Abstract
We present the revised 2016 Singapore paediatric resuscitation guidelines. The International Liaison Committee on Resuscitation’s Pediatric Taskforce Consensus Statements on Science and Treatment Recommendations, as well as the updated resuscitation guidelines from the American Heart Association and European Resuscitation Council released in October 2015, were debated and discussed by the workgroup. The final recommendations for the Singapore Paediatric Resuscitation Guidelines 2016 were derived after carefully reviewing the current available evidence in the literature and balancing it with local clinical practice.
INTRODUCTION
The national paediatric and neonatal guidelines were last reviewed and released in 2011.(1) For this review and update, in addition to a paediatric resuscitation workgroup, a neonatal workgroup was appointed to review and update our national neonatal resuscitation guidelines. The National Resuscitation Council (NRC) paediatric workgroup comprised representations from the spectrum of our local paediatric community – paediatric intensivists, paediatric anaesthetists and paediatric emergency physicians – from both the public and private healthcare sectors.
In October 2015, consensus statements on science and treatment recommendations (CoSTR) from the Paediatric Taskforce of the International Liaison Committee on Resuscitation (ILCOR) were released.(2-4) The ‘Grading of Recommendations, Assessment, Development and Evaluation’ (GRADE) system(5,6) was adopted by ILCOR for evidence and scientific reviews for the CoSTR statements. Our workgroup reviewed these consensus statements, as well as the relevant body of evidence and literature, when updating our national paediatric guidelines. In addition, the workgroup reviewed and deliberated on the 2015 paediatric guidelines from the American Heart Association (AHA) and the European Resuscitation Council (ERC).(7-10) Important references made in the papers were accessed and reviewed. Other relevant documents and papers, where appropriate and indicated, were also reviewed. The final recommendations for the NRC were derived after carefully reviewing the current available evidence in the literature and balancing these recommendations with local clinical practice. Where appropriate, the existing levels of evidence and classes of recommendations are cited in our recommendations.
DEFINITIONS
A neonate is defined as a patient aged 28 days or less. An infant is a patient aged one year and below. A child is any patient aged one year to puberty. Unless otherwise stated, ‘paediatrics’ in our recommendations refers both to infants and children, but excludes neonates.
MAIN RECOMMENDATIONS
Our main recommendations are divided into four sections: pre-arrest paediatric acute care; basic paediatric life support; advanced paediatric life support; and post-arrest paediatric acute care. Each section consists of sub-sections that are expanded upon in the following paragraphs.
A. PRE-ARREST PAEDIATRIC ACUTE CARE
Paediatric Early Warning Score
In-hospital paediatric cardiac and respiratory arrest can potentially be averted by early recognition and intervention for the deteriorating patient. The use of early warning systems might enable identification of such patients so as to initiate effective interventions promptly. These early warning scoring systems assign numeric scores to specific abnormal observations in several clinical domains. Any effective scoring system must be reliable and reproducible. There must also be an appropriate response when the early warning scoring system identifies critical abnormalities.
At present, there remains a lack of consensus on an accepted paediatric scoring system.(11) The Paediatric Early Warning Score (PEWS), which was first proposed in 2006, has been validated in multicentre studies with high sensitivity and specificity. While early warning scores aid in the detection of deterioration in patients, there is less evidence that they improve clinical outcome. In one observational study, PEWS was associated with a reduction in cardiac arrest rate when used in a single hospital with an established medical emergency team system.(12) There is no evidence that the use of PEWS outside of the paediatric intensive care unit (ICU) setting reduces mortality.(5)
Medical emergency team/rapid response team
Medical emergency and rapid response teams (METs/RRTs) were developed for the urgent assessment of at-risk patients to prevent cardiac or respiratory arrest. These teams may function as the efferent response to the critical afferent early warning score signal.
However, the effectiveness of METs/RRTs in reducing the incidence of cardiac and/or respiratory arrest outside of the ICU setting is inconclusive.(13-15) Most studies demonstrated trends in improving mortality, although they were not statistically significant. The data has been largely observational and was from before-and-after studies, which may have unaccounted or confounding variables.(13-16) Joffe et al(17) demonstrated the potential for risk of bias or confounding variables by comparing the mortality rate at their institution, which did not initiate or organise a MET/RRT, with that of five published studies (all reviewed by ILCOR). The reduction in mortality at Joffe et al’s institution over the same time period was similar to the published results, illustrating the problems of confounding variables and contemporaneous trends. Variables such as the composition of the team, the type of patient, the hospital setting and the confounder of wider ‘system benefit’ complicate objective analyses. In addition, the outcome measures that were traditionally evaluated – respiratory arrests, cardiac arrests and deaths – are exceedingly rare. Thus, finding statistically significant changes in their rates often requires accumulating years of data.
A study at a single paediatric centre found that the implementation of an RRT (inclusive of an early warning score and MET) had a positive impact on the reduction of critical deterioration, “a proximate outcome metric defined as unplanned transfer to the ICU with noninvasive or invasive mechanical ventilation or vasopressor infusion in the 12 hours after transfer.”(16) Studies using a more valid and proximate outcome metric, such as Bonafide et al’s critical decision event,(18) may be better able to answer the question of whether METs/RRTs are truly feasible and effective, before strengthening the case for their implementation in the paediatric inpatient setting. Quality improvement methodology could be used to regulate the impact of a series of changes, which include educational processes, documentation review with feedback systems, and modification of other factors that are thought to improve the delivery of care.
