available for adolescents and young teenagers (
Box 5
Contraceptive methods:
Handing off and closing
Finally, the attending doctor must acknowledge that the feeling of sex can be new, exciting and confusing. Patients may get into difficult situations if they are under the influence of alcohol or drugs. Sex that is forced upon a person who does not want to participate is called rape or sexual assault. If the patient does not want sex and is unsure, the partner should respect her decision and stop at once. It is important to postpone sexual activity until patients are emotionally mature and understand that sexual activity affects both the physical and mental health of both parties involved. Patients should be encouraged to speak to a trusted adult or counsellor if they require more information, and a follow-up review should be scheduled in six weeks to review previous matters discussed and any further issues.
The family physician should be sensitive to the patient’s emotions and concerns. If necessary, a colleague of the same gender as the patient can be sought if the patient is not comfortable with discussing certain issues and sharing personal details.
WHEN SHOULD I REFER TO A SPECIALIST?
Patients should be referred to a specialist if there is suspicion of sexual abuse or violence, risk of self-harm, presence of teenage pregnancy, newly diagnosed sexual transmitted infections, or multiple risk-seeking behaviours in a teenager.
TAKE HOME MESSAGES
-
HEADSSS (home, education/employment/eating, activities, drugs, sexuality, sleep, suicide/depression and safety) is a screening tool that can be used to screen for and assess risks in adolescents.
-
Patterns of behaviour in adolescence have repercussions across the lifespan. Adolescent patients may keep their issues hidden if they do not have trust and confidence in their doctor during the consultation in the clinic.
-
The healthcare provider’s own set of beliefs influences the approach to providing the most developmentally appropriate care to the patient.
-
Adolescents may view risk-seeking lifestyle patterns as appropriate behaviours. The clinical challenge lies in helping the adolescent to see health risk-taking behaviours as issues and helping them to develop less harmful alternatives and strategies.
-
Primary care physicians should have a heightened awareness of and always respond to the adolescent’s concerns about bullying, abuse, harassment or violence in a safe environment.
-
In terms of ethics, healthcare professionals have a duty to respect the rights of adolescents, provided that the patient’s best interests are carried out. They should be familiar with the relevant legal statutes under our Penal Code, including sexual grooming of minors and sexting, especially healthcare professionals providing care to adolescents.
You counselled Emma about the side effects of emergency contraception. You also gave her sexual health advice and performed screening for sexually transmitted illnesses, using the Fraser guidelines to assess her competence to consent to contraceptive treatment and receive sexual health advice. You encouraged Emma to speak to a trusted adult or counsellor if she needed more information, and scheduled a follow-up review in six weeks.
SMJ-60-445.pdf