Recommendation
It is reasonable to use PEWS in the in-hospital setting and MET/RRT systems in facilities where children with high-risk illnesses are cared for in general inpatient units (Class IIb, LOE C-LD). It appears rational that intervening earlier in the course of development of a medical emergency provides greater scope for limiting the harmful effects of that condition and promoting recovery. The decision to use a MET/RRT system should, however, be balanced by the institution’s existing resources and capabilities. Training of emergency medical technicians will also need to be addressed so that evidence-based interventions can be brought into play to truncate the deterioration picked up by the early warning systems. Simulation-based MET training exercises have been linked to improved team performance and outcome.(15)
B. BASIC PAEDIATRIC LIFE SUPPORT
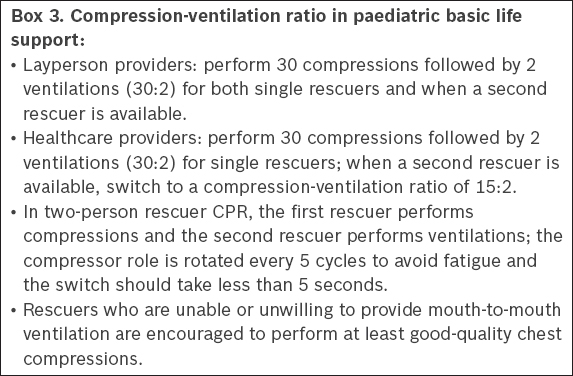
Recognition and assessment of cardiac arrest & initial management of collapse
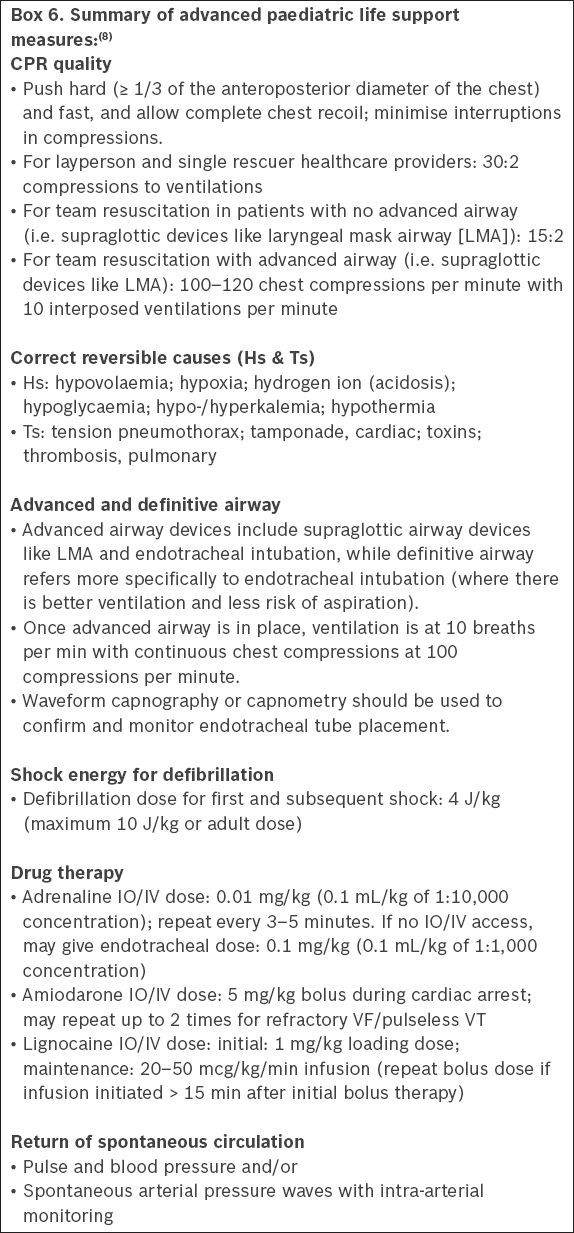
The key aspects for recognition and assessment of cardiac arrest and initial management of collapse in children are listed in
Box 1
Recognition and assessment of cardiac arrest:
Box 2
Initial management of collapse:
There might be some confusion about what A-B-C and C-A-B actually mean and refer to. In the local context, the initial A-B-C refers to opening of the ‘airway’ (A), checking for ‘breathing’ (B) and, if absent, followed by ‘chest compression’ (C), as opposed to other localities, where A-B might refer to ‘providing ventilation’ (e.g. providing five rescue breaths). Following the initial first compression, A-B then refers to opening the airway and providing rescue breaths (i.e. ventilations), followed again by chest compression (C).
There have been discussions about whether one should do chest compressions first before ventilation or vice versa (i.e. C-A-B vs. A-B-C). There is very low-quality evidence that validates performing chest compression before ventilating a patient. Three simulation-based randomised controlled trials (RCTs) – two adult manikin studies and one paediatric manikin study – which were all downgraded for imprecision and very serious indirectness,(19-21) showed a reduced time to first chest compression using the C-A-B approach, as opposed to the A-B-C approach. Data from the three previously cited RCTs showed that time to first chest compression was 18.0–24.3 seconds shorter when using a C-A-B sequence as compared with an A-B-C sequence (15.4–25.0 vs. 36.0–43.4 seconds). Furthermore, data from the two manikin studies showed that time to first ventilation is delayed by only 5.7–6.0 seconds when using a C-A-B sequence as compared with an A-B-C sequence (28.4–43.0 vs. 22.7–37.0 seconds). There are no clinical (human) studies comparing the C-A-B and A-B-C approaches for the initial management of cardiac arrest that address outcomes of return of spontaneous circulation (ROSC), survival to hospital admission, or survival to 180 days with good neurological outcome.
As the only trials to date are manikin studies and the ILCOR paediatric taskforce states that “the confidence in effect estimates is so low that the panel decided a recommendation was too speculative”, the present workgroup decided to maintain our current practice to open the airway, check for breathing and, if absent, start chest compressions (i.e. A-B-C approach).
Recommendation
We recommend that for children, one should first open the airway, check for breathing and, if absent, start chest compressions. One should take not more than ten seconds to determine if there is cardiac arrest. The presence or absence of pulse is not a reliable determinant of cardiac arrest. Other determinants of cardiac arrest are unresponsiveness, gasping, not breathing normally and absence of any signs of life.
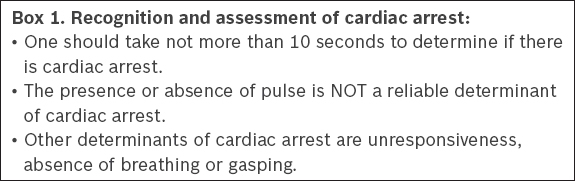
Compression-ventilation ratio
In paediatrics, the usual cause of collapse or acute decompensation is respiratory in nature. It is important to optimally manage the respiration and ventilation of a collapsed child. This is different from a collapsed adult, where there is usually an underlying cardiac/dysrhythmia aetiology, and hence the emphasis on optimal chest compression and the use of defibrillation. The workgroup discussed the merits of adhering to the compression-ventilation ratio of 30:2 as opposed to 15:2 (i.e. having more interposed ventilations with chest compressions).
One should remember that a 30:2 compression-ventilation CPR ratio is more frequently used by a single rescuer in situations where manpower is limited during the acute resuscitation of a collapsed patient. There have not been any new studies specifically addressing the benefits of a 15:2 vs. 30:2 compression-ventilation ratio for CPR in paediatrics. The general move in resuscitation, especially in healthcare settings, has been to perform continuous effective chest compressions and ventilations with advanced airway devices in situ.
While there is no clear evidence that switching compressors every two minutes improves outcomes, many studies have indicated chest compression decay after two minutes of CPR at 30:2.(22,23) However, one must also remember that the oft-quoted two-minute fatigue is derived from studies of trained and seasoned resuscitators. The time to fatigue for laypersons, who are not familiar or well-versed in resuscitation, is likely to be much shorter. In the near future, feedback devices, such as end-tidal carbon dioxide (ETCO2) to guide chest compression quality, may help one to better determine the quality of CPR, although these devices will need to be clinically validated.
Recommendation
For single-rescuer layperson and healthcare providers, we recommend a 30:2 compression-ventilation for children. For healthcare providers with more than one rescuer, we recommend a compression-ventilation ratio of 15:2 when there are no advanced airway devices (i.e. supraglottic devices such as laryngeal mask airway), and continuous chest compressions at 100–120 per minute with interposed ventilations at ten per minute for children with advanced airway devices (see
Box 3
Compression-ventilation ratio in paediatric basic life support:
Chest compression depth
A paediatric (involving patients aged > 1 year) observational study(24) of in-hospital cardiac arrest (IHCA) (89 cardiac arrest events) showed that chest compression depths > 51 mm (> 2 inches) are associated with statistically significant improvement in outcomes (good neurological outcome: relative risk [RR] 3.71; 95% confidence interval [CI] 0.90–15.33; survival to discharge: RR 3.48; 95% CI 1.02–11.84), and better survival to 24 hours (adjusted odds ratio [aOR] 10.3; 95% CI 2.75–38.8; p < 0.001) and ROSC (aOR 4.21; 95% CI 1.34–13.2; p = 0.014). Two paediatric observational studies(25,26) of IHCA and out-of-hospital cardiac arrest (OHCA), with six and nine subjects, respectively, showed that targeting a real-time measured chest compression depth or a subjective anteroposterior diameter during CPR is not associated with a statistically significant difference in outcome (Sutton et al: OR 1.04; 95% CI 0.63–1.71; and Maher et al: RR 6.0; 95% CI 1.00–35.91).
As such, ILCOR suggests that “rescuers compress the chests of infants by at least one-third anteroposterior dimension, or approximately 1.5 inches (4 cm)” and that “rescuers compress the child’s chest by at least one-third of the anteroposterior dimension, or approximately 2 inches (5 cm)”.
Recommendation
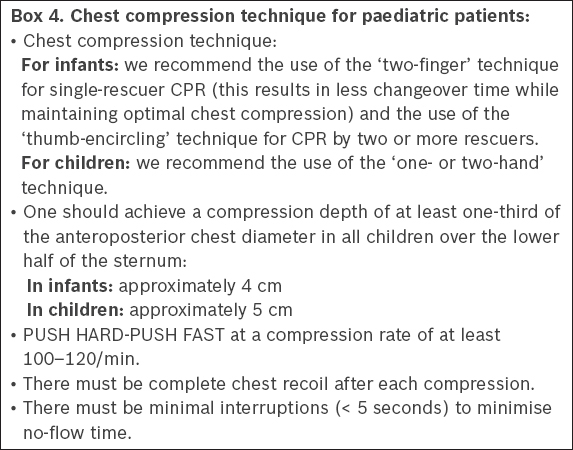
We recommend that the chest compression depth for paediatric CPR should be at least one-third of the anteroposterior diameter for infants and children, or approximately 4 cm to 5 cm, respectively (see
Box 4
Chest compression technique for paediatric patients
Chest compression-only CPR
Two paediatric observational studies(27,28) looked at the critical outcome of 30-day neurologically intact survival in OHCA (n = 5,170; n = 5,056, respectively), comparing the use of compression-only CPR to conventional CPR. Compression-only CPR was associated with worse 30-day neurologically intact survival (RR 0.46; 95% CI 0.34–0.62). Pooled data from the two studies showed no benefit in 30-day neurologically intact survival when comparing the use of bystander compression-only CPR with no bystander CPR (RR 1.21; 95% CI 0.89–1.65). For the important outcome of survival to hospital discharge, no paediatric evidence was identified.
Hence, ILCOR recommends that “rescuers provide rescue breaths and chest compressions for paediatric IHCA and OHCA. If rescuers cannot provide rescue breaths, they should at least perform chest compressions (strong recommendation, low-quality evidence)”. At present, there is, therefore, no evidence to recommend chest compression-only CPR in acute resuscitation of paediatric patients. However, as stated in
Recommendation
We recommend against routine chest compression-only CPR for children. However, rescuers who are unable or unwilling to provide mouth-to-mouth ventilation are encouraged to perform at least good quality chest compressions.
Foreign body airway obstruction (FBAO)
Infants should have chest thrusts to help dislodge the foreign body. Abdominal thrusts (i.e. Heimlich manoeuvre) are not recommended for infants. Children aged ≥ 1 year may be given abdominal thrusts (Heimlich manoeuvre) for FBAO care. The algorithm for paediatric FBAO is summarised in Annex A2.
Use of automated external defibrillator in paediatric cardiac arrest
Since 2005, ILCOR has advocated the early use of automated external defibrillators (AEDs) in children to analyse rhythms and provide defibrillation in cases of cardiac arrest with shockable rhythms.(29,30) When recognised early and rapidly treated, paediatric patients with ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) have a higher survival rate than those with other rhythms.(31-33) AEDs are capable of accurately identifying arrhythmias in children and are unlikely to advise inappropriate shocks.(34,35) For patients aged < 1 year, the incidence of shockable rhythms is very low, except when they suffer from cardiac disease.(36)
Recommendation
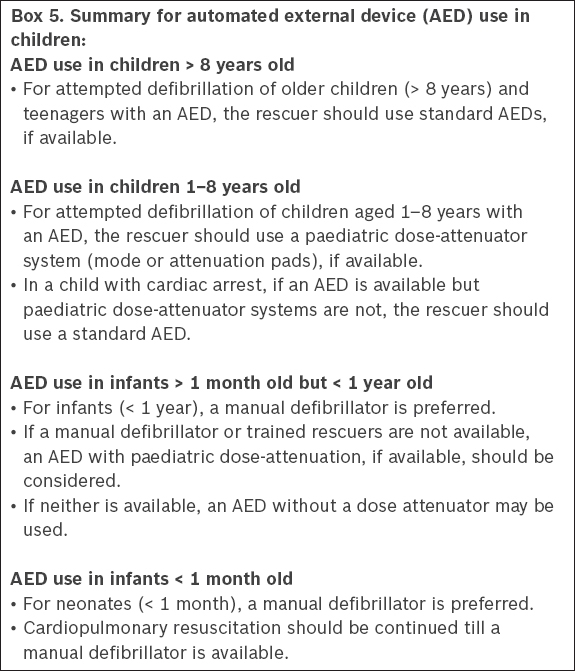
Paediatric dose-attenuating systems can be used in children aged 1–8 years to reduce the energy dose delivered by AEDs.(29-33) This may be done either via a paediatric-specific (attenuated) pad-cable system, or an AED with a paediatric mode or switch, to select for half of the adult energy dose. Most paediatric-specific attenuation pads deliver 50–75 J (see
Box 5
Summary for automated external device (AED) use in children:
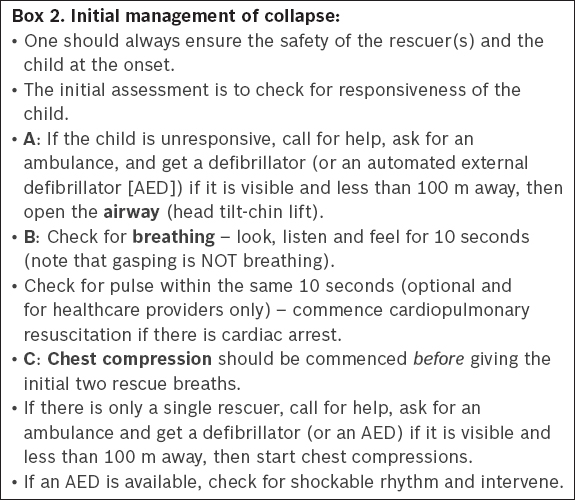
C. ADVANCED PAEDIATRIC LIFE SUPPORT
While pulse check is not recommended for layperson rescuers, healthcare providers may do a pulse check, but this should be carried out during the same ten seconds when the breathing check is being carried out. Pulse should be assessed at the brachial (for infants), femoral (for infants and children) and carotid (for children) arteries.
Newborns that require CPR in any setting should be managed in the same way as newborns in the delivery room, i.e. 3:1 chest compression to ventilation ratio. For infants beyond the neonatal period (i.e. > 28 days of life), CPR should follow the paediatric guidelines, i.e. 30:2 for laypersons and single-rescuer healthcare providers (see
Laryngeal mask airway and supraglottic devices
While paediatric supraglottic devices have been safely used in elective paediatric surgical procedures, their role during emergency situations remains largely consensus-driven.(37) However, early complications are more frequently observed when using supraglottic devices in infants and young children than in adult practice.(38)
Prehospital paediatric resuscitation
Adult OHCA studies have not shown any survival or neurological benefit of bag-valve-mask over the use of supraglottic devices.(39) Observational studies have not found any significant difference in survival among the types of airways used in prehospital paediatric arrest victims(40) or any significant benefits in simulation studies using manikins.(41) In the prehospital environment, based on the limited paediatric literature available, bag-valve-mask should be used for initial airway management. However, if there are issues ventilating a critically ill or collapsed paediatric patient, it is reasonable to use appropriate supraglottic devices, especially laryngeal masks, as a rescue device in conjunction with bag-valve-mask.(37)
In-hospital paediatric resuscitation
While there are no formal high quality studies on supraglottic devices for in-hospital resuscitation of critically ill or collapsed infants and children, supraglottic devices, especially laryngeal mask airways, should be considered for use as rescue airway adjuncts in situations where there is difficulty in intubation and ventilation. Second-generation supraglottic devices may have the added benefits of allowing drainage of gastric contents and facilitation of endotracheal intubation in these situations.(42)
Recommendation
When ventilation is difficult and/or endotracheal intubation is not possible during paediatric resuscitation, appropriate supraglottic airway devices, especially laryngeal mask airways, if available, are recommended when used by experienced providers to provide a patent airway and support ventilation.
Use of atropine for premedication in emergency intubation
Bradycardia may occur during emergency intubation in the paediatric population. The causes are hypoxia, vagal response to laryngoscopy or pharmacological effect of drugs (e.g. succinylcholine). Bradycardia due to hypoxia is rapidly reversed by effective ventilation. Atropine is generally used to prevent reflex bradycardia during emergency intubation. Observational data suggests that the use of atropine for critical care intubation was associated with a reduction in ICU mortality in children over one month old and reduces the prevalence of new arrhythmias during intubation for children older than one month.(43) However, current evidence, based on observational studies, is not robust regarding the routine use of atropine in emergency intubation for preventing bradycardia or cardiac arrest.(44-47)
Recent discussions and studies have also disproved the concept of paradoxical bradycardia below the 0.1 mg dose threshold of atropine.(48,49) Atropine should be administered based on dose-weight requirements, especially for very light-weight premature infants.
Recommendation
Atropine (0.02 mg/kg) may be used as premedication in emergency intubations where there is a risk of bradycardia, e.g. when succinylcholine is used to facilitate intubation. There is no absolute minimum dose of atropine and its dosage should be guided by the weight of the patient.
Fluid management
Fluid management forms a critical part of the resuscitation of a child. When a child shows signs of circulatory compromise caused by reduced circulatory volume or hypovolaemia, controlled volume resuscitation is immediately indicated.(50) However, fluid bolus may not be indicated in children with febrile illness who are not showing signs of reduced circulatory volume or hypovolaemia. A cautious approach to fluid therapy with frequent reassessment of the child is essential.(2-4,51-53) The Fluid Expansion as Supportive Therapy (FEAST) study indicated that, while fluid management is important in paediatric life support, it needs to be judiciously administered.(51,52)
The recommended initial resuscitation fluid of choice in infants and children remains as isotonic crystalloids.(54,55) If the patients show signs of inadequate systemic perfusion, they may benefit from a bolus of 20 mL/kg of an isotonic crystalloid. After each bolus, the child’s clinical status should be reassessed using the ABCDE approach. This is used as a basis to decide if further fluid boluses or other forms of support are required. In some infants and children, early inotropic support may be required.(56,57) Close attention should be given to the patient’s conscious state and respiratory effort, as some patients will require intubation and mechanical ventilation.
Recommendation
Isotonic crystalloids are recommended as initial resuscitation fluid in infants and children with any type of shock. A fluid bolus of 20 mL/kg is used to treat circulatory failure due to hypovolaemia. It is not recommended to give fluid bolus in severe febrile illness when circulatory failure is absent in a child. There should be regular and frequent assessments and reassessments of the child.
Shockable rhythms in paediatric cardiac arrest: VF and pVT defibrillation
VF and pVT may occur in 7%–25% of children with IHCA,(58) and must be immediately treated with defibrillation and good quality CPR. Although it is well accepted that early defibrillation is effective in VF/pVT, the optimal energy dose for safe and effective defibrillation remains to be determined. The evidence available with which to guide defibrillation in children is limited and comes from animal studies, extrapolations from adult data, and historical and recent clinical data. In the 2015 guidelines, the ERC recommends 4 J/kg, while the AHA recommends 2 J/kg for the first shock and 4 J/kg for subsequent shocks.(59-62)
(a) Energy dose
Two small case series demonstrated termination of VF/pVT with either 2 J/kg or 2–4 J/kg. In an observational study on IHCA, Meaney et al(63) reported that a higher initial energy dose of > 3–5 J/kg was less effective than a dose of 1–3 J/kg in achieving ROSC. In a study reporting out-of-hospital paediatric VF, Rossano et al(64) found that such patients often received doses that exceeded the recommended, with no survival to discharge advantage compared with patients who received 2–4 J/kg for initial defibrillation. One observational study of IHCA(58) showed no benefit in achieving ROSC with a specific energy dose for initial defibrillation, but there was a trend of better survival to hospital discharge with a higher mean energy dose per shock (25% with < 2 J/kg, 43.4% with 2–4 J/kg and 50% with > 4 J/kg).
Recommendation
It is reasonable to use an initial and subsequent dose of 4 J/kg of monophasic or biphasic energy for defibrillation (Class IIa, LOE C-LD). For refractory VF, it is reasonable to consider using higher energy levels, not exceeding 10 J/kg or the adult maximum dose (Class IIb, LOE C-LD).
(b) Medications
The 2005 and 2010 guidelines recommended administering amiodarone in preference to lignocaine for the management of refractory VF or pVT. This recommendation was based predominantly on a paediatric case series(65) and extrapolation from adult studies that used short-term outcomes.(66) Valdes et al(67) recently reported that, in their observational cohort study, the use of lignocaine was associated with an increased likelihood of ROSC, as compared with the use of amiodarone or without the use of lignocaine. However, the same study did not show an association between lignocaine or amiodarone use and survival to hospital discharge.
Recommendation
The workgroup has revised the sequence of administering medication from what was recommended in 2011. We recommend that adrenaline be given after the second shock; thereafter, this is alternated with either amiodarone or lignocaine (see algorithm for shockable rhythm in Annex A4).
For shock-refractory VF or pVT, either amiodarone or lignocaine may be used. Amiodarone (5 mg/kg; maximum dose of 300 mg) can be administered intravenously or intraosseously in refractory VF or pVT at the third shock and at every alternate shock (up to a maximum of three doses). Lignocaine may be considered an alternative to amiodarone in refractory VF. If lignocaine is used, an initial bolus of 1 mg/kg (maximum dose of 100 mg) may be given at the third or fifth shock, followed by a maintenance infusion of 20–50 mcg/kg/min. If there is a delay between the initial bolus and the start of infusion by more than 15 minutes, another bolus of 1 mg/kg can be given. Clinicians should choose the drug that they are familiar with, for which they have knowledge of both the expected and unexpected side effects.
ECMO in CPR and paediatric IHCA
The workgroup reviewed the current evidence on the effectiveness of extracorporeal membrane oxygenation (ECMO), also known as extracorporeal cardiopulmonary resuscitation (ECPR) in resuscitation, as compared to conventional CPR alone without the use of ECMO. This is a new area of discussion in the 2015 NRC guidelines that was not addressed in the 2011 guidelines.
The 2010 AHA Pediatric Advanced Life Support (PALS) guidelines suggested that ECPR be considered when dealing with paediatric cardiac arrest refractory to conventional interventions and when the underlying disease process is deemed to be reversible in nature.(60) The 2015 ILCOR systematic review looked at the clinically significant outcomes of survival at 180 days with favourable neurological outcome and survival to hospital discharge.(2-4) Paediatric OHCA was not considered in the 2015 ILCOR systematic review. Current evidence on paediatric ECPR is limited to observational studies and retrospective database reviews. Evidence from cardiac arrest registries(68) and the Extracorporeal Life Support Organisation registry(69) suggests that ECMO can be safely and effectively used in paediatric resuscitation.
To date, there is no controlled paediatric trial comparing ECPR and CPR alone, although unmatched observational series and a propensity-matched analysis of a paediatric inpatient database did not show any overall benefit of ECPR compared to CPR alone in IHCA.(70-73) ECMO, however, was associated with increased complications (e.g. haemorrhage, thrombotic events) and was more resource-intensive.(70) In a retrospective review of a paediatric IHCA registry database, ECPR was shown to improve survival in patients with isolated cardiac disease when CPR alone had failed, especially in surgical cardiac patients.(68,70) The majority of survivors who received ECPR had a favourable neurological outcome.(68,69) In most series, post-arrest ECPR or ECMO were initiated in cardiac patients.(68,71,72,74) When ECPR was initiated in a critical care setting, long-term survival was also reported in children with underlying cardiac disease even after prolonged conventional CPR.(68)
Recommendation
Given current evidence, the NRC workgroup recommends that for paediatric patients with underlying cardiac disease who have IHCA, ECPR may be considered only in settings with the expertise, resources and systems to optimise the use of ECMO during and after resuscitation.
Intra-arrest prognostic factors
For both IHCA and OHCA, the use of predictors of positive patient outcome, such as patient age < 1 year and the initial presence of a shockable rhythm (VF/pVT), should be used to assist prognostic decisions.(40,72,75-85) The taskforce states in the section on the knowledge gap of intra-arrest prognostic factors:(1-3) “Large prospective studies of the association of paediatric cardiac arrest risk factors with outcomes are needed for rescuers to accurately predict successful outcomes and, in particular, to guide decisions on termination of resuscitation.” It also adds: “Studies need to be performed that maintain similar resuscitation protocols to reduce the risk of bias from changing treatment strategies, including post-ROSC care.”
Recommendation
We recommend that predictors of positive patient outcomes, such as patient age < 1 year and the initial presence of a shockable rhythm, should be used to assist in making the prognostic decision during cardiac arrest resuscitation.
Role of ETCO2 and invasive blood pressure monitoring
There is a paucity of scientific evidence regarding ETCO2 monitoring and the role of invasive blood pressure monitoring in advanced paediatric life support.(86,87) For the role of ETCO2 monitoring, the taskforce(2-4) found that “the use of capnography during paediatric cardiac arrest has until now been informed by only animal data and extrapolation from adult observational data”. For invasive blood pressure monitoring, there were only paediatric animal studies to infer from; these showed the benefit of invasive blood pressure monitoring on critical outcomes such as likelihood of survival to discharge, and ROSC.
Recommendation
It is reasonable to use ETCO2 and invasive blood pressure monitoring during cardiac arrest, when available, to guide and optimise resuscitative efforts during paediatric cardiac arrest.
Use of vasopressors during arrest
During arrest, vasopressors can restore spontaneous circulation by improving coronary blood flow and help maintain cerebral perfusion. Conversely, the use of vasopressors can also result in vasoconstriction and increased myocardial oxygen consumption. However, whether its use during arrest actually confers short- or long-term benefits is debatable. Jacobs et al(88) showed improved short-term benefits in adult OHCA patients with the use of adrenaline, in terms of survival to hospital admission and ROSC, but not for longer-term patient outcomes.
Two paediatric out-of-hospital observational studies(89,90) involving 74 patients suggest that the use of vasopressors does not confer certain benefit as compared with non-use of vasopressors in terms of survival with good neurological outcome (Dieckmann et al: RR 2.0; 95% CI 0.50–7.98), as well as survival to hospital discharge and ROSC (Dieckmann et al: RR 1.67; 95% CI 0.82–3.41 and RR 0.95; 95% CI 0.80–1.14, respectively).
Recommendation
It is reasonable to use standard-dose adrenaline for paediatric cardiac arrest management.
D. POST-ARREST PAEDIATRIC ACUTE CARE
Post-cardiac arrest targeted temperature management
The workgroup reviewed evidence for the role of targeted temperature management (TTM) after paediatric cardiac arrest. Data suggests that post-arrest hyperthermia is common in children and associated with poor outcomes.(91)
The 2010 AHA PALS recommendations for targeted temperature control were largely based on extrapolation of adult and neonatal data. In a recent multicentre, prospective trial involving 260 children (aged two days to 18 years) who remained unconscious after OHCA, the children were randomly assigned to either therapeutic hypothermia (target temperature 33.0°C) or therapeutic normothermia (target temperature 36.8°C) within six hours after return of circulation. The primary efficacy outcome was survival at 12 months after cardiac arrest with neurobehavioural scores of ≥ 70 on the Vineland Adaptive Behaviour Scales (VAB-II). TTM was maintained for 120 hours in each group, and those assigned to the therapeutic hypothermia arm were pharmacologically paralysed and targeted temperature of 33.0°C was maintained for 48 hours before slow rewarming over at least 16 hours, to a targeted temperature of 36.8°C. This study found no difference in survival, with good functional outcomes at one year and no complications (e.g. infections, bleeding, serious arrhythmias) in patients treated with therapeutic hypothermia (32.0°C–34.0°C) compared to those treated with normothermia (36.0°C–37.5°C) (27/138 versus 15/122; RR 1.54; 95% CI 0.85–2.76)(92) (moderate quality evidence, downgraded for imprecision).
Observational data from paediatric patients resuscitated from IHCA or OHCA has shown that ICU duration of stay, neurological outcomes and mortality are unchanged with the use of therapeutic hypothermia(93,94) (very low quality evidence, downgraded for bias and imprecision), and therapeutic hypothermia has been associated with the risk of bradycardia and hypotension.(95) Only a small retrospective study of therapeutic hypothermia in survivors of paediatric asphyxia arrest (IHCA and OHCA) showed improvement in mortality at hospital discharge, albeit with no difference in neurological outcomes(96) (very low quality evidence, downgraded for risk of bias and imprecision).
For infants and children successfully resuscitated after IHCA or OHCA, the NRC recommends that TTM be used in the post-cardiac arrest period, and that fever (temperature ≥ 38°C) be aggressively treated after ROSC (Class I). Based on the available data,(2-4) it is reasonable to use either five days of normothermia (36°C–37.5°C), or two days of hypothermia (32°C–34°C), followed by three days of normothermia, in children who remain comatose after OHCA. However, given the paucity of evidence for the role of, and in view of the potential risks associated with, therapeutic hypothermia, the NRC workgroup recommends that normothermia (36°C–37.5°C) be maintained in children who remain comatose after OHCA. In light of the insufficient evidence to recommend cooling over normothermia in children who remain comatose after IHCA, the workgroup recommends maintenance of normothermia (36°C–37.5°C).
Recommendation
We recommend that normothermia (36°C–37.5°C) be maintained in children who remain comatose after OHCA or IHCA.
Post-ROSC ventilation and PO2/PCO2/post-ROSC fluids and inotropes
There are very few studies looking at optimal ventilation strategies post-ROSC in children.
(a) Post-ROSC PO2 targets
Four observational studies(97-100) evaluated post-ROSC normoxaemia or hyperoxaemia in children for the following: survival to hospital discharge with good neurological outcome (Bennett: RR 1.27; 95% CI 0.86–1.90); survival to six months (Guerra-Wallace: RR 1.09; 95% CI 0.81–1.46); survival to hospital discharge (Del Castillo: RR 1.25; 95% CI 0.76–2.05); and survival to paediatric ICU discharge (Ferguson: RR 1.08; 95% CI 0.95–1.23).
Recommendation
In children with ROSC, we recommend supporting ventilation and aiming to achieve 12 breaths per minute (> 8 years old) and 20 breaths per minute (1–8 years old). It is reasonable to measure PaO2 after ROSC, and to target a value appropriate to the specific patient condition and state. In the absence of specific patient data and condition, it is reasonable to target normoxaemia after ROSC. It is also reasonable to use pulse oximetry after ROSC and aim for an oxygen saturation range of 94%–98%.
(b) Post-ROSC PCO2 targets
One paediatric observational study of IHCA and OHCA involved 195 survivors who were observed for at least six hours after arrest. The outcome measured was survival to hospital discharge with favourable/functional neurological outcome (assessed with paediatric cerebral performance category [PCPC 1–2] or no change from baseline before cardiac arrest).(97) Bennett et al found no association between hypercapnia (PaCO2 > 50 mm Hg) and outcome (RR 0.76; 95% CI 0.50–1.16).(97) Conversely, Del Castillo et al’s paediatric observational study(99) of IHCA involving 223 subjects showed that worse outcomes (survival to hospital discharge) were associated with hypercapnia (PaCO2 ≥ 50 mmHg) than with PaCO2 < 50 mmHg (RR 0.48; 95% CI 0.27–0.86).
Both the observational studies of Bennett et al and Del Castillo et al did not show any association between hypocapnia and outcome (survival to hospital discharge with favourable/functional neurological outcome (assessed with PCPC 1–2 or no change with baseline before cardiac arrest, and survival to hospital discharge, respectively – RR 0.70; 95% CI 0.43–1.14 and RR 0.83; 95% CI 0.46–1.51, respectively).
Recommendation
It is reasonable to measure PaCO2 after ROSC and to target a value appropriate to the specific patient condition and state. We suggest that normocapnia is a reasonable target during resuscitation, as both hypo- and hypercapnia have adverse consequences, which are not desirable.
(c) Post-ROSC fluid and inotrope therapy
The issue of optimal post-ROSC fluid and inotrope regime in paediatric patients has only been addressed in observational studies. Topjian et al(101) conducted a paediatric observational study of IHCA and OHCA in 367 children. Patients with systolic blood pressure lower than the fifth percentile for age after ROSC showed worse outcomes, i.e. survival to hospital discharge with good neurological outcome (RR 0.78; 95% CI 0.62–0.99). Two other paediatric observational studies(102,103) of IHCA and OHCA involving a total of 615 children showed worse outcomes (survival to hospital discharge) in patients who experienced hypotension after ROSC. There was significant heterogeneity (I-squared value 0.87), which does not support pooling of data from the aforementioned studies (Topjian: OR 0.62; 95% CI 0.41–0.93; Lin: OR 0.10; 95% CI 0.03–0.32; and Lin: OR 0.07; 95% CI 0.02–0.25).
Recommendation
Post-ROSC, it is reasonable to maintain normal blood pressure that is appropriate for the age of the child through the use of parenteral fluids and/or inotropes or vasopressors. The minimum paediatric systolic blood pressure according to age is as follows:(104-106)
- Term neonates (0–28 days) – 60 mmHg
- Infants (1–12 mth) – 70 mmHg
- Children (1–10 yr) [5th BP percentile] – 70 + (age in yr × 2)
- Children > 10 yr – 90 mmHg
Post-ROSC predictive factors
(a) Post-ROSC EEG
Two paediatric observational studies(107,108) involving a total of 68 patients showed that an electroencephalogram (EEG) (performed within the first seven days after cardiac arrest) that demonstrates a continuous and reactive tracing was associated with a higher likelihood of good neurological outcome at hospital discharge (RR 4.18; 95% CI 2.25–7.75). In comparison, patients with an EEG demonstrating a discontinuous or isoelectric tracing had a higher likelihood of poor neurological outcome at hospital discharge (RR 2.19; 95% CI 1.51–3.77).
Recommendation
It is reasonable to consider the use of an EEG within the first seven days after cardiac arrest to assist in prognostication.
(b) Other post-ROSC predictive factors
The presence of a positive pupillary light reflex post-ROSC suggests good predictive outcomes: from survival up to 180 days with good neurological outcome to survival to hospital discharge with good neurological outcomes.(109) Other observational studies show better outcomes when post-ROSC levels of lactate and neuron-specific enolase or S100B serum levels are lower.(110-112)
Recommendation
It is reasonable to use multiple variables, such as reactivity of pupils and serum markers after cardiac arrest, to predict outcomes for infants and children after cardiac arrest.
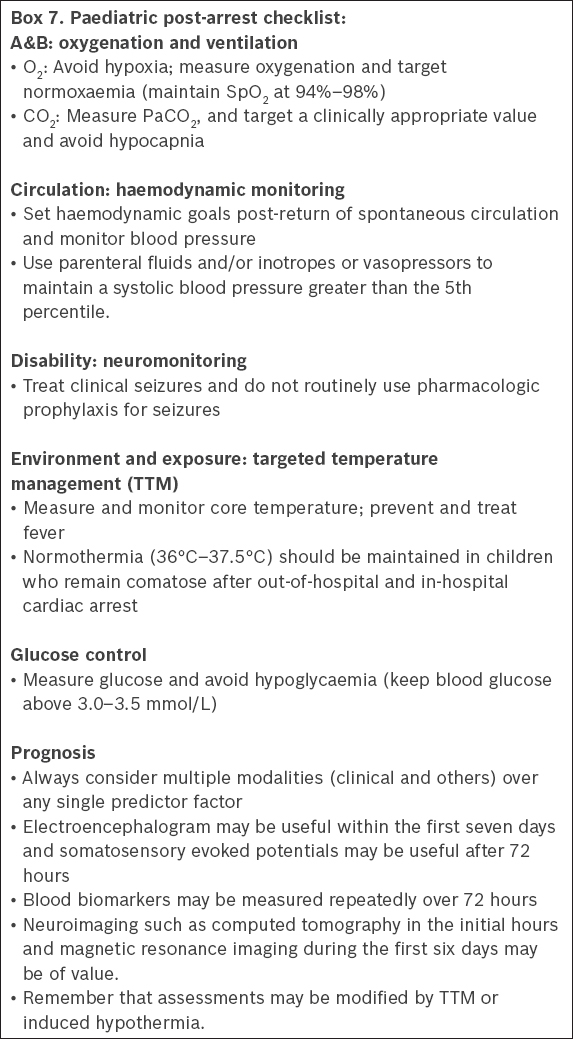
Paediatric post-arrest checklist
The workgroup reviewed the AHA post-arrest checklist(8) and came up with a post-arrest checklist for paediatric resuscitation (
Box 7
Paediatric post-arrest checklist
CONCLUSION
Many of the paediatric recommendations from ILCOR, AHA and ERC have thus far been extrapolated from adult studies and animal models. There currently exists a limited amount of objective scientific paediatric resuscitation evidence. Therefore, more consolidated research needs to be done for paediatric resuscitation. The use of resuscitation registries to capture resuscitation data and concurrent use of feedback devices will help further fine-tune and improve paediatric resuscitation science and practice. For example, the creation of a national and regional paediatric resuscitation registry will help determine the prognostic factors for post-ROSC survival outcomes.
SUMMARY OF RECOMMENDATIONS

ACKNOWLEDGEMENTS
The authors would like to thank Prof V Anantharaman, Chairman of the National Resuscitation Council, and A/Prof Lim Swee Han, Immediate Past President of the Resuscitation Council of Asia, for their invaluable input during the workgroup discussions and in the preparation of this set of recommendations.